This case highlights the importance of a thorough clinical examination and detailed anamnesis in patients with bilateral shoulder dislocations associated with major tubercle fractures. It also illustrates that tonic-clonic convulsions can cause bilateral glenohumeral dislocations requiring both orthopedic and cardiologic management.
Dr. Touré Layes, Department of Orthopaedic and Trauma Surgery, Bocar Sidi Sall Teaching Hospital, Kati, Mali. E-mail: layestoure854@gmail.com
Introduction: Bilateral dislocations of the glenohumeral joint are most often posterior, secondary to convulsive seizures. We report a case of bilateral anterior dislocation with fracture of the two major tubercles following a very rare mechanism.
Case Report: A 52-year-old patient admitted at the emergency department for bilateral closed shoulder trauma following a tonic-clonic seizure. The patient had a blood pressure of 160/100 mm Hg and a clear consciousness. Symmetrical and bilateral clinical examination of the shoulders shows the signs of bilateral anterior dislocation of the shoulders. The vascular and nerve examinations were normal. Standard shoulder X-ray showed bilateral dislocation in its anterior subcoracoid variety associated with fracture of the major tubercles. The blood test performed showed severe hyponatremia at 113 mmol/L. The dislocations were reduced by the Milch maneuver under sedation. The X-rays showed the reductions. Both shoulders were immobilized with an orthosis and cushion in mild abduction for 4 weeks. The patient stayed in the cardiology department for the management of hypertension and hyponatremia. He benefited the functional rehabilitation sessions after the removal of the orthosis. At the last follow-up at 9 months of the trauma, the shoulders were stable, painless, without recurrence or instability with a normal lifestyle and a muscular strength of 4/5.
Conclusion: This case highlights the importance of general exam and anamnesis in bilateral shoulder dislocations with major tubercles fractures following a tonic-clonic hypertensive convulsion. The treatment is multidisciplinary with orthopedic and cardiological.
Keywords: Shoulders dislocation, shoulder fractures, seizures.
Although anterior dislocations of the glenohumeral joint are the most common dislocations encountered in the emergency department, bilateral forms are very rare [1]. These bilateral dislocations of the glenohumeral joint are most often posterior, secondary to convulsive seizures. Earlier forms are rare. Less than thirty cases have been published [2,3,4]. We report a case of bilateral anterior dislocation with fracture of the two Majors tubercules following a very rare mechanism.
It was a 52-year-old patient, with no known medical history, admitted to the emergency department for bilateral closed shoulder trauma following a tonic-clonic seizure at 4 h after the trauma. On admission, the patient had a blood pressure of 160/100 mm Hg and a clear consciousness. Symmetrical and bilateral clinical examination of the shoulders revealed the signs of bilateral anterior dislocation of the shoulders with an external axe blow and irreducible abduction (Fig. 1a). Sensitivity and motor skills in the axillary nerve area were preserved. Peripheral pulses were present. The examination of the other devices was normal. After conditioning the patient by taking a venous line, administering analgesics and temporarily immobilizing the patient, an imaging and biological assessment was requested. Standard shoulder X-ray revealed bilateral dislocation in its anterior subcoracoid variety associated with fracture of the major tubercles (Fig. 1b, c, d, e).
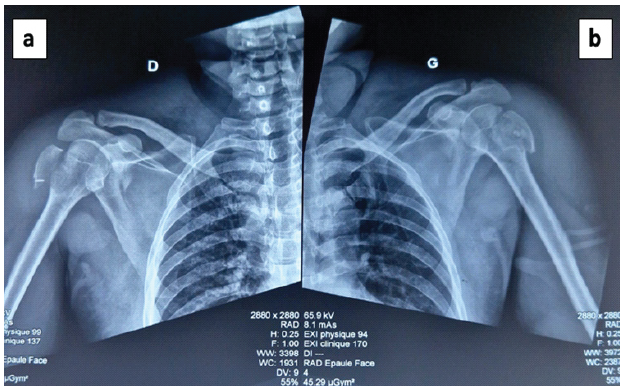
Figure 1: Clinical appearance and X-rays showed the shoulders dislocations. (a) Clinical appearance of the shoulders showed signs of bilateral anterior dislocation of the shoulders with an external axis blow and irreducible abduction (b and c). Right Shoulder’s X-rays showed the shoulder dislocation with major tubercle fracture (d and e). Left Shoulder’s X-rays showed the shoulder dislocation with major tubercle fracture.
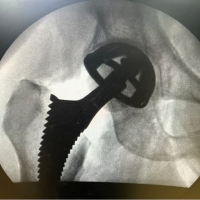
The blood test performed showed severe hyponatremia at 113 mmol/L. Sedated in the operating room, the dislocations were reduced by the Milch maneuver: arm brought to external rotation and abduction gradually, then the humeral head is pushed back, and the arm brought back in medial rotation elbow to the body. The reduction was stable. The follow-up X-ray performed made it possible to objectify a reduction in fractures and dislocations (Fig. 2a and b).
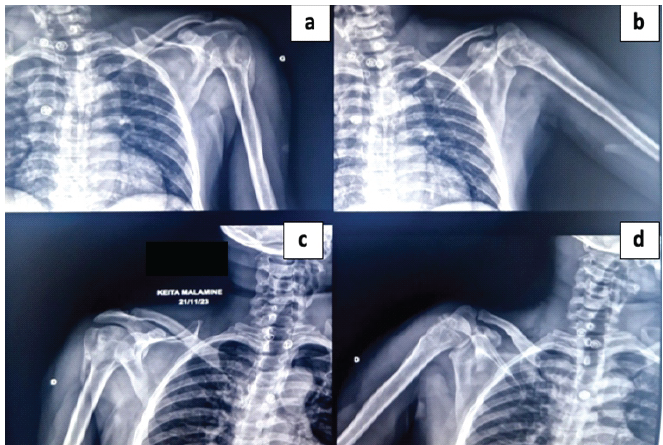
Figure 2: Shoulders X-rays on Anteroposterior views only after the shoulders dislocations reductions. Shoulders X-rays on front views only after the shoulders dislocations reductions showed major tubercles fractures (a) Anteroposterior of Right Shoulder (b) Front view of Left Shoulder.
Both shoulders were immobilized with an orthosis and cushion in mild abduction for 4 weeks. The patient stayed in the cardiology department for the management of hypertension and hyponatremia. He benefited the functional rehabilitation sessions. At 6 weeks of evolution, the fractures were consolidated (Fig. 3a, b, c, d).

Figure 3: Shoulders X-rays at 6 weeks after dislocation reduction. Shoulders X-rays at 6 weeks after dislocation reduction showed major tubercles consolidation process (a and b). Left Shoulders X-rays (c and d), right shoulders X-rays.
The mobility of both shoulders was limited (Fig. 4a and b) with joint ranges of 90° in active abduction going to 130° bilaterally in passive. At the last follow-up at 9 months of the trauma, the shoulders were stable, painless, without recurrence or instability with a normal lifestyle and a muscular strength of 4/5.
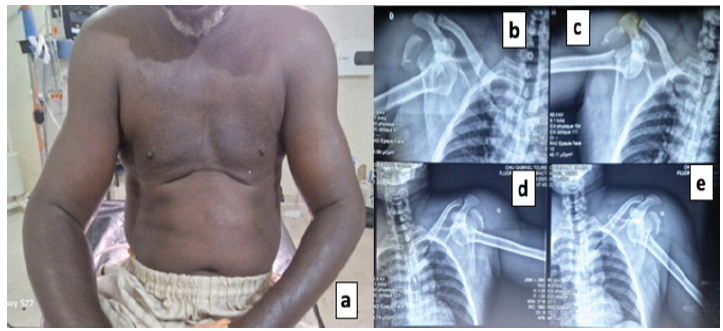
Figure 4: Clinical appearance of shoulders at 6 weeks after the trauma. Clinical appearance of shoulders at 6 weeks after the trauma showed the limited abduction of shoulder <90° (a) Right Shoulder abduction (b) Left Shoulder abduction.
Bilateral shoulder dislocation was first described in 1902 as a result of excessive muscle contraction caused by camphor overdose [5]. They have been the subject of a few publications [6]. Indeed, the force necessary to produce them must act symmetrically and synchronously at the level of the two glenohumeral joints. This happens most often in the event of a convulsive seizure, like in our patient. The etiology of the seizure may follow electrocution or in cases of neuromuscular disease [4]. Brown [1] in 1984 individualized a series of 90 cases of bilateral dislocations. He mentioned three different etiologies: violent muscle contractions (49%), direct trauma (23%) and the absence of any trauma (36%). In these bilateral dislocations, it is the posterior variety that is the most frequent [7,8]. They have been described by Brackstone et al. [9] as the “triple E syndrome” (epilepsy or any convulsive seizure, electrocution, and extreme trauma). As for the earlier varieties, they are rare with only about thirty cases reported [7]. Other unusual mechanisms have been described. Singh et al. [10] reported a case where both shoulders were dislocated by different mechanisms, in a patient with a history of right shoulder instability. The anterior left dislocation was post-traumatic secondary to a fall from a motorcycle with direct landing on the shoulder, while the right side was secondarily dislocated anteriorly during transport, patient held by the right upper limb. In our case, it was a rare mechanism of a tonic-clonic convulsive seizure of hypertensive origin associated with hyponatremia, which led to the anterior dislocation with fracture of the major tubercles. The treatment in our patient was orthopedic by a reduction of dislocations under general anesthesia by the Milch method. Many techniques for reducing dislocations are described [11] but we have avoided the Kocher method which aggravates the displacement of the major tubercle fracture. Whatever reduction maneuver is used, it should be gentle and gradual so as not to aggravate the lesions [12]. Immobilization was performed in slight abduction due to the presence of the fracture of the major tubercle. Our patient did not have a recurrence at the last follow-up, and the prognosis was good after rehabilitation.
Bilateral anterior shoulder dislocations with fractures of the major tubercles are exceptional. We report a case of this type of dislocation in a 52-year-old patient following a tonic-clonic convulsive seizure. Treatment was orthopedic, and the functional outcome acceptable with a limitation of shoulder range.
Early recognition and multidisciplinary management are key to successful recovery in bilateral shoulder dislocations associated with convulsive episodes. Hence, any patient presenting after a convulsive episode should undergo a complete shoulder examination to rule out bilateral dislocations, even in the absence of obvious trauma.
References
- 1. Brown RJ. Bilateral dislocation of the shoulders. Injury 1984;15:267-73. [Google Scholar] [PubMed]
- 2. Maffulli N, Mikhail HM. Bilateral anterior glenohumeral dislocation in a weight lifter. Injury 1990;21:254-6. [Google Scholar] [PubMed]
- 3. Yuen MC, Tung WK, Wong WC, Lau CC. The use of the Spaso technique in a patient with bilateral dislocation of the shoulders. Am J Emerg Med 2001;19:64-6. [Google Scholar] [PubMed]
- 4. Devalia KL, Peter VK. Bilateral post traumatic anterior shoulder dislocation. J Postgrad Med 2005;51:72-3. [Google Scholar] [PubMed]
- 5. Mynter H. XIV. Subacromial dislocation from muscular spasm. Ann Surg 1902;36:117-9. [Google Scholar] [PubMed]
- 6. Dunlop CC. Bilateral anterior shoulder dislocation–a case report and review of the literature. Acta Orthop Belg 2002;68:168-70. [Google Scholar] [PubMed]
- 7. Bouras Y, Elandaloussi Y, Nadil MA. Bilateral anterior shoulder dislocation in bodybuilders: About a case. J Sports Traumatol 2009;26:247-9. [Google Scholar] [PubMed]
- 8. Ryan J, Whitten M. Bilateral locked posterior shoulder dislocation in a footballer. Br J Sports Med 1997;31:74-5. [Google Scholar] [PubMed]
- 9. Brackstone M, Patterson SD, Kertesz A. Triple “E” syndrome: Bilateral locked posterior fracture dislocation of the shoulders. Neurology 2001;56:1403-4. [Google Scholar] [PubMed]
- 10. Singh S, Kumar S, Kumar R, Mehta S. Bilateral anterior shoulder dislocation: A case report. Eur J Emerg Med 2005;12:33-5. [Google Scholar] [PubMed]
- 11. Genin J. Management of glenohumeral dislocation by winter sports resort physicians. J Sports Traumatol 2001;18:113-22. [Google Scholar] [PubMed]
- 12. Sirveaux F, Molé D, Walch G. Instabilities and glenohumeral dislocations. In: Encyclopédie Médico-Chirurgicale. Musculoskeletal System. Paris: Elsevier Masson; 2002. [Google Scholar] [PubMed]