[box type=”bio”] What to Learn from this Article?[/box]
While evaluating new onset hip pain in a previous surgically managed intertrochanteric fracture, the possiblity of de-novo intracapsular fracture should be considered. And since it happens in mainly low demand elderly patients, the treatment preferably should be removal of implant and conversion to arthroplasty.
Case Report | Volume 5 | Issue 2 | JOCR April-June 2015 | Page 18-20 | Farhan Syed, Perrico Nunag, Abubakar Mustafa, Anand Pillai . DOI: 10.13107/jocr.2250-0685.263
Authors: Farhan Syed[1], Perrico Nunag[2], Abubakar Mustafa[2], Anand Pillai[2]
[1] Department of Trauma & Ortrhopaedics, Warwick Hospital. United Kingdom.
[2] Department of Trauma & Ortrhopaedics, University Hospital Of South Manchester. United Kingdom.
Address of Correspondence:
Dr. Farhan Syed, 30 Remburn Gardens, Warwick, CV345BH, United Kingdom.
E-mail: farhan.syed@doctors.net.uk
Abstract
Introduction: Sustaining an intracapsular fracture in a hip which was previously fixed with dynamic hip screw for extracapsular fracture, is a very rarely reported occurrence. We present one such case in order to discuss the presentation and management of this fracture. We have also reviewed the literature and pooled the previously reported cases to look at potential cause & risk factors.
Case Report: A 92 year old female, presented with new onset hip pain following a trivial injury. Couple of years back, she had sustained an extracapsular fracture on same side which was treated by DHS fixation. Further investigations confirmed a de-novo fracture which was treated by removal of DHS and cemented bipolar hemiarthroplasty.
Conclusion: This complication might not be as rare as earlier thought to be. All patients, especially elderly females who present with new onset hip pain following DHS fixation of their hip fracture previously must be evaluated for a de-novo intracapsular fracture. On confirmation of diagnosis, they can be treated by removal of dynamic hip screw and hemiarthroplasty as most of these are low demand elderly patients.
Keywords: Hip fractures, Extracapsular fracture, Dynamic hip screw.
Introduction
Hip fractures in elderly are cause of significant morbidity and mortality. These injuries are classified as intracapsular or extracapsular fractures, based on their relationship to hip joint capsule attachment. The treatment depends on factors like physiological age, fracture pattern & medical co-morbidities. Extracapsular fractures are most commonly treated by dynamic hip screw fixation, although there is increasing trend to use an intramedullary device for such fractures . We present a case of extracapsular hip fracture treated with Dynamic hip screw fixation, which represented 2 years later with intracapsular fracture on same side sustained following a trivial fall. We look at potential causes & review the literature for similar cases reported in the past.
Case report
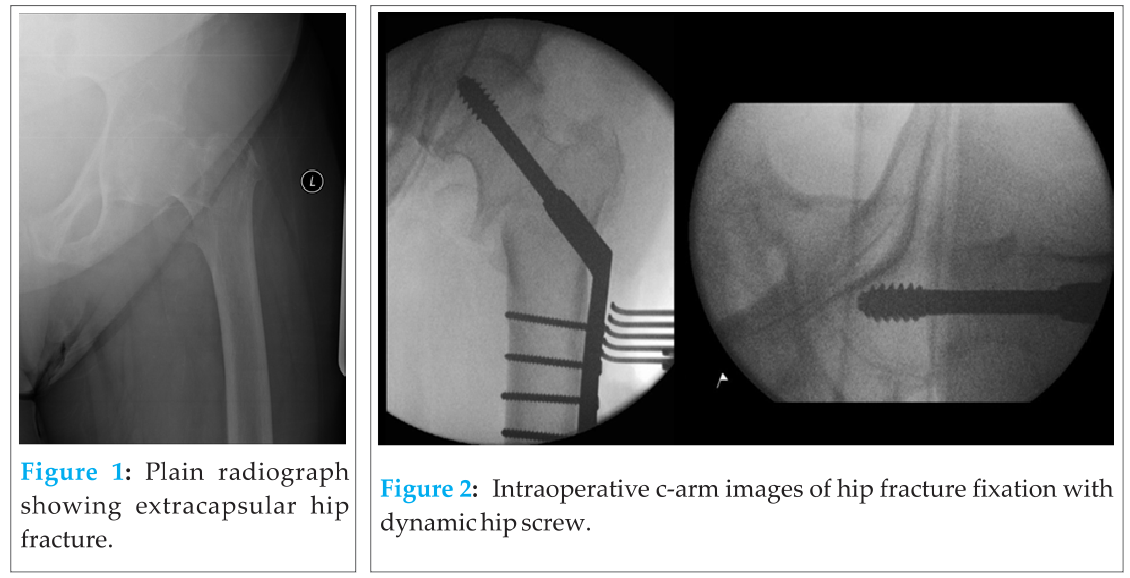
A 92 yr old lady had an unwitnessed fall and was found on the floor by her friend. Considering that she was unable to bear weight and was complaining of left hip pain, she was brought in to the A&E. She had a DHS fixation of her left hip 2 yrs back following an extracapsular fracture sustained due to a mechanical fall (Fig 1 & 2).
Clinically she was tender over her left hip and movements were painfully restricted, however there was no obvious limb deformity. Plain radiograph showed a subcapital intracapsular fracture of left hip with DHS insitu (Fig 3). She didn’t have any preexisting pain and the routine blood investigations including inflammatory markers & bone profile were unremarkable. Because of the atypical nature of fracture she was further evaluated with a CT scan of her left hip which confirmed a new intracapsular fracture (Fig 4).
Considering her age and the fact that she was a household ambulator with a zimmer frame, it was decided to treat her with removal of DHS and cemented hemiarthroplasty (figure 5). Intraoperatively, the trochantric fracture was well united and findings confirmed our radiological diagnosis of new intracapsular fracture. Intraoperatively swabs and tissues were sent off for microscopy and culture, which didn’t show any evidence of infection. Histological study of femoral head demonstrated changes suggestive of osteoporosis. The post-operative recovery was uneventful & patient returned to her baseline mobility status.
Discussion
One of the earliest case report that describes this complication was reported in 1975 . The author reported 3 such cases following a nail plate fixation. The proposed cause was trauma in an osteoporotic bone with a preexisting healed extracapsular fracture fixed with “short” nail plate. The author suggested its prevention by using a nail plate extending just short of articular surface.
Another paper published later that year reported this complication after fixation with blade plate . They suggested it occurred because of stress concentration. The prevention strategy proposed was using long blade implant, their routine removal after fracture healing and the ultimate solution being development of more biocompatible materials.
Subsequently this complication was reported with various implants like Zickel nail, Mclaughlin nail plate and Enders nail used for pertrochanteric fractures–– . Interestingly Wilson-Macdonald, who reported this complication with Mclaughlin’s nail plate , suggested that it probably occurred because of inadequate fixation, and this can potentially be avoided by using DHS & early weight bearing.
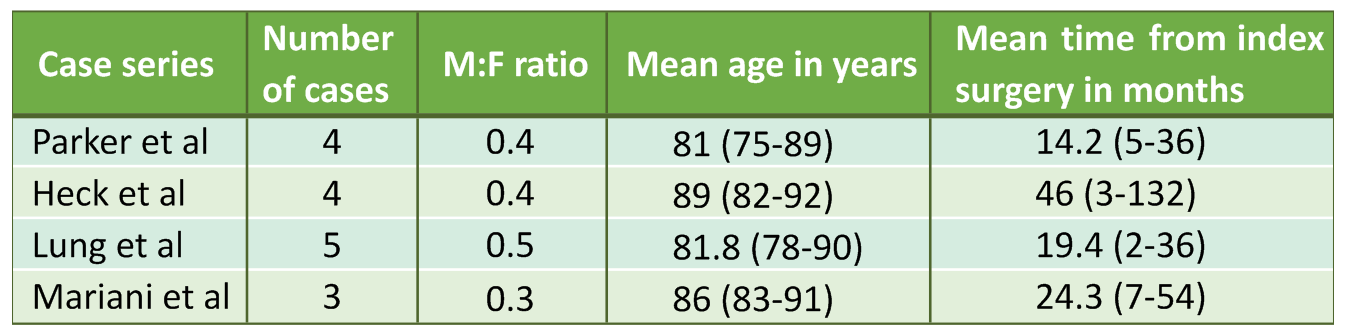
Further cases were reported even when DHS was used–– . Lombardi reported a similar case report occurring secondary to sub-clinical osteomyelitis . Relatively larger case series include 3 cases by Mariani et al 4 cases by Parker et al , 4 cases by Heck et al & 5 cases by Lung et al . Most case reports hypothesized that underlying osteoporosis along with stress concentration effect is the cause of such fractures. Some also went on to propose insertion of lag screw close to the subchondral bone (5-10mm) in order to avoid this complication. In our patient the screw tip was at 6 mm from the articular surface on AP view with a combined tip apex distance of 15mm. In most case reports, including ours, the fracture occurred at the base of the screw threads rather than at screw tip. Although there is enough evidence to suggest that Tip apex distance is the most important factor in preventing implant cut out, same can’t be extrapolated to this complication. And also to note is that our patient was on bisphonates & calcium supplementation after having sustained the first fracture.
Considering there are only case reports and small case series reporting this complication we decided to pool the available data in order to look for any risk factors. Papers from which data was analysed included Parker et al , Heck et al , Lung et al , Mariani et al and the case that we are reporting. All 17 cases were female with an average age of 84.5 years (75-92 years), at the time of diagnosis of intracapsular fracture. There was history of trauma only in 5 cases (29.5%). We need to bear in mind that these are osteoporotic fractures and the trauma patient sustained may be so trivial that they might not be able to recall it. The mean time from index surgery to second fracture was 23.4 months (2-132months). Subsequent surgery involved hemiarthroplasty in 12, THR in 2, no data available for 2, and 1 patient was deemed unfit for second surgery.
Conclusion
This complication might not be as rare as earlier thought to be. All patients, especially elderly females who present with new onset hip pain following DHS fixation of their hip fracture previously must be evaluated for a de-novo intracapsular fracture, even in absence of trauma. Computed tomography is useful imaging modality where radiographs are inconclusive. Old age, Osteoporosis and stress concentration seems to be the risk factors for these kind of fractures. Considering that most of them are low demand elderly patients, they can be treated by removal of dynamic hip screw and hemiarthroplasty.
Clinical Message
In a patient presenting with new onset hip pain following DHS fixation for extracapsular, a new intracapsular fracture should be considered besides the other obvious causes like implant cut out and OA. Based on presently available literature the causative factor is stress concentration around the tip of the implant and the predisposing factors are elderly age, osteoporosis and female sex.
References
1. Frost SA, Nguyen ND, Center JR, Eisman JA, Nguyen TV: Excess mortality attributable to hip-fracture: A relative survival analysis. Bone 2013, 56:23–29.
2. Anglen JO, Weinstein JN, American Board of Orthopaedic Surgery Research Committee: Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am 2008, 90:700–707.
3. Lee Y-K, Yoon B-H, Nho J-H, Kim K-C, Ha Y-C, Koo K-H: National trends of surgical treatment for intertrochanteric fractures in Korea. J Korean Med Sci 2013, 28:1407–1408.
4. Baker DM: Fractures of the femoral neck after healed intertrochanteric fractures: a complication of too short a nail plate fixation. Report of three cases. J Trauma 1975, 15:73–81.
5. Cameron HU, Pilliar RM, Hastings DE, Fornasier VL: Iatrogenic subcapital fracture of the hip: a new complication of intertrochanteric fractures. Clin Orthop 1975:218–220.
6. Ross PM, Kurtz N: Subcapital fracture subsequent to Zickel nail fixation: a case report. Clin Orthop 1980:131–133.
7. Wilson-MacDonald J: Subcapital fracture complicating an intertrochanteric fracture. Clin Orthop 1985:147–150.
8. Chan KM, Tse PY: Late subcapital fracture of the neck of the femur–a rare complication of Ender nailing. J Trauma 1986, 26:196–198.
9. Gogan WJ, Daum WJ, Simmons DJ, Evans EB: Subcapital fracture of the hip following an intertrochanteric fracture. A case report and literature review. Clin Orthop 1988:205–209.
10. Wolff AM, Kessler HW: Subcapital fracture after open reduction and internal fixation of an intertrochanteric fracture may be prevented. Clin Orthop 1990:308–310.
11. Blyme PJ, Iversen E, Burgaard P: Subcapital fracture of the femoral neck following internal fixation with a dynamic hip screw. Acta Orthop Belg 1990, 56:517–519.
12. DiMaio FR, Haher TR, Splain SH, Mani VJ: Stress-riser fractures of the hip after sliding screw plate fixation. Orthop Rev 1992, 21:1229–1231, 1238.
13. Fairbank AC, Ellis M, Jinnah RH: Spontaneous subcapital femoral neck fracture complicating a healed pertrochanteric fracture: aetiology and ease of diagnosis is not as previously thought. Injury 1993, 24:692–694.
14. Malkani AL, Rand JA: Subcapital femoral neck fracture following open reduction and internal fixation of an intertrochanteric hip fracture using a sliding screw and side plate. Orthop Rev 1993, 22:469–472.
15. Arrington ED, Davino NA: Subcapital femoral neck fracture after closed reduction and internal fixation of an intertrochanteric hip fracture: a case report and review of the literature. Am J Orthop Belle Mead NJ 1999, 28:517–521.
16. Lombardi LJ, Cleri DJ, Goldhagen PR, Halligan JB: Subcapital fracture complicating fixation of an intertrochanteric fracture from osteomyelitis. Orthop Rev 1994, 23:257–260.
17. Mariani EM, Rand JA: Subcapital fractures after open reduction and internal fixation of intertrochanteric fractures of the hip. Report of three cases. Clin Orthop 1989:165–168.
18. Parker MJ, Walsh ME: Importance of sliding screw position in trochanteric fracture. 4 cases of secondary cervical fracture. Acta Orthop Scand 1993, 64:73–74.
19. Heck BE, Ebraheim NA, Bielski RJ, Jackson WT: Femoral neck fracture following intertrochanteric fracture. J Arthroplasty 1996, 11:873–879.
20. Lung YT, Kam WL, Leung YF, Chung OM, Wai YL: Subcapital femoral neck fracture following successful trochanteric fracture treatment with a dynamic hip screw: a report of five cases. J Orthop Surg Hong Kong 2007, 15:238–241.
| How to Cite This Article: Syed F, Nunag P,Mustafa A, Pillai A. Ipsilateral Intracapsular Hip Fracture 2 Years after Fixation of Extracapsular Fracture by Dynamic Hip Screw. Journal of Orthopaedic Case Reports 2015 April-June;5(2): 18-20 . Available from: https://www.jocr.co.in/wp/2015/04/20/2250-0685-263-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com