In men with high-energy pelvic fracture, careful scrotal examination and review of preoperative imaging are essential, as anterior pelvic approach allow intraoperative correction of traumatic testicular dislocation and prevent long-term complications.
Dr. Aleix Agelet-Pueyo, Department of Orthopaedic Surgery and Traumatology, Hospital Universitari de Bellvitge, Feixa Llarga s/n, 08907 L’Hospitalet de Llobregat, Barcelona, Spain. E-mail: aagelet@bellvitgehospital.cat
Introduction: Testicular dislocation due to trauma is a rare and frequently overlooked consequence of high-energy injuries, particularly those involving pelvic fractures. Early recognition is crucial to prevent complications, such as atrophy, infertility, or persistent discomfort.
Case Report: We present two cases of right testicular dislocation managed intraoperatively during anterior Pfannenstiel approaches for reduction and fixation of unstable pelvic ring fractures (Tile C2 and B3) in male patients following motor vehicle accidents. Preoperative computed tomography scans revealed the ectopic location of the test is within the pelvic cavity. Urologic collaboration was obtained intraoperatively in both cases, allowing manual reduction and fixation by orchidopexy. Definitive fracture stabilization was achieved with anterior plating and iliosacral screws.
Results: Both patients showed good urologic recovery. One developed a superficial wound infection that required surgical debridement, with favorable progression thereafter. Follow-up imaging demonstrated correct fracture consolidation in both cases. These cases underscore the need for systematic scrotal evaluation in male pelvic trauma patients.
Conclusion: Traumatic testicular dislocation, though infrequent, should be considered in the evaluation of patients with pelvic trauma, especially when scrotal abnormalities or ambiguous imaging findings are present. Multidisciplinary management involving orthopedic and urologic teams allows appropriate treatment and reduces long-term risks. When well recognized during diagnosis, surgical correction can be performed effectively.
Keywords: Testicular dislocation, pelvic trauma, orthopedic surgery, orchidopexy, urology, case report.
Traumatic testicular dislocation (TTD) is an uncommon but clinically significant consequence of high-energy blunt trauma, particularly motorcycle or vehicle collisions. Since Claubry first reported the condition in 1818 [1], fewer than 200 cases have been documented [2,3]. Despite its rarity, TTD is likely underdiagnosed, especially in polytrauma patients, where attention is often focused on life-threatening injuries. Pelvic fractures are frequently associated with genitourinary injuries; however, TTD is rarely addressed in orthopedic trauma literature [4,5]. The testis may be displaced into various ectopic sites, such as the inguinal canal, pubic region, or retroperitoneal cavity, often facilitated by a patulous external inguinal ring or vigorous cremasteric reflex [6,7]. Accurate diagnosis hinges on a high index of suspicion and awareness of subtle imaging signs [8,9]. While previous reports have largely emerged from emergency or urologic disciplines, orthopedic involvement – particularly during pelvic fixation procedures – is underrepresented. In some rare instances, closed reduction has been attempted, but success rates are low and carry risks of re-dislocation or missed vascular compromise [10,11]. This article aims to fill that gap by presenting two modern cases of intraoperative TTD identification and correction during anterior pelvic ring fixation, emphasizing diagnostic awareness, operative considerations, and multidisciplinary care.
Two male patients (aged 51 and 40) were admitted following high-energy motor vehicle collisions in 2021 and 2024. Each sustained unstable pelvic ring injuries: One with a Tile C2 (AO 61-C2), and the other with a Tile B3 (AO 61-B3) fracture pattern. Time from injury to surgery was 48 h in both cases. Pre-operative computed tomography (CT) scan revealed right testicular dislocation into the pelvic cavity, anterior to the bladder, identifiable in axial and sagittal views (Figs. 1 and 2). Physical examination noted hemiscrotal asymmetry, but due to the patients’ polytrauma context, findings were not initially prioritized.
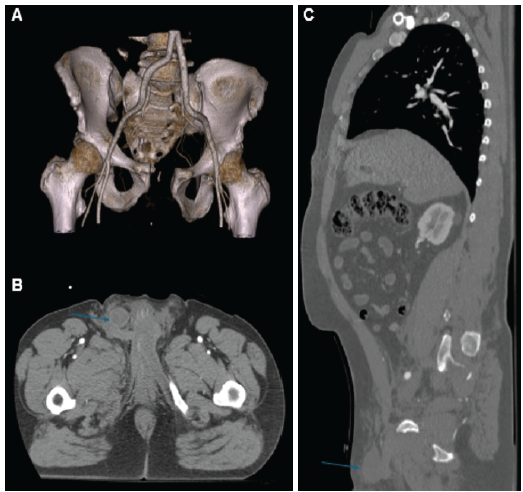
Figure 1: Preoperative computed tomography images from Case 1. (a) Three-dimensional reconstruction showing the pelvic fracture pattern. (b) Coronal view demonstrating migration of the right testicle into the pelvic cavity (indicated by a blue arrow). (c) Sagittal view confirming the presence of the testicle within the pelvic cavity (blue arrow).
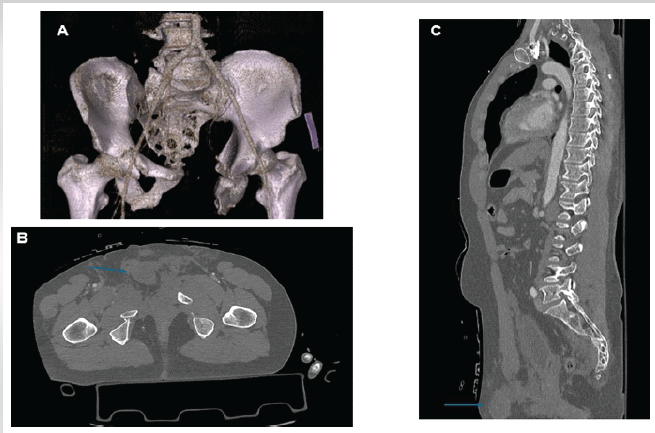
Figure 2: Preoperative computed tomography images from Case 2. (a) Three-dimensional reconstruction of the pelvic ring injury. (b) Coronal view showing intrapelvic displacement of the right testicle (blue arrow). (c) Sagittal view confirming the same finding (blue arrow).
Surgical access was obtained via a Pfannenstiel approach. Intraoperatively, the dislocated testis was encountered in the retropubic space (Fig. 3). Urologic consultation was obtained during the procedure. After confirming vascular viability by direct inspection, the testes were mobilized using blunt dissection, tunneled into the scrotum, and fixed using 3-0 non-absorbable polypropylene sutures. Care was taken to avoid traction or torsion of the spermatic cord.
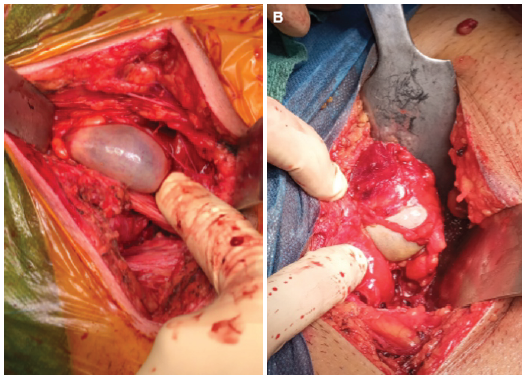
Figure 3: Intraoperative photographs of the right testicle in both cases. (a) Case 1: macroscopic view through a Pfannenstiel approach. (b) Case 2: macroscopic view obtained during surgical exposure through a Pfannenstiel incision.
Pelvic stabilization proceeded with anterior reconstruction plating and percutaneous iliosacral screws (Fig. 4). No intraoperative complications occurred. One patient developed a superficial wound infection requiring debridement. Hospital stay was 9 and 12 days, respectively. At 3- and 6-month follow-up, both patients showed complete radiological union and preserved testicular volume without pain or atrophy.
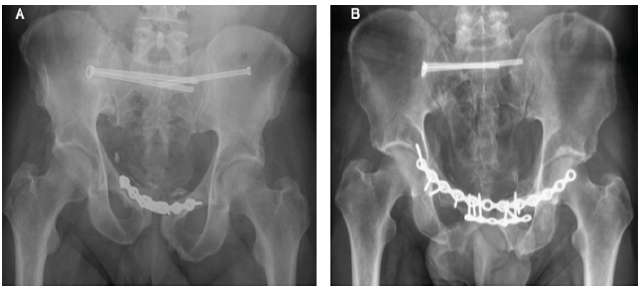
Figure 4: Postoperative pelvic radiographs. (a) Case 1: anteroposterior view showing fixation with a symphyseal plate and bilateral iliosacral screws. (b) Case 2: anteroposterior view after fixation with double anterior plating and right-sided iliosacral screws.
TTD is a rare injury often overshadowed in the setting of polytrauma. Yet its clinical consequences – ranging from chronic pain to infertility – are avoidable with early detection and prompt treatment. TTD typically results from direct or upward blunt force to the scrotum, displacing the test is out of the tunica vaginalis. Reported ectopic sites include the superficial inguinal canal, perineum, and abdominal cavity [2,3]. Anatomical predisposition plays a role, but so does injury mechanism: Motorcycle and car accidents account for most cases [2,4,12]. Diagnosis relies on clinical suspicion and imaging. Physical findings, such as an empty hemiscrotum are easily missed. CT and ultrasonography are essential, yet underused. Our cases reinforce that even when visible on CT, TTD may go unreported unless actively sought [8,9]. Previous authors, including Ko et al., Wiznia et al., and Ezra et al., have similarly emphasized the need for radiological vigilance and accurate triage in pelvic trauma [8,9,13]. The anterior Pfannenstiel approach – commonly used for symphyseal fixation – provides a direct view of the retropubic space and creates an opportunity for intraoperative identification [5,9]. In our series, this allowed successful concurrent orchidopexy. We advocate that during anterior pelvic exposure, surgeons routinely inspect this space for displaced gonadal structures. Technical pearls include blunt dissection around the testis, protection of the cord, and use of non-absorbable suture. Intraoperative Doppler can be considered to confirm viability, though it was not used in our case. Collaboration with urology was key to safe reduction and fixation. Failure to address TTD early can result in long-term damage. Sakamoto et al. reported a case where spermatogenesis resumed 15 years post-bilateral testicle dislocation caused by pelvic trauma, by performing a late orchidopexy [14], but this is an outlier. Most literature – including Middleton, Sehrawat, and O’Brien et al. – shows delayed diagnosis leads to atrophy, infarction, or need for orchiectomy [5,15,16]. Bilateral dislocations, sometimes with unilateral rupture, have also been described and present an even more urgent surgical challenge [17]. In certain pediatric or low-impact cases, conservative management has been attempted [7], but long-term data are lacking. López Alcina et al. and Chiu and Lin provide comprehensive overviews of different management pathways and outcomes [18,19]. We propose trauma protocol updates: Include scrotal inspection in secondary surveys, add testicular position as a standard field in pelvic CT reports, and flag cases for preoperative urology consults. Furthermore, trauma registries should incorporate TTD to better quantify incidence and outcomes. Compared to prior case series, our contribution is unique in combining preoperative CT diagnosis confirmed intraoperative, immediate orthopedic-urologic collaboration, and technical detail of fixation and outcome. These cases serve as a call to action for orthopedic teams to include scrotal content evaluation in pelvic trauma workups.
TTD is a rare but clinically significant injury that may be easily overlooked in the setting of high-energy pelvic trauma. Its timely recognition is essential to prevent long-term complications, such as testicular atrophy, chronic pain, and infertility. These two cases highlight the critical role of orthopedic surgeons not only in pelvic stabilization but also in identifying and managing associated soft-tissue injuries during surgical exposure. Routine inspection of the retropubic space during anterior approaches, particularly when preoperative imaging suggests scrotal abnormalities, provides a valuable opportunity for immediate diagnosis and treatment. Early multidisciplinary collaboration with urology enables safe testicular repositioning and fixation, ensuring favorable functional outcomes. We recommend that orthopedic trauma protocols include systematic scrotal examination and structured imaging review in all male patients with pelvic fractures. Increasing awareness of this rare but relevant entity can improve diagnostic rates, facilitate intraoperative decision-making, and ultimately optimize patient care.
In patients with high-energy pelvic trauma, systematic scrotal assessment and review of preoperative imaging are essential to identify rare testicular dislocation. Intraoperative recognition through anterior approaches allows timely orchidopexy and prevents long-term complications.
References
- 1. Claubry E. Observation of a sudden retraction of both testicles into the abdomen following violent compression of the lower part of the abdominal wall by a cart wheel. J Gen Med Chir Pharm 1818;64:325-30. [Google Scholar] [PubMed]
- 2. Al Saeedi A, Khalil IA, Omran A, Alobaidy A, Al Ansari A. A literature review and two case reports: Is traumatic dislocation of the testes a surgical emergency? Cureus 2022;14:e24672. [Google Scholar] [PubMed]
- 3. De Carvalho NM, Marques AC, De Souza IT, Soares VG, Do Nascimento FG, Pinto LM, et al. Bilateral traumatic testicular dislocation. Case Rep Urol 2018;2018:7162351. [Google Scholar] [PubMed]
- 4. Gómez RG, Storme O, Catalán G, Marchetti P, Djordjevic M. Traumatic testicular dislocation. Int Urol Nephrol 2014;46:1883-7. [Google Scholar] [PubMed]
- 5. Sehrawat S, Sharma V, Srivastava GS, Farooque K. Unilateral traumatic testicular dislocation in a patient of pelvic diastasis and spine fracture in an adult: A case report and review of literature. J Orthop Case Rep 2024;14:99-104. [Google Scholar] [PubMed]
- 6. Feder M, Sacchetti A, Myrick S. Testicular dislocation following minor scrotal trauma. Am J Emerg Med 1991;9:40-2. [Google Scholar] [PubMed]
- 7. Shirono Y, Yamaguchi S, Takahashi E, Terunuma M. Conservative management of bilateral traumatic testicular dislocation in a 10-year-old boy. J Rural Med 2018;13:82-5. [Google Scholar] [PubMed]
- 8. Ko SF, Ng SH, Wan YL, Huang CC, Lee TY, Kung CT, et al. Testicular dislocation: An uncommon and easily overlooked complication of blunt abdominal trauma. Ann Emerg Med 2004;43:371-5. [Google Scholar] [PubMed]
- 9. Wiznia DH, Wang M, Yeon-Kim C, Tomaszewski P, Leslie MP. Traumatic testicular dislocation associated with lateral compression pelvic ring injury and T-shaped acetabulum fracture. Case Rep Orthop 2016;2016:9706392. [Google Scholar] [PubMed]
- 10. Madden JF. Closed reduction of a traumatically dislocated testicle. Acad Emerg Med 1994;1:272-5. [Google Scholar] [PubMed]
- 11. Nagarajan VP, Pranikoff K, Imahori SC, Rabinowitz R. Traumatic dislocation of testis. Urology 1983;22:521-4. [Google Scholar] [PubMed]
- 12. Bromberg W, Wong C, Kurek S, Salim A. Traumatic bilateral testicular dislocation. J Trauma 2003;54:1009-11. [Google Scholar] [PubMed]
- 13. Ezra N, Afari A, Wong J. Pelvic and scrotal trauma: CT and triage of patients. Abdom Imaging 2009;34:541-4. [Google Scholar] [PubMed]
- 14. Sakamoto H, Iwasaki S, Kushima M, Shichijo T, Ogawa Y. Traumatic bilateral testicular dislocation: A recovery of spermatogenesis by orchiopexy 15 years after the onset. Fertil Steril 2008;90:2009.e9-11. [Google Scholar] [PubMed]
- 15. Middleton AH, Martin JM, Wittmann TA, Schmeling GJ. Testicular dislocation after pelvic ring injury: A report of 2 cases. JBJS Case Connect 2019;9:e0141. [Google Scholar] [PubMed]
- 16. O’Brien MF, Collins DA, McElwain JP, Akhtar M, Thornhill JA. Traumatic retrovesical testicular dislocation. J Urol 2004;171:798. [Google Scholar] [PubMed]
- 17. Edson M, Meek JM. Bilateral testicular dislocation with unilateral rupture. J Urol 1979;122:419-20. [Google Scholar] [PubMed]
- 18. López Alcina E, Martín JC, Fuster A, Pérez J, Puertas M, Moreno J. Testicular dislocation: report of two new cases and review of the literature. Actas Urol Esp 2001;25:299-302. [Google Scholar] [PubMed]
- 19. Chiu YC, Lin YK. Traumatic testicular dislocation: A case report and literature review. Medicine (Baltimore) 2022;101:e29137. [Google Scholar] [PubMed]