Optimal graft utilization enables effective single-stage reconstruction of complex multiligament knee injuries while preserving future revision options.
Dr. Rahul Kakran, Department of Orthopaedics, Yashoda Group of Hospitals, Nehru Nagar and Vasundhara, Ghaziabad, Uttar Pradesh, India. E-mail: rahul.kakran@yahoo.com
Introduction: Multiligament knee injuries (MLKIs) are complex injuries associated with significant instability and functional impairment. Surgical management is challenging due to controversies regarding timing, staging, and graft selection, particularly in polytrauma patients.
Case Report: We report the case of a 60-year-old male who sustained a multiligament injury to the right knee following a road traffic accident, involving complete tears of the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and medial patellofemoral ligament (MPFL), with associated meniscal injuries. After ruling out vascular compromise, the patient underwent single-stage arthroscopic reconstruction. The ACL and PCL were reconstructed using peroneus longus tendon grafts, whereas the MCL was repaired and augmented using a semitendinosus graft. The same semitendinosus graft was strategically utilized for concurrent MPFL reconstruction to address recurrent patellar instability.
Results: Postoperatively, the patient demonstrated satisfactory clinical and radiological outcomes, with restoration of knee stability and progressive improvement in range of motion. Follow-up magnetic resonance imaging confirmed intact reconstructed ligaments, and the patient was able to mobilize with a stable knee at short-term follow-up.
Conclusion: This case highlights that single-stage reconstruction with optimal graft utilization, including combined MCL and MPFL reconstruction using a single semitendinosus graft, is a feasible and effective option in complex MLKIs. This approach restores stability while preserving graft options for potential future revision surgery.
Keywords: Multiligament knee injury, single-stage reconstruction, graft optimization, semitendinosus rerouting, medial collateral ligament, medial patellofemoral ligament, peroneus longus graft, case report.
Multiligament knee injuries (MLKIs) are devastating injuries. They are defined as injuries to at least two of the four major ligaments in the knee: Anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), lateral collateral ligament (LCL) (and posterolateral corner) and medial collateral ligament (MCL) (and posteromedial corner) [1]. These injuries are commonly classified using the Schenck classification system [2]. The incidence of these injuries has been reported to be around 0.02–0.20% of all orthopedic injuries [3]. However, this is likely to be an underestimation due to spontaneous knee reduction and missed injuries. The immediate management of these injuries is crucial in identifying and treating any vascular and nerve injury. The literature has shown poor outcomes and residual instability in those who were treated non-operatively [4,5]. However, the optimal surgical treatment for these injuries is not known, with differences in opinion among treating clinicians. There are controversies in the timing of surgery (early vs. delayed), single-staged or two-staged procedures and whether the damaged ligaments should be repaired or reconstructed. Graft selection can be challenging in multiligament knee reconstruction. Surgeons have the option of using autograft, allograft, or synthetic graft. Each of these options has its advantages and disadvantages [6]. The decision on graft choice usually depends on the number of ligaments requiring reconstruction/augmentation, graft availability, surgeon preference and the chosen surgical technique for reconstruction (certain techniques require longer grafts) [6]. Autograft options include hamstring (gracilis and semitendinosus) tendon, bone-patella tendon-bone (BPTB), and quadriceps tendon (with or without a distal bone block) [6]. These grafts can be harvested from the injured knee or from the contralateral knee. Some surgeons prefer to harvest the graft from the uninjured contralateral knee to reduce further insult to the injured knee. Common allografts used in multiligament knee reconstruction include Achilles tendon, extensor mechanism apparatus, BPTB or tibialis anterior tendon. Allograft is expensive and may not be readily available [6,7]. Synthetic grafts such as the ligament augmentation and reconstruction system (LARS) can also be used in multiligament knee reconstruction. Several studies have shown good outcomes with the use of LARS ligaments in acute multiligament knee reconstruction [8,9,10]. This article aims to summarize how we managed multiligament injury patients in one sitting and also maximize the usage of the graft harvested thus in case of revision surgery we still have graft options (quadriceps and patellar tendon) available to us.
A 60-year-old male patient came to us 1 week after an injury to the right knee after a road traffic accident. The knee was swollen, unstable, and painful.
Radiographs of the knee revealed increased medial joint opening with respect to the normal knee joint. (Fig. 1) Local examination of right knee showed increased medial joint space opening with positive valgus stress and posterior sag signs, suggestive of MCL and PCL injuries (Fig. 2).
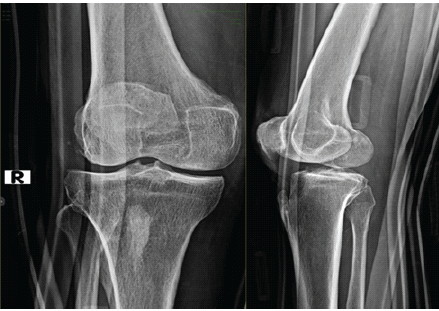
Figure 1: Pre-operative X-ray of right knee showing increased medial joint space opening.

Figure 2: Pre-operative clinical photograph showing positive valgus stress test, suggestive of medial collateral ligament injury, and positive posterior sag sign, suggestive of posterior cruciate ligament injury.
Computed tomography angiography of the right lower limb revealed normal arterial flow.
Magnetic resonance imaging (MRI) scan of the knee revealed a complete tear of the ACL, PCL, MCL, medial patellofemoral ligament (MPFL), and a grade II tear of the body of the medial and lateral meniscus.( Fig. 3)
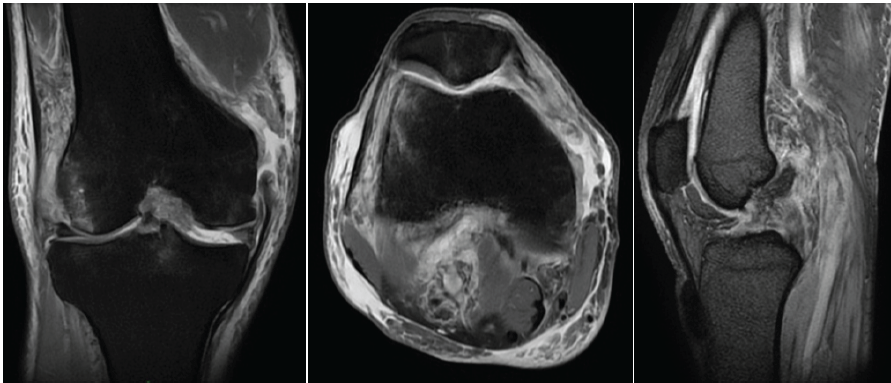
Figure 3: Magnetic resonance imaging of the right knee showing medial collateral ligament tear at the femoral end, anterior cruciate ligament tear, posterior cruciate ligament tear, and medial patellofemoral ligament tear.
There was also an LCL sprain.
Procedure and findings (surgical technique)
The patient was administered spinal anesthesia and positioned supine with the operative limb in leg-on-table position. A pneumatic tourniquet was applied to the proximal thigh. Standard anteromedial and anterolateral arthroscopic portals were established. After thorough lavage and evacuation of hemarthrosis, diagnostic arthroscopy was performed. Arthroscopy revealed complete tears of the ACL and PCL, along with tears involving the body of both medial and lateral menisci. A femoral-side tear of the MCL and MPFL tear were also identified.( Fig. 4)
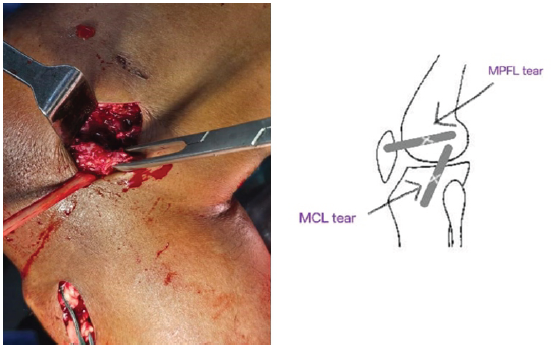
Figure 4: Medial collateral ligament tear identified at the femoral end.
The ACL was reconstructed using the ipsilateral peroneus longus tendon graft. Femoral fixation was achieved using an adjustable rigid loop, and tibial fixation was performed with a Milagro Advance Interference Screw (DePuy).
Subsequently, the PCL was reconstructed using a contralateral peroneus longus tendon graft, fixed on the femoral side with an adjustable rigid loop and on the tibial side with a Milagro Advance Interference Screw (DePuy). Partial meniscectomy of the body of both medial and lateral menisci was performed. Attention was then directed to the MCL. The semitendinosus tendon was harvested using a tendon stripper (Fig. 5). The MCL tear at the femoral attachment was primarily repaired using Ethibond sutures. Augmentation was performed using the semitendinosus graft, which was passed under the sartorius fascia through a tunnel created near the MCL tear site and fixed using a metallic suture anchor (FASTIN-RC, DePuy) placed on the medial aspect of the medial femoral condyle (broad insertion point between adductor tubercle and medial epicondyle – Schöttle’s point) as described by Kakran et al. (Fig. 6).
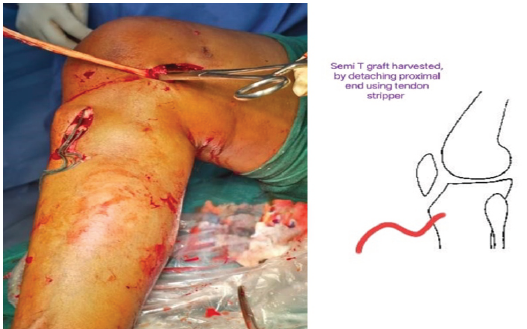
Figure 5: Hamstring graft (semi-tendinosus) was harvested and passed via tunnel near the medial collateral ligament tear technique site – Kakran et al.
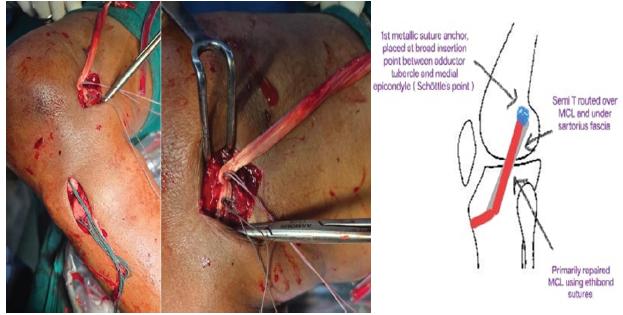
Figure 6: Medial collateral ligament tear repaired using Ethibond sutures and augmentation done via Semi – T graft using metallic (FASTIN-RC) suture anchor – DePuy {Placed on the medial aspect of the medial femoral condyle}– Kakran et al. technique.
The MPFL tear was reconstructed using the same semitendinosus graft, routed in the soft-tissue plane between layer II (retinaculum) and layer III (capsule). Fixation was achieved using a metallic suture anchor (FASTIN-RC, DePuy) placed on the medial aspect of the patella (between the upper 1/3rd and middle 1/3rd of the medial patellar border) in accordance with Kakran et al. technique (Fig. 7).
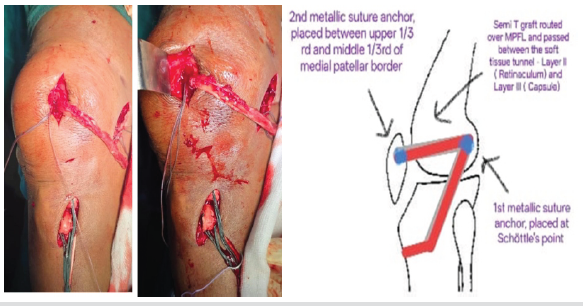
Figure 7: Medial patellofemoral ligament tear identified and reconstructed using metallic (FASTIN RC) suture anchor – DePuy {Placed on the medial aspect of the patella}– Kakran et al. technique.
Final graft tensioning was performed, and knee stability was assessed through a full range of motion. Hemostasis was secured, wounds were closed in layers, a sterile dressing was applied, and the tourniquet was released.
Immediate Post-op X-ray of right knee was done which showed stable fixation and satisfactory alignment. ( Fig. 8)
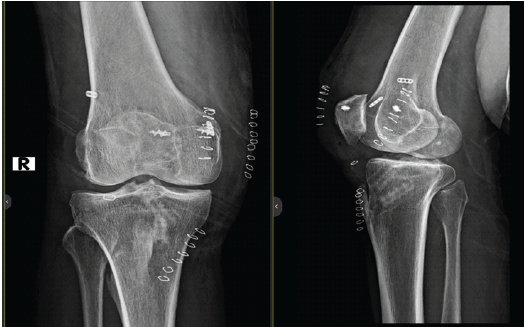
Figure 8: Immediate post-operative X-ray of right knee.
Clinical and functional outcome
One-month post-operative clinical findings
At 1-month follow-up, satisfactory wound healing with no evidence of infection or skin complications. Mild residual knee swelling was present. The patient was able to actively extend the knee and maintain the limb in extension in the supine position. Straight leg raising was possible, indicating preserved quadriceps function with no significant extensor lag. Knee flexion was achieved up to approximately 90°. The patient was able to sit comfortably and perform basic activities of daily living, though prolonged standing and higher-demand activities were restricted.
Radiographs obtained at 1 month showed maintained alignment and appropriate positioning of fixation and reconstruction hardware, with no evidence of implant failure or loss of reduction.
Three-months post-operative clinical findings (Fig. 9)

Figure 9: Three-months post-operative clinical images showing knee flexion and extension, and 3-months post-operative X-ray of the right knee.
At 3-month follow-up, clinical images demonstrated complete healing of surgical scars with healthy surrounding skin and absence of joint effusion or local tenderness. The patient achieved near full knee extension and flexion, with a smooth and painless range of motion. Straight leg raising was performed comfortably without extensor lag, reflecting good quadriceps strength. The patient was able to sit, stand, and ambulate independently without assistive devices. Clinical examination revealed a stable knee with no varus–valgus or anteroposterior instability.
Radiographs at 3 months confirmed maintained joint alignment and stable fixation. Magnetic resonance imaging demonstrated intact reconstructed ACL, PCL, MCL, and MPFL grafts with satisfactory graft integration (Fig. 10).
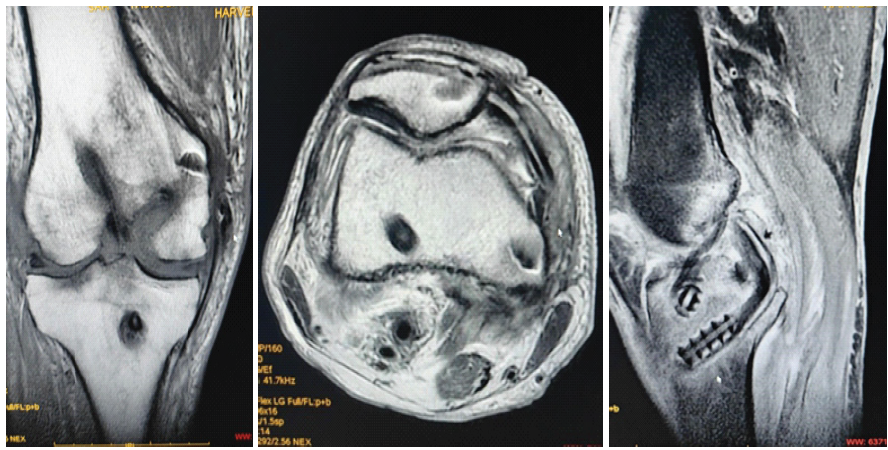
Figure 10: Three-month post-operative magnetic resonance imaging showing reconstructed anterior cruciate ligament and posterior cruciate ligament, reconstructed medial patellofemoral ligament, and reconstructed medial collateral ligament.
Follow-up protocol and functional outcome assessment (Table 1)
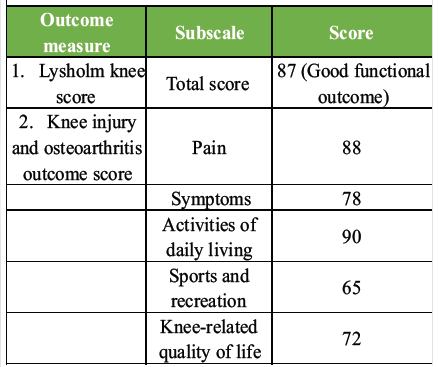
Table 1: Functional outcome scores at final follow-up (3 months)
The patient was followed up at regular intervals postoperatively, with clinical and radiological assessments performed at 1 month and 3 months, and the patient continues to remain under follow-up. At each visit, clinical evaluation included assessment of wound healing, knee range of motion, extensor mechanism function, and ligamentous stability. Standard anteroposterior and lateral radiographs of the knee were obtained to evaluate implant position and osseous alignment. At the 3-month follow-up, magnetic resonance imaging was performed to assess the integrity and continuity of the reconstructed ligaments.
Functional outcome was quantified using the Lysholm Knee Scoring Scale and the Knee Injury and Osteoarthritis Outcome Score (KOOS). At the most recent follow-up of 3 months, the patient demonstrated a Lysholm score of 87, indicating a good functional outcome. At the latest follow-up of 3 months, functional assessment revealed a Lysholm Knee Score of 87, indicating a good functional outcome. The KOOS demonstrated satisfactory improvement across all subscales, with scores of 88 for pain, 78 for symptoms, 90 for activities of daily living, 65 for sports and recreation, and 72 for knee-related quality of life. A limitation of this report is the short-term follow-up duration, which may not fully capture long-term functional outcomes or the durability of ligament reconstructions in an MLKI. In addition, although validated outcome measures were used, the KOOS assessment was performed at a single post-operative time point, and longer-term follow-up is required to evaluate sustained functional recovery and return to higher-demand activities.
Post-operative rehabilitation protocol
A structured, phase-wise rehabilitation protocol was implemented under physiotherapist supervision.
Immediate phase (0–2 weeks)
The knee was immobilized in extension using a hinged knee brace. Quadriceps isometric and ankle pump exercises were initiated. Partial weight bearing was allowed with a walker or crutches.
Early phase (2–6 weeks)
Gradual knee range of motion up to 90° was started with progressive weight bearing as tolerated. Closed-chain quadriceps strengthening was introduced, whereas valgus stress and deep knee flexion were avoided.
Intermediate phase (6–12 weeks)
Full range of motion was achieved with progressive strengthening of quadriceps and hamstrings, along with proprioceptive and balance training.
Advanced phase (3–6 months)
Functional strengthening and agility exercises were initiated, followed by a gradual return to non-contact sports.
Return to sports
Full return to sports was permitted after 9–12 months, based on clinical stability, muscle strength, and functional assessment.
MLKIs represent complex and challenging clinical entities, often resulting from high-energy trauma and frequently associated with polytrauma. These injuries demand meticulous evaluation, timely intervention, and individualized surgical planning to restore knee stability and function. Although operative management has been shown to yield superior outcomes compared with non-operative treatment, consensus regarding the ideal timing, staging, and choice of reconstruction techniques remains controversial. In the present case, the patient sustained a high-energy injury resulting in complete rupture of the ACL, PCL, MCL, and MPFL, along with meniscal tears and LCL sprain. Given the gross instability of the knee, recurrent patellar dislocation during flexion, and the absence of vascular compromise, a single-stage surgical reconstruction was planned. Single-stage reconstruction offers the advantages of early restoration of knee stability, reduced total rehabilitation time, and avoidance of multiple anesthetic exposures, especially in patients who can tolerate a prolonged surgical procedure. A key challenge in multiligament reconstruction is graft availability, particularly in older patients and in scenarios where future revision surgery may be required. In this case, a strategic graft selection was adopted to maximize graft utilization while preserving potential future options. The peroneus longus tendon was used for ACL and PCL reconstruction, thereby sparing the quadriceps and patellar tendons for possible revision procedures. Previous studies have demonstrated that the peroneus longus tendon provides adequate graft strength with minimal donor-site morbidity, making it a reliable alternative in multiligament settings. The medial side injury was addressed using a combination of repair and reconstruction. The MCL tear was identified at its femoral attachment, which is known to have good healing potential. Primary repair augmented with a semitendinosus graft provided additional stability and protected the repair during early rehabilitation. Augmentation rather than isolated repair is particularly beneficial in older patients and in multiligament injuries, where healing capacity may be compromised, and valgus instability can jeopardize cruciate reconstructions. A novel aspect of this case was the utilization of a single semitendinosus graft for both MCL augmentation and MPFL reconstruction. This approach allowed effective reconstruction of two medial stabilizers using one harvested tendon, thereby minimizing donor-site morbidity and conserving graft options. Although MPFL reconstruction is often deferred or staged in multiligament injuries, it was performed in the same sitting in this patient due to persistent patellar instability, with dislocation occurring during knee flexion. Immediate MPFL reconstruction helped restore patellofemoral stability and facilitated early rehabilitation. At short-term follow-up, the patient demonstrated satisfactory clinical and radiological outcomes, with restored knee stability, improved range of motion, and MRI evidence of well-integrated reconstructed ligaments. This case highlights that, with careful planning, single-stage multiligament reconstruction using alternative graft sources and innovative graft utilization techniques can yield favorable outcomes.
This case demonstrates that rerouting and optimal utilization of a semitendinosus graft for combined MCL and MPFL reconstruction is a viable option in MLKIs. This technique not only restores medial and patellofemoral stability but also preserves valuable graft options for future revision surgery, making it particularly useful in complex and resource-limited scenarios.
Learning Points
- Multiligament knee injuries can be effectively managed with a well-planned single-stage reconstruction in selected patients, allowing early restoration of stability and function
- Strategic graft selection and utilization, including using a single semitendinosus graft for both MCL and MPFL reconstruction, helps minimize donor-site morbidity and preserves graft options for future revision surgery
- Addressing patellofemoral instability simultaneously in the presence of recurrent dislocation is crucial to achieving a stable knee and facilitating early rehabilitation.
Careful surgical planning with optimal graft utilization allows safe single-stage reconstruction of complex multiligament knee injuries, restoring stability while preserving graft options for future revision surgery.
References
- 1. Ng JW, Price K, Deepak S. Knee pain in children. Paediatr Child Health 2019;29:521-7. [Google Scholar] [PubMed]
- 2. Schenck RC. Classification of knee dislocations. In: Fanelli GC, editor. The Multiple Ligament Injured Knee: A Practical Guide to Management. New York: Springer; 2004. p. 37-49. [Google Scholar] [PubMed]
- 3. Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury 2011;42:1198-204. [Google Scholar] [PubMed]
- 4. Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: An evidence-based review. Sports Med Arthrosc Rev 2011;19:167-73. [Google Scholar] [PubMed]
- 5. Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations: A meta-analysis. Am J Knee Surg 2001;14:33-8. [Google Scholar] [PubMed]
- 6. Weiss NG, Kaplan LD, Graf BK. Graft selection in surgicalreconstruction of the multiple-ligament-injured knee. Oper Tech Sports Med 2003;11:218-25. [Google Scholar] [PubMed]
- 7. Billières J, Labruyère C, Steltzlen C, Gonzalez A, Boisrenoult P, Beaufils P, et al. Multiligament knee injuries treated by one-stage reconstruction using allograft: Postoperative laxity assessment using stress radiography and clinical outcomes. Orthop Traumatol Surg Res 2019;106:937-44. [Google Scholar] [PubMed]
- 8. Batty LM, Norsworthy CJ, Lash NJ, Wasiak J, Richmond AK, Feller JA. Synthetic devices for reconstructive surgery of the cruciate ligaments: A systematic review. Arthroscopy 2015;31:957-68. [Google Scholar] [PubMed]
- 9. Ranger P, Renaud A, Phan P, Dahan P, De Oliveira E Jr., Delisle J. Evaluation of reconstructive surgery using artificial ligaments in 71 acute knee dislocations. Int Orthop 2011;35:1477-82. [Google Scholar] [PubMed]
- 10. Ranger P, Senay A, Gratton GR, Lacelle M, Delisle J. LARS synthetic ligaments for the acute management of 111 acute knee dislocations: Effective surgical treatment for most ligaments. Knee Surg Sports Traumatol Arthrosc 2018;26:3673-81. [Google Scholar] [PubMed]









