[box type=”bio”] What to Learn from this Article?[/box]
TB should be considered as a diffrential diagnosis in every case of atypical infection.
Case Report | Volume 5 | Issue 2 | JOCR April-June 2015 | Page 50-52 | Yogesh Gaikwad, Madhav Khadilkar, Ashish S. Ranade, Devendra N. Vartak. DOI: 10.13107/jocr.2250-0685.273
Authors: Yogesh Gaikwad[1], Madhav Khadilkar[1], Ashish S. Ranade[1], Devendra N. Vartak[1]
[1] Dept. of Orthopaedics, SKN Medical College, Pune 411041. Maharashtra. India.
Address of Correspondence
Dr Yogesh Gaikwad
Associate Professor, Dept. of orthopaedics, SKN Medical College, Opposite Pune Banglore High Way, Pune – 41. Maharashtra. India. Email:- yogeshrg68@gmail.com
Abstract
Introduction: A typical presentations of tuberculosis are not uncommon. Periprosthetic infection with tuberculosis after total joint replacement has well published. Tuberculosis of the elbow following open reduction internal fixation of a distal humerus fracture is extremely rare.
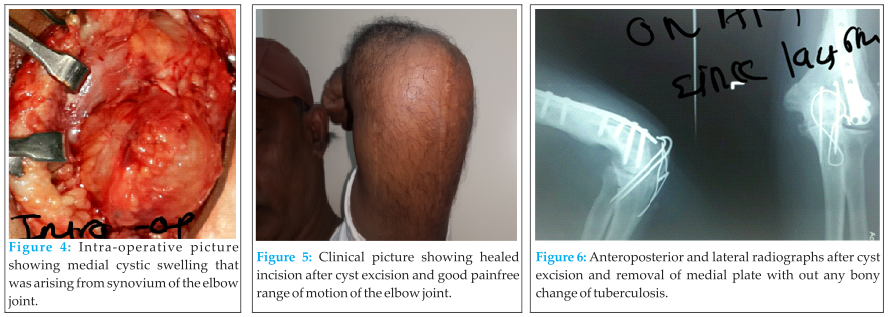
Case Report: We report case of a healthy, immunocompetenet 49-year-old male who underwent open reduction and internal fixation with bicolumnar plating for distal humerus fracture and presented after 18 month with cystic swelling over medial aspect of operated site. There was no wound dehiscence and the underlying fracture was healed well without any signs of implant loosening or bony involvement. Cystic swelling was excised and histopathology provided the diagnosis of tuberculosis. Patient was treated with anti tubercular chemotherapy and patient made uneventful recovery.
Conclusion: Although synovial tuberculosis after fracture fixation is a rare entity, tuberculosis should be kept as a differential diagnosis. Surgeons should have high index of suspicion to diagnose atypical presentations of tuberculosis.
Keywords: distal humerus fracture, elbow, open reduction internal fixation, tuberculosis, osteoarticular.
Introduction
A typical presentations of tuberculosis are not uncommon. Periprosthetic infections with tuberculosis have been reported in the past[1]. However it is very rare to find tuberculous synovitis presenting as a late complication following open reduction internal fixation of a fracture. There are only two case reports describing tuberculosis with involvement of bone after fracture fixation[2,3]. Of those that have been published on the matter, none describe tuberculosis presenting without bony involvement.
We present a rare case report of 49 year old male with cystic swelling over medial side of left elbow joint which was previously operated for fracture supracondylar humerus with bicolumnar plating one and half years ago. The cystic swelling was excised and it turned out to be tuberculous synovitis.
Case report
A 49 year old male presented with Left supracondylar humerus fracture with intercondylar extension (Fig 1). Patient had sustained this fracture following fall from steps. There was no history of clinical signs or symptoms of tuberculosis and there was no primary focus in the lungs at the time of presentation. The fracture was treated with olecrenon osteotomy and medial and lateral column plating (Fig 2). The procedure was uneventful and patient was discharged and followed up routinely. Stitches were removed on 14th post-operative day and the incision healed well. Patient resumed back his activities and remained asymptomatic. Fracture healed well without any problems. After one and half years after the index surgery, patient presented with a swelling over the medial side of operated left elbow joint. He has had swelling since one month duration. There was no history of trauma, fever, any other joint pain or any systemic symptoms. There was no tuberculous contact history in family. Physical examination showed a cystic mass measuring 5×5 cm over medial aspect of operated left elbow with mild tenderness without any erythema. There was no induration over incision site. There was no open wound or discharge. There was no neurological deficit. Movements of elbow were normal with limitation of terminal 5 degrees flexion. Plain radiograph of left elbow showed united distal humerus fracture (Fig 3) without any lysis, erosions or reduction in joint space. 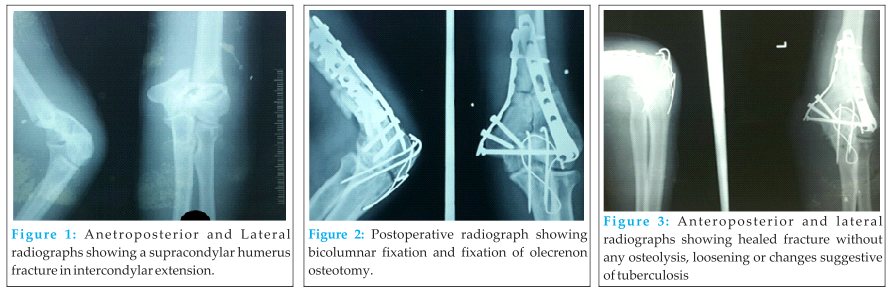
The patient was informed about the use of pertaining data for case report publication.
Discussion
Atypical presentations of osteoarticular tuberculosis are known. There are reports of tuberculosis infection following total joint arthroplasty [1, 4]. However tuberculosis following internal fixation of a fracture has been very rare [2, 3]. This case report describes a case of tuberculos synovitis after distal humerus fracture fixation.
Osteoarticular tuberculosis is characteristically a monoarticular disease and usually affects weight-bearing joints, with 10-15% being polyarticular. Non-weight bearing joints affected by tuberculosis, such as the elbow, are rarely reported in the medical literature. Tuberculous infection of the upper extremities and synovitis of the elbow joint are relatively rare and difficult to diagnose accurately at an early stage. [5,6, 7] The common diagnostic dilemma in elbow TB is due to the similarity of disease with the more common pathologies like rheumatoid arthritis, low virulence pyogenic arthritis, gout, pigmented villonodular synovitis and even sometimes neoplasms.
Tubercle bacilli tend to remain dormant following initial spread from the primary complex. The bacteria can reach implant by hematogenous spread or by local reactivation of dormant bacteria. Reduced immune response following trauma has been thought to cause reactivation of dormant bacteria at a distant focus [8,9].
Kumar et al have reported a series of five patients having skeletal tuberculosis after fracture fixation [2]. The authors found that all patients were exposed to severe trauma; all fractures were in the metaphyseal region. The range of time frame between initial surgery and diagnosis of tuberculosis was four to nine months. Our patient is different in several aspects to the patients in the series by Kumar et al. our patient was not exposed to severe trauma, there was no bony involvement and there was no loosening of implant. The longest duration between surgery and manifestation of infection was of 9 months in the series by Kumar et al. Our patient presented after 18 months from the index procedure.
In another report by Habib et al, olecrenon fracture fixation was complicated by tuberculous infection in early post-operative period. There was involvement of the bone and the implants were loose needing implant removal [3].
In our case the insidious onset of non-tender cystic swelling over medial elbow joint arising from synovium appears to be primary focus of tuberculosis because there was no evidence of TB foci elsewhere in the body. Radiological findings in osteoarticular tuberculosis are nonspecific and require aspiration or synovial biopsy for culture and histopathological examination for confirmation of diagnosis. A high degree of clinical suspicion is necessary for early diagnosis and prompt treatment so as to avoid later complication. As this case illustrates, patients with extrapulmonary tuberculosis do not always have the classic systemic symptoms associated with pulmonary tuberculosis. Also every post-operative patient with swelling at operative site may not be pyogenic infection but should be investigated thoroughly keeping in mind the differentials like tuberculosis. In addition, the blood investigations and radiographs of the joint may be normal. However, it is important to realize that these ‘normal’ findings do not rule out disease. A history of exposure to, and risk factors for, tuberculosis especially in the presence of atypical osteoarticular disease should always be considered in endemic countries.
Although tuberculosis as a late complication following open reduction internal fixation of a fracture is very rare, tuberculosis should be kept as one of the differential diagnosis.
Conclusion
Although synovial tuberculosis after fracture fixation is a rare complication, tuberculosis should be kept as a differential diagnosis. Surgeons should have high index of suspicion to diagnose atypical presentations of tuberculosis. While dealing with such cases, it is prudent to send the debrided material for histopathological examination.
Clinical
Tuberculosis should be kept as a differential diagnosis of late coplication following open reduction and internal fixation of a fracture. Surgeons should have high index of suspicion while diagnosing atypical presentations of tuberculosis.
References
1. Spinner RJ, Sexton DJ, Goldner RD, et al. Periprosthetic infections due to Mycobacterium tuberculosis in patients with no prior history of tuberculosis. J Arthroplasty 1996; 11(2):217-22.
2. Kumar S, Agarwal A., Arora A. Skeletal tuberculosis following fracture fixation. A report of five cases. J Bone Joint Surg Am 2006; 88(5): 1101-6
3. Habib M, Tanwar YS, Jaiswal A, Arya RA. Tubercular arthritis of the elbow joint following olecrenon fracture fixation and the role of TGF-beta in its pathogenesis. Chin J Traumatol 2013; 16(5):288-291.
4. Kim SJ, Kim JH. Late onset mycobacterium tuberculosis infection after total knee arthroplasty: a systematic review and pooled analysis. Scand J Infect Dis.2013; 45(12): 907-14.
5. Wang CT, Sun JS. Hou SM, Mycobacterial infections of the upper extremities. J Formos Med Assoc. 2000; 99(9):710-5.
6. Dhillon MS, Goel A, Prabhakar S, Aggarwal S, Bacchal V. Tuberculosis of the elbow: A clinicoradiological analysis. Ind J Orthop 2012; 46(2):200-5.
7. Aggarwal A, Dhammi I. Clinical and radiological presentation of tuberculosis of the elbow. Acta Orthop Belg 2006; 72(3):282-7.
8. Rodrick ML, Wood JJ, O’Mahony JB, Davis CF et al. Mechanism of immunosupression associated with severe nonthermal traumatic injuries in man: production of interlukin 1and 2. J Clin Immunol 1986; 6:310-8.
9. Lyons A, Kelly JL, Rodrick ML, Mannick JA, Lederer JA. Major injury induces increased production of interlukin- 10 by cells of the immune system with a negative impact on resistance to infection. Ann Surg. 1997; 226:450-60.
| How to Cite This Article: Gaikwad Y, Khadilkar M, Ranade AS, Vartak DN. Atypical Presentation of Tuberculosis of Elbow Joint in Operated Case of Distal Humerus Fracture. Journal of Orthopaedic Case Reports 2015 April-June;5(2): 50-52. Available from: https://www.jocr.co.in/wp/2015/04/20/2250-0685-273-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com