[box type=”bio”] What to Learn from this Article?[/box]
Use of Technology in form of 3-D printing to plan and execute complex bony surgeries.
Case Report | Volume 5 | Issue 1 | JOCR Jan-March 2015 | Page 23-25 | James M Duncan, Samuel Nahas, Kashif Akhtar, Jasvinder Daurka. DOI: 10.13107/jocr.2250-0685.247
Authors: James M Duncan[1], Samuel Nahas[2], Kashif Akhtar[2], Jasvinder Daurka[2]
[1] Kings College Hospital, London
[2] Imperial College Hospitals NHS Trust, London.
Address of Correspondence:
Dr. James M Duncan Flat 1, 39 Tunstall Road, London, SW9 8BZ. Email: James.duncan41@gmail.com
Abstract
Introduction: Surgical management of acetabular fractures is often highly complex, and a successful outcome depends upon an appreciation of the fracture pattern and the most appropriate approach to reduce and hold it. Currently, computed tomography (CT) images are used in conjunction with plain x-rays to identify the main fracture components and their spatial relationship to one another, and as such surgeons still have to make decisions based upon their ability to visualise the fracture from the images available. 3D printers have now become widely available and inexpensive, and can be used to rapidly produce life-size models based on CT scans of an individual patient. The availability of patient specific, accurate and detailed models of complex acetabular fractures can aid planning of surgical management on a patient specific basis.
Case Report: This report describes the use of a 3D printer to create a life-size model reconstruction of the pelvis of a 48 year old male patient who sustained a left sided associated both column acetabular fracture following a motorbike accident in the Sahara Desert. The model allowed visualisation of the multiple fracture fragments and their relative displacements. The tactile feedback allowed assessment of the different fracture fragments. The relative displacement of the quadrilateral plate and posterior column fragments could be assessed and the surgeon felt that these would be amenable to reduction from an ilioinguinal approach. An anatomic reduction was achieved and was held with the application of a pelvic brim plate with 2 screws lagging the posterior column/quadrilateral plate fragment.
Conclusion: There are previous examples of 3D models being used in orthopaedic surgery through the use of rapid prototyping, however this method is usually expensive and time consuming. Advances in 3D printer technology offer surgeons a number of advantages when treating these complex fractures. With the ever-increasing economy, ease of use and speed of additive processing, the possible applications of this technology within orthopaedic surgery are numerous. Given the possible applications of this technology, and its ever increasing availability, we feel that its use can only improve patient outcomes and so should be explored further for use in orthopaedic surgery.
Keywords: 3D printing, acetabular reconstruction, trauma.
Introduction
Surgical management of acetabular fractures is often highly complex, and a successful outcome depends upon an appreciation of the fracture pattern and the most appropriate approach to reduce and hold it. The importance of the choice of approach as a prognostic indicator has been previously highlighted [1,2]. Currently, two- and three-dimensional computed tomography (CT) images are used in conjunction with plain x-rays to identify the main fracture components and their spatial relationship to one another. However, because these images are viewed on a screen, they give the surgeon limited insight into the physical configuration of the fracture and the optimal surgical management to be used [3,4]. Surgeons still have to make important decisions based upon a combination of their ability to visualise the fracture from the images available, and intraoperative direct fluoroscopy following fracture reduction [5].
3D printers have now become widely available and inexpensive, and can be used to rapidly produce life-size models based on CT scans of an individual patient. The availability of patient specific, accurate and detailed models of complex acetabular fractures can aid planning of surgical management and allow a better appreciation of both the most appropriate approach and the reduction manoeuvres required on patient specific basis.
Case report
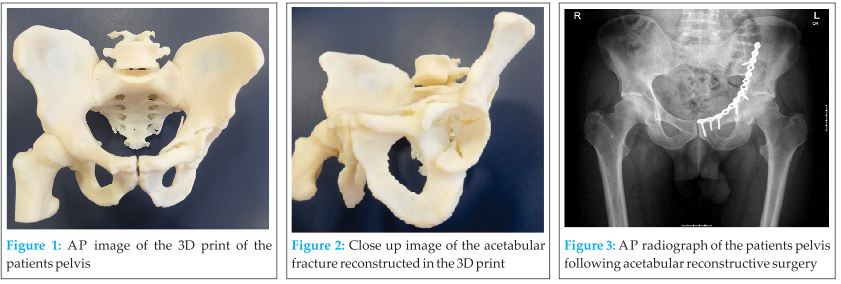
This report describes the use of a 3D printer to create a life-size model reconstruction of the pelvis of a 48 year old male patient who sustained a left sided associated both column acetabular fracture following a motorbike accident in the Sahara Desert. The 3D print was created from the CT images taken of the patient, and was then used to help plan surgery and assist intra-operatively (Figs 1 & 2). The DICOM imaging files were converted to STL to enable printing on an Objet Eden 250 printer utilizing selective laser sintering of nylon (Stratasys Inc, Rehovot Israel).
The model allowed a visualisation of the multiple fracture fragments and their relative displacements. The tactile feedback allowed an assessment of the different fracture fragments. The relative displacement of the quadrilateral plate and posterior column fragments could be assessed and the surgeon felt that these would be amenable to reduction from an ilioinguinal approach. The confidence with which this could be decided preoperatively prevented the patient from undergoing a dual or an extensile approach.
An anatomic reduction was achieved and this was held with the application of a pelvic brim plate with 2 screws lagging the posterior column/quadrilateral plate fragment (Fig 3).
Discussion
There are previous examples of 3D models being used in orthopaedic surgery through the use of rapid prototyping (6-8), however this method is usually expensive and time consuming, as the manufacturing process was much more difficult. Advances in 3D printer technology used in combination with user-friendly software and early CT scan assessment of injuries, offer surgeons a number of advantages when treating these complex fractures. It can allow better assessment of the nature of the injuries sustained, and give the surgeon better visuospatial appreciation of the relation of fracture fragments to one another, and therefore aid the decision regarding optimal approach to be used, and fixation technique including size of implants and trajectories of screws. This reduces over-all surgical time by assisting pre-operative planning, which in turn reduced the risk of a multitude of complications.
Conclusion
With the ever-increasing economy, ease of use and speed of additive processing, the possible applications of this technology within orthopaedic surgery are numerous. There is also scope for the development of custom made implants and pre-contoured plates that are unique to a patient’s anatomy and fracture type and this has already been explored in maxillofacial surgery where direct laser metal sintering has been used to produce custom titanium miniplates (9).
Clinical Message
Given the possible applications of 3D printing technology in trauma and orthopaedic surgery, and its ever increasing availability, we feel that its use can only improve patient outcomes and so should be explored further for use in orthopaedic surgery.
References
1. Giannoudis PV, Grotz MRW, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. Journal of Bone and Joint Surgery – British Volume. 2005;87:2–9.
2. Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. Journal of Bone and Joint Surgery – American Volume. 2012;94(17):1559-67.
3. Brown GA, Milner B, Firoozbakhsh K. Application of computer-generated stereolithography and interpositioning template in acetabular fractures: a report of eight cases. J Orthop Trauma. 2002;16:347-352.
4. Citak M, Gardner MJ, Kendoff D, Tarte S, Krettek C, Nolte LP, Hufner T. Virtual 3D Planning of Acetabular Fracture Reduction. J Orthop Res. 2008;26:547-552.
5. Fornaro J, Keel M, Harders M, Marincek B, Szekely G, Frauenfelder T. An Interactive Surgical Planning Tool for Acetabular Fractures: Initial results. J Orthop Surg Res. 2010;5:50.
6. Bagaria V, Deshpande S, Rasalkar DD, Kuthe A, Paunipagar BK. Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. European journal of radiology [Internet]. Elsevier Ireland Ltd; 2011 Dec [cited 2013 Sep 24];80(3):814–20. .
7. Krishnan SP, Dawood A, Richards R, Henckel J, Hart a J. A review of rapid prototyped surgical guides for patient-specific total knee replacement. J Bone Joint Surg [Br]. 2012 Nov;94(11):1457–61.
8. Brown G, Firoozbakhsh K, DeCoster T, Reyna Jr J, Moneim M. Rapid prototyping: the future of trauma surgery? J Bone Joint Surg[Am]. 2003;85:49–55.
9. Philippe B. Custom-made prefabricated titanium miniplates in Le Fort I osteotomies: principles, procedure and clinical insights. Int J Oral Maxillofac Surg. 2013;42(8):1001–6.
| How to Cite This Article: Duncan JM, Nahas S, Akhtar K, Daurka J. The Use of a 3D Printer in Pre-operative Planning for a Patient Requiring Acetabular Reconstructive Surgery.. Journal of Orthopaedic Case Reports 2015 Jan-March;5(1): 23-25. Available from: https://www.jocr.co.in/wp/2015/01/28/2250-0685-247-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com