[box type=”bio”] What to Learn from this Article?[/box]
Post tuberculosis bilateral knee deformities treated using external fixator with successful results.
Case Report | Volume 5 | Issue 1 | JOCR Jan-March 2015 | Page 48-51 | Aakash Mugalur, Aditya C Pathak, Sunil M Shahane, Ashwin Samant. DOI: 10.13107/jocr.2250-0685.254
Authors: Mugalur A[1], Pathak AC[1], Shahane SM[1], Samant A[1]
[1] Department Of Orthopaedics, Dr RN Cooper Hospital, Vile Parle –West, Mumbai-400056, Maharashtra, India.
Address of Correspondence:
Dr. Aditya C Pathak, Neelam Nagar Phase 2, J-11/204, Near Jain Temple, Mulund-East, Mumbai – 400 081, Maharashtra, India. Email: dr_acp18@yahoo.co.in, acp.ortho@gmail.com
Abstract
Introduction: Bilateral Flexion Deformity commonly results secondary to cerebral palsy, poliomyelitis, haemophilia etc. It is accompanied by valgus deformity and external rotation at knee in long standing cases secondary to the contracture of the iliotibial tract. Flexion deformity at knees is an impediment to the normal ambulation and is difficult to address.
Case Report: A 34 year old male presented with bilateral knee stiffness. He had multifocal tuberculosis and was bed ridden for almost a year and consequently developed bilateral knee flexion deformity of 60o with further flexion upto 120o. Patient was treated with gradual distraction using a modified external fixator and achieved full correction at the end of 6 weeks. At final followup patient was walking comfortably and was able to squat and sit crossed legged.
Conclusion: Idiopathic isolated bilateral flexion deformity of knees is very rare and is an impediment to normal ambulation. Arthrodiastasis with indigenously designed fixator using the Ilizarov principle and modified fixator is a simple, efficient and cost effective treatment for flexion deformity of knee.
Keywords: knee, flexion, deformity, external fixator.
Introduction
Bilateral knee flexion deformity develops in association with arthrogryposis, popliteal pterygium syndrome, sacral agenesis, poliomyelitis, haemophilia & cerebral palsy [1,2,3]. It is very rare to find bilateral isolated flexion deformity of knee as it is often complicated by valgus deformity, subluxation, and external rotation of the tibia on the femur because the hamstring muscles pull the tibia posteriorly and the biceps femoris and the iliotibial band rotate the tibia externally [4]. Traction with balanced suspension, Buck extension, static and dynamic splints, casts, or braces designed to extend the knee gradually are of value in the conservative management of flexion contracture of knee. Surgical options in adults include soft tissue release procedures, gradual distraction using the Ilizarov principle or a combination of the above [4]. We report a case of idiopathic bilateral flexion deformity of knees with an indigenously developed Bhosale fixator [5] with complete correction of the deformity and recovery of pain-free full range of movement. The case is unique with respect to etiology, presentation and management and is yet not reported in literature till date.
Case report
A 34 year male Indian patient presented with bilateral flexion deformity of knees with chief complaints of inability to walk over the past one year. The patient was admitted and treated for disseminated tuberculosis over the past eight months at a hospital. The general condition of the patient was poor and was completely bedridden throughout the eight months of AKT( Anti Kochs Therapy) treatment . Patient was non-compliant with bracing and physiotherapy during that period and had developed flexion deformity of knee. There was no history of trauma, haemophilia or any other significant childhood history like cerebral palsy and the patient was symptom free and had a normal pain-free bipedal gait before the onset of disseminated tuberculosis.
On clinical examination the patient had a flexion deformity in bilateral knees of 60 degrees with further pain-free flexion possible upto 120 degrees bilaterally (Fig 1). 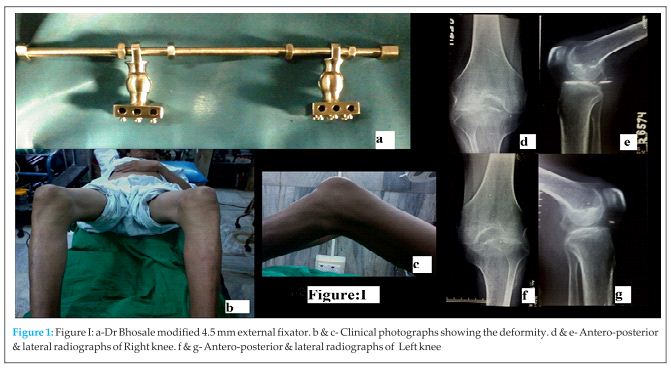
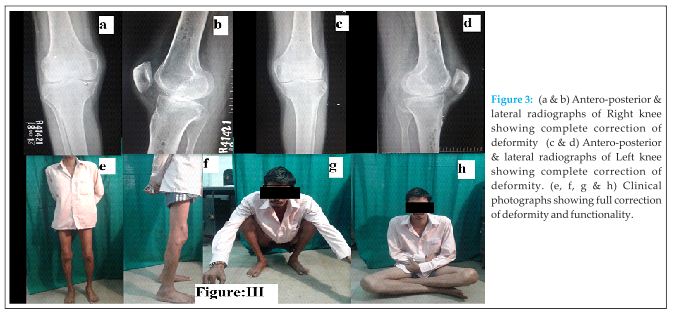
The cast was removed and the patient was subjected to physiotherapy over a period of six weeks to achieve functional range of motion and quadriceps strength. Gait training was given to the patient along with push knee brace. The patient gained a normal pain-free full range of motion of both the knees with a normal bipedal unassisted gait. A total of 17 weeks elapsed from the onset of the treatment till the patient regained bipedal unassisted gait. The patient is able to squat and sit cross-legged.( Fig 3).
Discussion
Bilateral flexion deformity in knees is generally caused due to arthrogryposis multiplex congenita, lumbosacral agenesis, poliomyelitis, multiple pterygium syndrome, cerebral palsy and in rare cases haemophilia [1,2,3]. There was no evidence of osteoarticular or spinal Kochs at presentation. Inflammatory disorders were ruled out based on the serology and the lack of symmetrical involvement of small joints of hand/foot or spine clinico-radiologically. The coagulation profile of the patient was normal. Congenital, traumatic and developmental causes of flexion deformity were ruled out as the patient was absolutely normal before the onset of disseminated tuberculosis. We present here a case of bilateral flexion deformity of knee with the etiology most likely being postural. We could not find idiopathic bilateral isolated flexion deformity of knees in the literature.
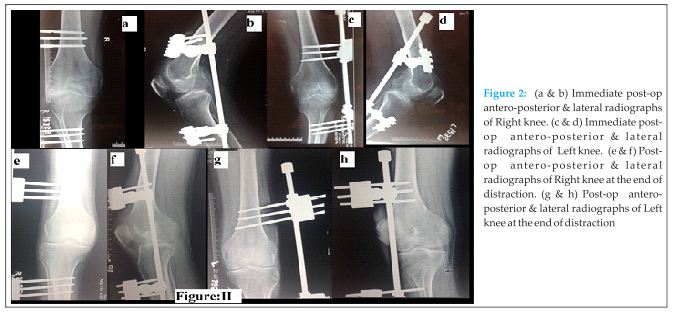
The flexion deformity of knees usually can be at least partially corrected conservatively. Traction with balanced suspension, Buck extension, static and dynamic splints, casts, or braces designed to extend the knee gradually are of value. These measures can be used before surgery to make the operation less extensive and after surgery to increase the correction.[4]Progressive correction of the knee flexion deformity by skeletal traction is associated with high morbidity, such as pain, pin site infection, and posterior subluxation of the knee, and usually does not correct the deformity entirely, necessitating further surgery at a later date. Serial casting was avoided in cases of flexion deformity greater than 20°, because of its poor outcome and complications such as pressure sores, pain and subluxation of the knee.[6]Surgical procedures proposed to treat flexion knee deformity are lengthening of the hamstrings, posterior capsulotomy, supracondylar femoral extension osteotomy or proximal tibial wedge osteotomy, femoral shortening and arthrodesis. Osteotomies are effective but change the anatomy of the joint. Massive soft tissue release may lead to joint instability. Martin et al[7] effectively treated flexion deformities in adults by acute posterior soft tissue release maintained by knee spanning unilateral external fixator accompanied by daily stretching and active physiotherapy on daily basis in partially corrected cases. They concluded that their method of treatment was safe and effective with no recurrence, instability and no neurological or vascular complications. However acute correction of flexion knee contracture with soft tissue release, osteotomy, or both may lead to serious complications. Soft tissue release may be complicated by peroneal palsy, knee subluxation, hyperextension, skin necrosis, and recurrence [8]. Dror Paley [9] emphasised that correction of severe deformities (>40o) should rarely be attempted at one sitting. Distraction arthrodiastasis may induce an increased fibrous tissue response which may be more pronounced after soft tissue release. Hence many prefer gradual correction with the frame without a soft tissue release [10]. Gradual correction of the deformity has been achieved by many authors using Ilizarov circular fixator [11] and monolateral fixators[8]. Herzenberg [8] et al observed that the average total arc of motion remained essentially unchanged after treatment though the functional range of motion improved substantially.
As the deformity was significant acute radical release and correction of deformity was not done due to risk of soft tissue complications and peroneal nerve injury. The severity of the deformity prevented the use of the serial casting. Bilateral application of ring fixator is cumbersome both for the patient and for the surgeon. We treated this particular case using the indigenously developed Bhosale fixator which is also based on Ilizarov principle. The swivel clamps at either ends help to correct the angular deformity at the time of distraction and no separate hinges are required. Since it is a monolateral fixator compliance was not an issue and very simple to apply. It is cost effective when compared to the Ilizarov and Limb Reconstruction System monolateral fixator. However the fixator has its own limitations. The fixator cannot be used if there is subluxation of the knee joint. Its difficult to get optimal results in osteoporotic bones and multiplanar deformities.
We are not aware of bilateral flexion deformity in the literature with etiology being postural. Although the flexion deformity was of long duration it wasn’t associated with valgus malalignment, external rotation or posterior subluxation of the knee joint. We treated this case using indigenously devised Dr Bhosale fixator without soft tissue release. We achieved full correction of the deformity with pain-free full range of motion at the knee joint with no residual stiffness.
Acknowledgement:
Dr( Prof) P B Bhosale, Former Head of the department of orthopaedics, KEM Hospital, Mumbai.
Conclusion
Idiopathic isolated bilateral flexion deformity of knees is very rare and is an impediment to normal ambulation. Arthrodiastasis with indigenously designed Bhosale fixator is a simple, efficient and cost effective treatment for flexion deformity of knee. Regular physiotherapy with range of motion exercises in a bed ridden patient should prevent such deformities.
Clinical Message
Regular structured physiotherapy is very important to maintain range of motion of joints in chronically ill bed-ridden patients to prevent the avoidable problem of joint deformity. The indigenously designed Bhosle fixator is valuable and cost-effective in treating flexion deformity of knees. However such deformities are better prevented.
References
1. Hosny GA, Fadel M. Managing flexion knee deformity using circular a circular frame.Clin Orthop Relat Res. 2008 December; 466(12): 2995–3002.
2. Ma FY, Selber P, Nattrass GR, Harvey AR, Wolfe R, Graham HK. Lengthening and transfer of hamstrings for a flexion deformity of the knee in children with bilateral cerebral palsy: technique and preliminary results. J Bone Joint Surg Br. 2006 Feb;88(2):248-54.
3.Kumar A, Logani V, Neogi DS, Khan SA, Yadav CS, Rao S. IIlizarov external fixator for bilateral severe flexion deformity of the knee in haemophilia: case report. Arch Orthop Trauma Surg. 2010 May;130(5):621-5.
4. Robert H, Miller III, Azar FM. Knee injuries in: Canale ST. Beaty JH, Campbell’s Operative Orthopaedics, 11th edition, Mosby Elsevier; 2008; p.2395-2600.
5. Patel DA, Knee in poliomyelitis in: Kulkarni GS. Textbook of orthopaedics and trauma, 2ndedition,Jaypee 2008. Chapter 71; p567-573.
6. de Moraes Barros Fucs PM, Svartman C, de Assumpção RM. Knee flexion deformity from poliomyelitis treated by supracondylar femoral extension osteotomy. Int Orthop. 2005 Dec;29(6):380-4.
7. Martin JN, Vialle R et al. Treatment of knee flexion contracture due to central nervous system disorders in adults JBJS.(Am) 2006;88(4):840-845
8.Herzenberg JE, Davis JR, Paley D, Bhave A. Mechanical distraction for treatment of severe knee flexion contractures. Clin Orthop Relat Res. 1994; 301:80–88.
9. Dror Paley.TKR and total hip replacement associated with malalignment in: Principles of deformity correction. Verlag: Springer;2002. p. 777-798
10. Herring JA. Disorders of the knee in: Tachdjian’s Pediatric Orthopaedics: From the Texas Scottish Rite Hospital., 5th edition, Saunders Elsevier;2013.; p.682-712.
11. Damsin JP, Ghanem I. Treatment of severe flexion deformity of the knee in children and adolescent using the Ilizarov technique. J Bone Joint Surg Br. 1996;78:140–144.
| How to Cite This Article: Mugalur A, Pathak AC, Shahane SM, Samant A.Successful Correction of Idiopathic Bilateral Flexion Deformity of Knee: A Rare Case Report.Journal of Orthopaedic Case Reports 2015 Jan-March;5(1): 48-51. Available from: https://www.jocr.co.in/wp/2014/11/29/2250-0685-250 / fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com