[box type=”bio”] What to Learn from this Article?[/box]
Conservative management can be considered in cases of solitary epithelioid hemangioendotheliomas of bone. It will avoid extensive surgeries especially in infants, thus saving the involved limbs.
Case Report | Volume 5 | Issue 1 | JOCR Jan-March 2015 | Page 37-40 | Lekha K.Nair, Anitha Das, Arun Kumar A.S, V. Ramachandran. DOI: 10.13107/jocr.2250-0685.251
Authors: Lekha K.Nair[1], Anitha Das[1], Arun Kumar A.S[1], V. Ramachandran[1].
[1] Department of Pathology, MES Medical College, Perinthalmanna. Malappuram District. Kerala. India.
Address of Correspondence:
Dr.Lekha K.Nair, Chelakkat house, ( PO) Thaikkad,(Via) Guruvayur, Thrissur Dist.680104. Kerala, India. Email: lekhamukundan5@gmail.com
Abstract
Introduction: Epitheloid hemangioendothelioma is a rare vascular soft tissue tumour of intermediate malignant potential. The tumor affects any age group, and liver is the commonest internal organ affected. Bones as calvarium, spine, tibia and femur may also be affected. The lesion can be multifocal in the liver or the same bone itself and can metastasise to lungs. Here we report a rare case of epithelioid hemangioendothelioma involving tibia in a male infant, which regressed by itself without any treatment, after incisional biopsy over a period of one and half years..
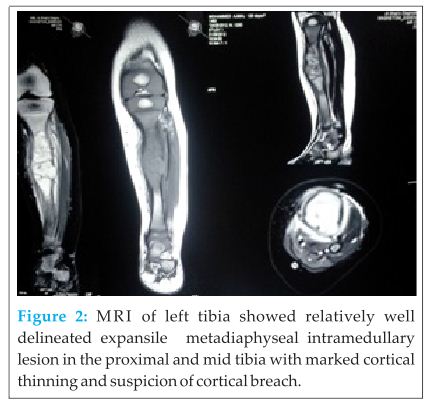
Case Report: A 7 month old male baby was presented with incessant cry, fever and swelling in left upper leg of 2 weeks duration.X-ray of leg showed a well demarcated lytic lesion in the meta diaphysial region of left tibia. Magnetic resonance imaging showed an irregular lytic lesion with intramedullary extension. Incisional biopsy showed a vascular tumor, epithelioid hemangioendothelioma grade 1. Meanwhile the patient became asymptomatic and subsequent follow ups showed regression in the size of the tumor and complete disappearance after one and half years. This points towards the need of a wait and watch policy in such intermediate grade vascular tumours even though the lesion is so extensive. This is the first case report of an extensive self regressing epithelioid hemangioendothelioma of tibia in an infant to our knowledge.
Conclusion: Intermediate grade vascular tumors can undergo spontaneous regression which points towards the need of a wait and watch policy in such tumors thus avoiding extensive surgeries, especially in young patients.
Keywords: epithelioid, hemangioendothelioma, vascular tumors.
Introduction
Epithelioid hemangioendothelioma (EHE) is a rare, well-differentiated endothelial tumour with a wide spectrum of behaviour. The term was designed to describe vascular soft tissue tumors between hemangiomas and angiosarcomas in terms of local recurrences and metastatic potential[1].Epithelioid hemangioendothelioma has several synonyms: low grade anaplastic angiosarcoma, cellular hemangioma, histiocytoid hemangioma and angioendothelioma. It represents 1% of all vascular neoplasms and is locally aggressive[2]. Hemangioendotheliomas of bone are multifocal and multi centric in contrast to other soft tissue tumors. A case of epitheloid hemangioendothelioma arising in bone is presented in the study with its clinical, radiological and histopathological features.
Case report
We report a case of epithelioid haemangioendothelioma of left tibia in 7 month old boy. He presented with fever and persistent cry of about 2 weeks duration. Parents noticed a swelling on left upper tibia .On examination there was a diffuse swelling at the anteromedial aspect of the left leg in the junction of upper and middle one third, measuring approximately 8x3x3 cms. Skin was shiny. No dilated veins or visible pulsations were seen on the skin over the swelling. Tenderness was present at the site of swelling. No abnormal movements or deformities, or other bone involvement were noticed. X-ray of left tibia showed an expansile osteolytic and poorly demarcated lesion involving the metaphyseo-diaphyseal region of left upper tibia (Fig 1).

Discussion
Epitheloid hemangioendothelioma, is an angiocentric vascular tumour[3]. Vascular tumors originating from bone constitute an infrequent group of tumors of bone. The term epithelioid hemangioendothelioma was first used by Weiss and Enzinger in 1982 for a vascular tumor of soft tissue with intermediate malignancy, showing features between hemangioma and angiosarcoma[4]. Although initially described most commonly in soft tissues, other sites including liver, lungs and long bones as femur, tibia and humerus[5,6] are well reported. Epithelioid hemangioendothelioma of bone has been encountered in virtually all age groups and can be multicentric, although it appears to peak both during the second and third decades and again in the later decades of life[7].Clinically, epithelioid hemangioendotheliomas present with pain and swelling. If spine is involved, the lesion may cause radicular symptoms or paraplegia[7].
On radiographic examination, epithelioid hemangioendotheliomas are expansile, osteolytic and poorly demarcated lesions. They have a distinctive “soap-bubble” matrix with sclerotic margins[7]. No periosteal reaction is present. Lesions with particularly ill-defined margins and loss of trabeculae are considered to be more aggressive. CT scan findings are noncontributory as they reflect only soft-tissue density, but lesions do enhance with contrast media[2].
MRI findings are also non-specific. The radiological differential diagnosis includes metastatic carcinoma, Ewing’s sarcoma, telangiectatic osteosarcoma, lymphoma, fibrous dysplasia and aneurysmal bone cyst[2].
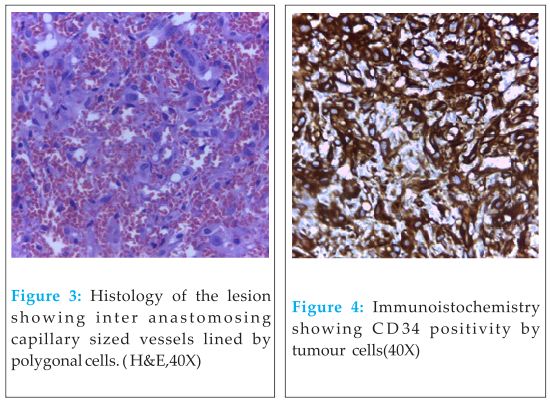
On gross examination, epithelioid hemangioendotheliomas are reddish-brown loculated masses with significant hemorrhage[2]. Microscopically, epithelioid hemangioendotheliomas expand vessels, usually preserving architecture as they expand centrifugally from lumen to soft tissue. Lumen is filled with combination of tumour, necrotic debris and dense collagen. Tumours are composed of short strands or solid nests of rounded to slightly spindled endothelial cells. Tumour cells form small intracellular lumens, which are seen as clear spaces or vacuoles which distort or blister the cells. Stroma varies from highly myxoid to hyaline[3]. Various criteria like the number of mitoses, hyperchromatic nuclei, pleomorphism and nucleus to cell ratio are used to determine the aggressiveness of the lesion (benign or malignant). While the cases with cellular atypia, increased mitotic activity and necrosis are expected to show a worse prognosis, it is not possible to predict prognosis only with the morphological features, for it is known that some low grade lesions may also metastasize. Because of the high incidence of the multifocal lesions in epithelioid hemangioendothelioma, it is necessary to perform bone scan and design the treatment plan accordingly. Immunohistochemistry shows typical endothelial phenotype with expression of vWF, CD31, CD34, FLI-1protein. LMW cytokeratin is expressed in 25% cases[8]. WWTR1-CAMTA1 gene fusion that results from a reciprocal t(1;3)(p36;q25)translocation is present in nearly all investigated EHE cases but is absent in other vascular neoplasms[9,10]. Reports have described a possible correlation between Bartonella infection and hepatic EHE[11,12] which may result from a relationship between infection, vascular endothelial growth factor induction, and angioproliferative disease[13-15].
The treatment of epithelioid hemangioendothelioma depends on the grade of the lesion. Benign appearing lesions may be treated with curettage, or wide resection wherever possible. Wide resection or (rarely) amputation is necessary for more aggressive tumors. The role of radiation and chemotherapy is ill defined at this time. Epithelioid hemangioendotheliomas may metastasize to bone and lung. Prognosis in these rare instances has been variable but may be good[2]. Tumors that initially appeared as histologically benign, but then progressed to metastatic disease have been well documented[16].
Conclusion
Epithelioid haemangioendothelioma presenting as infantile form is rare especially in tibia. Spontaneous regression of the tumor, as in our case, points towards the need of a wait and watch policy in the management of low grade epithelioid hemangio endotheliomas and towards categorizing the tumor in to one of self regressing tumors. Hence, there is role for conservative management in borderline vascular bone tumors.
Clinical Message
Chances of a conservative management should be kept in mind, once the diagnosis of epithelioid hemangioendothelima is met with, thus avoiding extensive surgeries, amounting towards saving a limb in case of extremities.
References
1.Gill R, O’ Donnell RJ, Horvai A. Utility of immunohistochemistry for endothelial markers in distinguishing epitheloid hemangioendothelioma from carcinoma metastasis to bone . Arch Pathol Lab Med, 2009, 133 (6):967-970.
2.http://www.bonetumor.org/unknown-tumor-soft-tissue/epithelioidhemangioendothelioma
3. Goldblum J.R, andSharon W. Weiss, Enzinger and Weiss’s Soft TissueTumors , Fifth Edition,Chapter 23, 681-687.
4.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer,1982, 50 (5):970-8.
5. Jinghong X, Lirong C. Pulmonary epithelioid hemangioendothelioma accompanied by bilateral multiple calcified nodules in lung. Diagn Pathol.2011, 6:21.
6. Kleer CG, Unni KK, McLeod RA. Epithelioid hemangioendothelioma of bone. Am J Surg Pathol. 2006, 20 (11):1301-11.
7. Epitheloid hemangioendothelioma of bone.www. hum path.com, Human pathology, 17 March 2011.
8. Flope A L, Inwards CY , Bone and soft tissue pathology. Chapter 9, 183-186.
9. Errani C, Zhang L, Sung YS, et al: A novel WWTR1-CAMTA1 gene fusion is a consistent abnormality in epithelioid hemangioendothelioma of different anatomic sites. Genes Chromosomes Cancer, 2011, 50:644-653.
10. Tanas MR, Sboner A, Oliveira AM, et al: Identification of a disease-defining gene fusion in epithelioid hemangioendothelioma. Sci Transl Med.2011,Aug 31, 3(98):98ra82.
11. Breitschwerdt EB, Maggi RG, Varanat M, et al: Isolation of Bartonella vinsonii subsp. berkhoffii genotype II from a boy with epithelioid hemangioendothelioma and a dog with hemangiopericytoma. J Clin Microbiol,2009, 47:1957-1960.
12. Mascarelli PE, Iredell JR, Maggi RG, et al: Bartonella species bacteremia in two patients with epithelioid hemangioendothelioma. J Clin Microbiol, 2011, 49:4006-4012.
13. Kempf VA, Volkmann B, Schaller M, et al: Evidence of a leading role for VEGF in Bartonella henselae-induced endothelial cell proliferations. Cell Microbiol 2001,3:623-632.
14. Dehio C: Molecular and cellular basis of bartonella pathogenesis. Annu Rev Microbiol 2004, 58:365-390.
15. Resto-Ruiz SI, Schmiederer M, Sweger D, et al: Induction of a potential paracrine angiogenic loop between human THP-1 macrophages and human microvascular endothelial cells during Bartonella henselae infection. Infect Immun 2002, 70:4564-4570.
16. Weiss SW, Ishak KG, Dail DH, Sweet DE, Enzinger FM. Epithelioid hemangioendothelioma and related lesions. Semin Diagn Pathol. 1986, 3(4):259-87.
| How to Cite This Article: Nair LK, Das A, Arun Kumar AS, Ramachandran V. Self Regressing Epitheloid Haemangioendothelioma of Tibia in an Infant- A rare case report and review of literature. Journal of Orthopaedic Case Reports 2015 Jan-March;5(1): 37-40. Available from: https://www.jocr.co.in/wp/2015/01/28/2250-0685-251-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com