[box type=”bio”] What to Learn from this Article?[/box]
In a case presenting with bilateral leg pain, erythema and swelling, compartment syndrome is still a differential even in an atraumatic case.
Case Report | Volume 5 | Issue 2 | JOCR April-June 2015 | Page 9-11 | Benjamin Pal Kapur, Michael Grant, Muthukrishnan Ramakrishnan. DOI: 10.13107/jocr.2250-0685.260
Authors: Benjamin Pal Kapur[1], Michael Grant[1], Muthukrishnan Ramakrishnan[1]
[1] Department of Orthopaedics, Wirral University Teaching Hospital NHS Trust, Arrowe Park Rd, Wirral, Merseyside,CH49 5PE. United Kingdom.
Address of Correspondence:
Dr. Benjamin Pal Kapur,
2 Willowdale Road, Mossley Hill, Liverpool, L18 1DJ. United Kingdom.
E-mail: benjaminpkapur@gmail.com
Abstract
Introduction: A traumatic bilateral compartment syndrome is not widely reported. There is usually a precipitating event to cause compartment syndrome for example open and closed fractures, plaster of Paris application, burns and post-ischaemia reperfusion injury. This case confirms the need for a high index of suspicion for compartment syndrome in a patient presenting with bilateral leg pain, swelling and erythema as early diagnosis and urgent decompression by fasciotomy is of vital importance to preserve limb function and avoid complications.
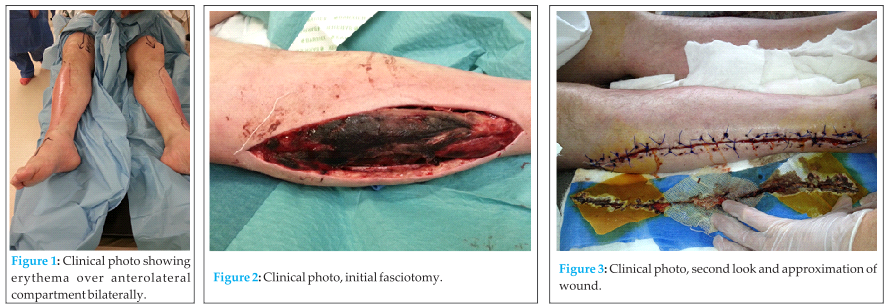
Case Report: We wish to report the case of atraumatic bilateral anterolateral compartment syndrome in a 58-year-old Caucasian man with a medical history of schizophrenia. He presented to Accident and Emergency with bilateral leg pain, swelling and erythema with no preceding history of trauma. Initially he was treated for bilateral lower leg cellulitis with a late diagnosis of compartment syndrome.
Conclusion: This case illustrates the need for a broad differential diagnosis.
Keywords: compartment syndrome; bilateral; fasciotomy; adult.
Introduction
Acute compartment syndrome is an orthopaedic surgical emergency. Compartment syndrome is difficult to diagnose, as it is not often thought of as a differential diagnosis for atraumatic leg swelling. Compartment syndrome is most commonly caused by open or closed fractures, burns, crush injury, vascular occlusion or revascularisation and iatrogenically due to plaster of paris application [1] Any cause of increased pressure in a closed myofascial space can lead to compartment syndrome resulting in tissue death, rhabdomyolysis and acute kidney injury if not recognised early [2]. An increasing number of cases are being reported termed ‘spontaneous’ compartment syndrome, whereby there is no obvious cause for the increase in pressure. Several of these reported cases have identified posture as a possible aetiology. It has been reported that horse riders sitting with hip and knee flexion leads to a reduced vascular supply to the lower leg. When dismounting the vascular supply returns resulting in a post-ischaemia reperfusion. Prolonged lithotomy position during surgery is a recognised risk factor [3-5]. Anticoagulant medication is an increasingly common cause for compartment syndrome. This can cause spontaneous bleeding with associated compartment syndrome [6].
Any patient with severe pain in a limb, which is not responding to analgesia, with no history of trauma should have a diagnosis of atraumatic compartment syndrome considered, as it is largely a clinical diagnosis. Another clinical feature is visible bulging of the fascial compartment and shiny skin. If necessary, routine laboratory investigations including creatine kinase and urinalysis may help the diagnosis rule out rhabdomyolysis. Clinical suspicion warrants consultation with the orthopaedic team and emergency fasciotomy if appropriate, decompressing the affected compartment. Delay in diagnosis and fasciotomy results in tissue necrosis. Compartment pressure measurements are indicated in patients with multiple trauma and those with a reduced glasgow coma score who are unable to provide a reliable history.
Case report
We report the case of a 58-year-old man who presented to the Emergency Department (ED) with bilateral leg pain, swelling and erythema. It had been reported by the care home staff that his mobility had decreased over the past few days secondary to the pain. The patient himself was a poor historian and we were unable to elicit the start of his symptoms but there was no history of trauma.
He was admitted under the care of the medical team the same day. A diagnosis of suspected bilateral cellulitis of the lower leg was made and he was commenced on intravenous flucloxicillin 2g QDS.
Laboratory tests on admission were: haemoglobin 13.2 g/dL, white cell count 16.8 x 109/L, sodium 122 mmol/L, potassium 3.8 mmol/L, urea 2.4 mmol/L, creatine 80 mmol/L C-reactive protein of 23 mg/L and a creatine kinase level of 6,966 IU/L.
Although compartment syndrome was not initially suspected the creatine kinase was performed as part of the accident and emergency pre-set blood profile for a patient attending with leg pain. The initial rise in creatine kinase was attributed to reduced mobility the previous day and the patients acute kidney injury.
On day 2 his renal function remained stable and his c-reactive protein had increased to 169mg/L. Interestingly his creatine kinase level had raised substantially to 33,250 IU/L. His fluid input and urine output were closely monitored and intravenous hydration continued. Daily urea and electrolytes were performed which remained static. The same treatment continued for a further 5 days, with his c-reactive protein rising further, and his creatine kinase remaining grossly elevated. Blood cultures taken were negative at 48 hours. On day 5 the general surgical team saw the patient as he had developed a distended abdomen and had clinical features of small bowel obstruction.
The general surgical consultant suspected bilateral anterolateral compartment syndrome, with secondary abdominal distension due to ileus as a result of rhabdomyolysis. An abdominal computerised tomography (CT) scan was performed which demonstrated high-grade small bowel obstruction with no identifiable cause radiologically. The patient was promptly reviewed by the orthopaedic consultant on call and a decision made to take the patient to theatre for bilateral anterolateral compartment fasciotomies and a laparotomy as a combined procedure.
Fasciotomy revealed muscle necrosis bilaterally in the antrolateral compartment. Decompression and debridement of the anterolateral compartments of both lower limbs took place. The laparotomy was negative with still no identifiable cause for the small bowel obstruction, and no evidence of bowel ischaemia.
The patient was managed in the intensive care unit postoperatively. A second-look and debridement with cutaneous approximation was performed 48 hours post-operatively. Recovery following this was uneventful, his bowel obstruction resolved and we discharged the patient after 3 weeks and rehabilitation was commenced.
Discussion
Several previous reports of atraumaic bilateral compartment syndrome have been documented, though underlying aetiology remains uncertain. Theories exist to suggest that posture and atypical limb position when maintained for long periods can cause compartment syndrome [3-11]. One case in the literature attributes bilateral anterolateral compartment syndrome to horse riding [12], and suggests the flexion of the hip and knee might obstruct vascular supply to the lower limb, and that in conjunction with ankle dorsiflexion, anterolateral compartment pressures are significantly elevated. Another position that has been documented to lead to bilateral compartment syndrome is the lithotomy position [3-5], again the flexion of the hips and knees for a prolonged period may be implicated.
Our case highlights the importance of early consideration of compartment syndrome in patients who present with atraumatic lower leg pain. It is therefore essential for the patient to be reviewed early by an experienced medical practitioner, and gain advice from the orthopaedic surgeons as early as possible if there is any suspicion. Elevated creatine kinase and acute kidney injury can be an indication of rhabdomyolysis and should be investigated as such.
We suspect that disrupted drug metabolism; resulting from interaction of antipsychotic medication and certain other medication, including simvastatin, with cytochrome P450 enzymes resulting in rapidly elevated drug plasma levels, which then lead to muscle toxicity and rhabdomyolosis. This is also combined with the lower reporting rates of pain in schizophrenic patients and the perceived higher pain threshold will result in a delayed reporting of symptoms and delayed diagnosis of compartment symdrome [13].
As documented previously, there is no substitute for a thorough history and examination by an experienced doctor who is aware of this possible diagnosis. It is also imperative that at the time of fasciotomy affected or all compartments in the limb are decompressed. We believe it therefore serves a purpose to raise awareness of this rare scenario.
Conclusion
Atraumatic bilateral antero-lateral compartment syndrome is rare. There is a documented association with antipsychotic medication. When present, it represents an orthopaedic emergency and as such needs to diagnosed and treated urgently with surgical decompression to reduce morbidity and mortality.
Clinical Message
Although a rare condition bilateral compartment syndrome needs to be diagnosed and managed urgently by the appropriate team which requires a high index of suspicion by the initial assessing doctor.
References
1. Shadgan B, Menon M, Sanders D, Berry G, Martin C, Duffy P, et al. Current thinking about acute compartment syndrome of the lower extremity. Can J Surg. 2010;53:329–334.
2. Mubarak SJ, Owen CA, Hargens AR, Garetto LP, Akeson WH. Acute compartment syndromes: diagnosis and treatment with the aid of the wick catheter. J Bone Joint Surg Am. 1978;60:1091–1095.
3. Chin KY, Hemington-Gorse SJ, Darcy CM. Bilateral well leg compartment syndrome associated with lithotomy (Lloyd Davies) position during gastrointestinal surgery: a case report and review of literature. Eplasty. 2009;9:e48
4. Simms MS, Terry TR. Well leg compartment syndrome after pelvic ad perineal surgery in the lithotomy position. Postgrad Med J. 2005;81:534–6.
5. Zappa L, Sugarbaker PH. Compartment syndrome of the leg associated with lithotomy position for cytoreductive surgery. J Surg Oncol. 2007;9:619–23.
6. Limberg RM, Dougherty C, Mallon WK. Enoxaparin-induced bleeding resulting in compartment syndrome of the thigh: a case report. J Emerg Med. 2011 Jul;41(1):e1-4. doi: 10.1016/j. jemermed.2008.04.016. Epub 2008 Nov 7.
7. Khan T, Lee GH, Alvand A, Mahaluxmivala JS. Spontaneous bilateral compartment syndrome of the legs: A case report and review of the literature. Int J Surg. 2012;3:209-211
8. Keene R, Froelich JM, Milbrandt JC, Idusuyi OB. Bilateral gluteal compartment syndrome following robotic-assisted prostatectomy. Orthopedics. 2010;33:852
9. Pfeffer SD, Halliwill JR, Warner MA. Effects of lithotomy position and external compression on lower leg muscle compartment pressure. Anesthesiology. 2001;95:632–636
10. Drey IA, Baruch H. Acute compartment syndrome of the calf presenting after prolonged decubitus position. Orthopedics. 2008;31:184
11. Ballesteros R, Garcia-Lazaro FJ, Moreno J, Chacón M, Málaga O, Lee M. Bilateral leg compartment syndrome complicating prolonged spine surgery in the kneeling position. Scholarly Res Exchange. 2009;535178
12. Naidu KS, Chin T, Harris C, Talbot S. Bilateral peroneal compartment syndrome after horse riding. Am J Emerg Med. 2009;27:901;e3–5
13. Webber MA, Mahwud W, Lightfoot JD, Shekhar A. Rhabdomyolysis and compartment syndrome with coadministration of risperidone and simvastatin. J Pscychopharmacol 2004;18(3):432-4.
| How to Cite This Article: Kapur BP, Grant M, Ramakrishnan M. A Traumatic Bilateral Anterolateral Compartment Syndrome and Subsequent small Bowel Obstruction in a Patient with Schizophrenia. Journal of Orthopaedic Case Reports 2015 April-June;5(2): 9-11. Available from: https://www.jocr.co.in/wp/2015/04/20/2250-0685-260-fulltext-2/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com