[box type=”bio”] What to Learn from this Article?[/box]
Total hip arthroplasty is a good option for failed Hemirthroplasty cases though it is technically demanding. Girdlestone arthroplasty may not be considered in such situation.
Case Report | Volume 5 | Issue 2 | JOCR April-June 2015 | Page 47-49 | Purushotham VJ, Ranganath BT. DOI: 10.13107/jocr.2250-0685.272
Authors: Purushotham VJ[1], Ranganath BT[1]
[1] Assistant Professor, Department of Orthopaedics, ESICMC PGIMSR, Rajajinagar, Bangalore. India.
Address of Correspondence
Dr V.J.Purushotham
Associate Professor & HOD Orthopaedic Department, ESIC medical college, Rajajinagar Bangalore 560010.
Email:- purushotham.vj@gmail.com
Abstract
Introduction: Girdlestone hip arthroplasty, though described as a salvage procedure for infected hip joints, can also be considered for failed Hemiarthroplasty procedures. The functional results of such Girdlestone hip may not be satisfactory. They may require total hip replacement to improve the quality of life, which are technically challenging. Here we are reporting such a case in a 60 year old male patient, with review of literature.
Case Report: A 60 year old male patient underwent cemented bipolar hemiarthroplasty for fracture neck of femur which failed, owing to improper implantation. Subsequently he underwent Girdlestone arthroplasty which resulted in persistent painful hip. He presented to us in this situation, where we successfully converted the Girdlestone arthroplasty to a Total Hip arthroplasty.
Conclusion: Improper implantation in Hemiarthroplasty fails subsequently. In such cases Girdlestone arthroplasty may be an option to consider, though it may not give requisite relief to patient in some cases. In such situations total hip arthroplasty procedure, though technically challenging will give stable painless hip to the patient.
Keywords: Hemiarthroplasty; Girdlestone arthroplasty; Totalhip arthropalsty.
Introduction
Hemiarthroplasty (unipolar or bipolar) of the hip is a commonly performed procedure in elderly patients with intracapsular displaced fractures of the neck of femur with good short-term results with regard to pain relief, return to activity, morbidity and mortality [1,2,3]. An improperly implanted bipolar prosthesis creates more problems with one of the options being a Girdlestone arthroplasty. Though good relief is achievable in some cases from Girdle stone arthroplasty, in most cases the results are not satisfactory [4,5,6]. With the following treatment option we report this case of re implantation with total hip arthroplasty in Girdlestone hip.
Case report
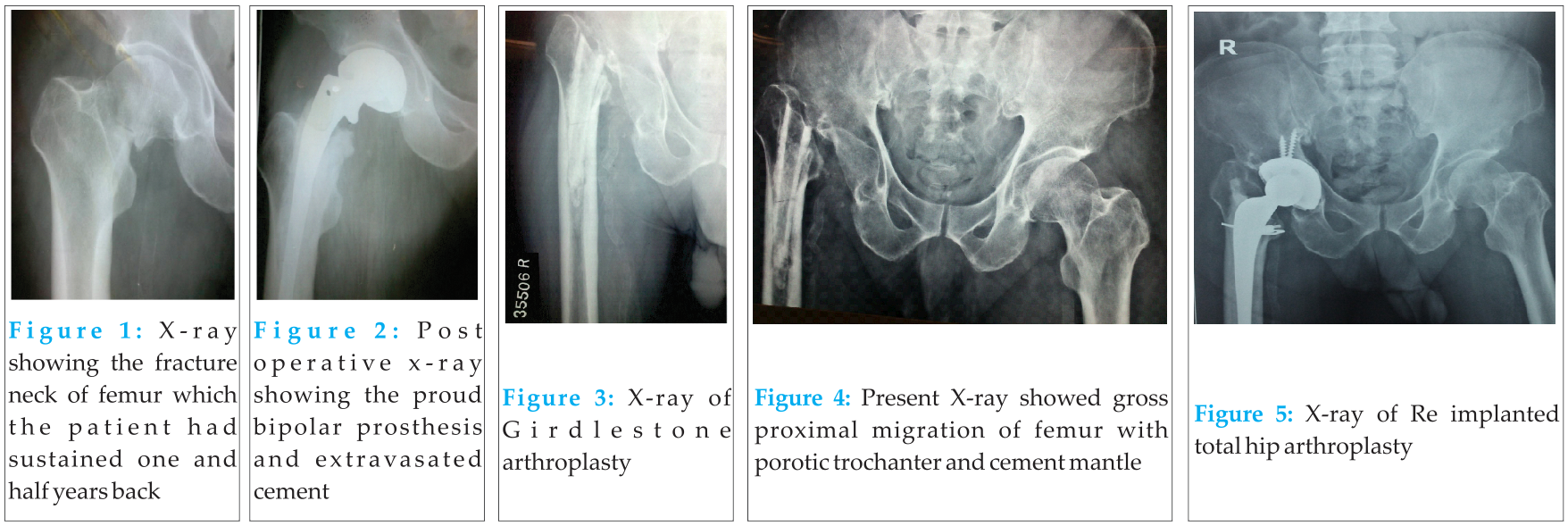
A 60 year old male patient presented to us in the outpatient department with complaints of limp and shortening of the right lower limb for the past one year. The patient had sustained fracture neck of femur following a fall while working one and half years back [Figure 1].He underwent cemented bipolar hemiarthroplasty for the same [Fig 2].The old post-operative x-rays showed a proud bipolar prosthesis with extravasations of cement from proximal femoral aspect.
The patient gave history of lengthening of the operated limb, which he noticed on day one. He had continuous dull aching pain in the right hip with stiffness for a period of six months from the day of surgery. Patient was walking with the support of a walking aid. As the pain & limp persisted, he was advised removal of bipolar prosthesis. Patient underwent the procedure of removal of improperly placed implant & Girdlestone arthroplasty [Fig 3]. Since, last one year he has been walking with pain, limp, shortening and instability. Patient had a Harris hip score of 26. The recent X-ray of the hip [Fig 4] showed gross proximal migration of femur with osteoporotic greater trochanter and cement mantle without any signs of loosening.
The patient was thoroughly investigated to rule out any signs of underlying infection. The markers of infection; CRP was negative and ESR was around 25mm at the end of one hour. The hip joint aspiration under C-arm guidance was done to rule out any infective collection which turned out to be negative. Later an MRI scan of the hip was also done to rule out any possible signs of infection.
As the patient’s intention was to have a painless joint with stability, he was advised total hip arthroplasty. With an operative plan of removal of cement mantle and total hip arthroplasty with or without extended trochanteric osteotomy, patient was posted for surgery. The standard posterior approach was used to expose the hip joint. The acetabulum was filled with hard fibrous tissue which was completely cleared and acetabular floor was prepared. Once the preparation of acetabulum was done the proximal femur was exposed without having to do the trochanteric osteotomy, the cement mantle in the proximal part of shaft was removed with some effort enblock, but the distal mantle was impacted in the shaft. The mantle was drilled with 3.2mm drill bit, to remove it in piece meal. But the peripheral part was integrated very well within the canal. The K- nail reamers of 6.0mm, 7.0mm and 8.0mm were used to gradually remove the mantle, in the attempt the antero-lateral wall of the femur was breached. The breach in the wall, which was about 6mm in diameter was identified immediately and the exposure was further extended to visualize it. The break in the cortex was used to remove the distal part of the cement mantle. Once the cement was completely removed the femoral canal was prepared. Long cemented stem was planned to bypass the cortical breach by at least 2 cortical diameters. An undisplaced split in the trochanter was stabilized using a steel cable.
The trial prosthesis was placed and reduction was attempted. It was noted that in spite of adequate soft tissue release the reduction was not achievable, unless the vertical offset was decreased. Hence a decision of placing the stem deeper in the shaft, accepting the shortening was taken & executed. Uncemented acetabular cup with a long cemented revision stem total hip arthroplasty was done [Fig 5]. An uncemented stem could not be used as the reduction was difficult, even with the smallest trial offsets.
The immediate post-operative period was uneventful and he was made to walk with support on the 3rd day. The patient is ambulant without support, without any significant pain at present though shortening of the limb of about 2.5cms is present, which is compensated by a heel raise. The latest follow up was one year after surgery. The patient was able to walk independently with the help of a stick, has mild pain on walking for more than a kilometer. The postoperative Harris hip score was 64.
Discussion
Intracapsular fracture neck of femur is one of the most common fragility fractures in the elderly. Most patients are managed by replacement with either a hemiarthroplasty or a total hip arthroplasty. An improperly implanted bipolar prosthesis would create more problems to the patient, leaving the surgeon to choose one of the options being a Girdlestone arthroplasty. Converting such painful Girdlestone hip is technically challenging.
We reviewed the literature pertaining to results of Girdlestone arthroplasty & total hip replacement in failed Girdlestone hips. There are no reports of Reimplantation of Total hip components in a case, where a failed hemi replacement is converted to a Girdlestone hip, as in our case report.
Girdlestone in both his articles in 1928 & 1942, has described radical excision of hips in tuberculosis & pyogenic infections [8]. He emphasized that the surgery involving excision of head, neck, greater trochanter & all musculatures is only for severe infections of hip joints. He concluded that if the surgery is done well the result is good with dramatic relief from the condition. In 1989 R T Muller, KF Schalgel5 endorsed this in their study where results of Girdlestone arthroplasty were good to satisfactory. Oheim et al in 2011 in their series of 27 cases opined Girdle stone arthroplasty is still an essential surgery though not functionally satisfactory [9].
However Bitter ES, Petty W in their series of 14 patients concluded that the functional results were not good following Girdlestone and the patient often needed further procedures, like fusion or replacement depending on the age of the patients [4].
In 2008, Pankaj A, Surya bhan et al in their series of 44 cases concluded that conversion of symptomatic hemiarthroplasty to total hip arthroplasty is a safe option that gives good functional results, with marginally higher rates of intra-operative complications [10].
Pradeep bhosle et al in their series of 89 cases in 2012, where Total hip replacement was performed for failed hemiarthroplasty concluded that THR is an excellent option in failed hemiathroplasty cases [11].
In 2004 Markus E Rittemeister et al in their series of 39 patients assessed the functional outcome of total hip replacement following Girdlestone hip arthroplasty. They concluded that the results were unpredictable from poor to fair hip function as evaluated with standardized hip scoring systems. In 17 cases they had to do revision surgeries. Microbiological culture, patient age, duration of Girdlestone arthroplasty and the number of preceding surgical procedures did not correlate with the functional outcome after conversion [12].
Although Girdlestone hip arthroplasty is a useful surgery, it is generally reserved for multiple failed attempts at reconstruction of the hip, generally as a result of infection or for septic and tubercular hips. The results of girdlestone hips vary from good to poor in the various studies published. Though girdlestone arthroplasty was a common surgery previously, the number of surgeries in the present date have decreased probably owing to the refusal from patients to accept an excision of the hip, improved surgical outcomes following revision hip reconstruction and decreased incidence of septic /tubercular hips.
On the other hand conversion of a long standing Girdlestone hip to a Total hip though is a well documented procedure in the literature, it is generally done for septic hips. The results mentioned in the literature are not generally uniform.. Each case has to be looked at individually and decision to offer a Total hip in such cases should be taken judiciously in consultation with the patient, after explaining pros and cons with a guarded prognosis.
Better results with total hip arthroplasty in Girdlestone hips can be expected in cases where more bone on the proximal femur can be preserved [7]. In this case where the proximal femur was completely intact was ideal for conversion to total hip arthroplasty. However the muscle strength around the hip in such cases which are operated multiple times is difficult to assess. It is important to explain guarded prognosis of the procedure beforehand to the patient.
Conclusion
The longevity of implants following hemiarthroplasty depends on its proper placement. Girdlestone arthroplasty may not give requisite functional relief to the patient. Though technically challenging, total hip arthroplasty in certain cases will give a relatively stable and painless hip, as is the observation in our case. Patient has been ambulant without pain till his last follow up of 1 year. A Long term follow up of this case may throw more information in these cases.
Clinical
Hemiarthroplasty will fail if not done properly. Converting such failed cases to Girdlestone hip arthroplasty may not be a good option. In such cases where Hemiarthroplasty has failed or subsequent Girdlestone hip arthroplasty has failed to give relief to patient, Total hip arthroplasty should be considered though it is technically demanding especially after 2 failed surgeries prior to it.
References
1. Yau WP, Chiu KY. Critical radiological analysis after Austin Moore hemiarthroplasty. Injury 2004; 35:1020-4.
2. Wachtl SW, Jacob RP, Gautier E. Ten-year patient and prosthesis survival after unipolar hip hemiarthroplasty in female patients over 70 years old. J Arthoplasty 2003; 18:587-91.
3. Clayer M, Brucknr J. The outcome of Austin-Moore hemiarthroplasty for fracture of the femoral neck. Am J Orthop 1997; 26:681-4.
4. Bittar ES, Petty W(1982) Girdlestone arthroplasty for infected total hip arthroplasty. Clin Orthop 170: 83-87.
5. Muller RT, Schlegel KF, Konermann H (1989) Long-term results of Girdlestone hip. Arch Orthop Trauma Surg 108;359-362.
6. Lenoble E, Goutallier D (1995) Replacement of infected total hip prosthesis in two stages. Int Orthop 19,151-156.
7. Witschger PM, Siegrist H. Totalprothese nach Girdlestone. Orthopäde. 1989;18 : 489-492.
8. G.R. Girdle stone; Acute pyogenic hip: an operation giving free access and effective drainage; CORR (2008) 466, 258-263
9. Oheim R. Surgical therapy of hip-joint empyema. Is the Girdlestone arthroplasty still up to date? International Orthopaedics [Int Orthop] 2012 May; Vol. 36 (5), pp. 927-33.
10. Pankaj A, Malhotra R, Bhan S. Conversion of failed hemiarthroplasty to totalhip arthroplasty: A short to mid-term follow-up study. Indian J Orthop [serial online] 2008
11. Pradeep Bhosale, Ashish Suryawanshi, and Amber Mittal ;Totalhip arthroplasty in failed aseptic Austin more prosthesis. Indian J Orthop. 2012 May-Jun; 46(3): 297–303.
12. Markus E. Rittmeister. Lilian Manthei. Nils P. Hailer ; Prosthetic replacement in secondary Girdlestone arthroplasty has an unpredictable outcome International Orthopaedics (SICOT) (2005) 29: 145–148.
| How to Cite This Article: Purushotham VJ, Ranganath BT. Total Hip Arthroplasty in a Girdlestone Hip following a Failed Hemiarthroplasty. Journal of Orthopaedic Case Reports 2015 April-June;5(2): 47-49 . Available from: https://www.jocr.co.in/wp/2015/04/20/2250-0685-272-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com