[box type=”bio”] What to Learn from this Article?[/box]
PVNS should be considered as one of the differentials in acute irritable knee in children. Prompt and proper treatment can lead to an excellent clinical result..
Case Report | Volume 5 | Issue 3 | JOCR July-Sep 2015 | Page 78-80 | Cheung Man Hong, Lui Tun Hing. DOI: 10.13107/jocr.2250-0685.316.
Authors: Cheung Man Hong[1], Lui Tun Hing[1]
1Department of Orthopaedics and Traumatology, North District Hospital, Sheung Shui, NT, Hong Kong SAR, China..
Address of Correspondence
Dr. Lui Tun Hing,
Department of Orthopaedics and Traumatology, North District Hospital, 9 Po Kin Road, Sheung Shui, NT, Hong Kong SAR, China.
E-Mail: luithderek@yahoo.co.uk
Abstract
Introduction: Pigmented villonodular synovitis (PVNS) is a proliferative condition of the synovium, which is composed of nodules and/or villi and has an abundant number of hemosiderin-laden macrophages.
Case Report: A 10-year-old boy presented with an acute irritable knee. Emergency arthroscopy showed a nodular PVNS in the intercondylar notch. The symptoms resolved after resection of the lesion.
Conclusion: PVNS of the knee in children is a rare entity. It can be one of the causes of acute irritable knee. Complete resection of the nodular PVNS can cure the disease.
Keywords: Pigmented villonodular synovitis, knee, nodular, irritable knee, septic arthritis.
Introduction
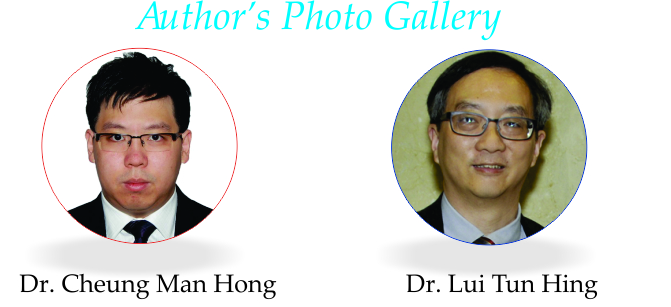
Pigmented villonodular synovitis (PVNS) is a proliferative condition of the synovium, which composed of nodules and/or villi and has an abundant number of hemosiderin-laden macrophages [1]. It is rare in children. A child with acute irritable knee mimicking infective arthritis of the knee joint was presented. Arthroscopy revealed a vascular mass with active contact bleeding, with histology confirmed a diagnosis of PVNS. The presence of hemarthrosis suggested that acute bleeding of the lesion into the joint may be the cause of such an atypical acute presentation. PVNS, although rare, should be considered as one of the differential diagnoses of an acute irritable knee presenting in children.
Case report
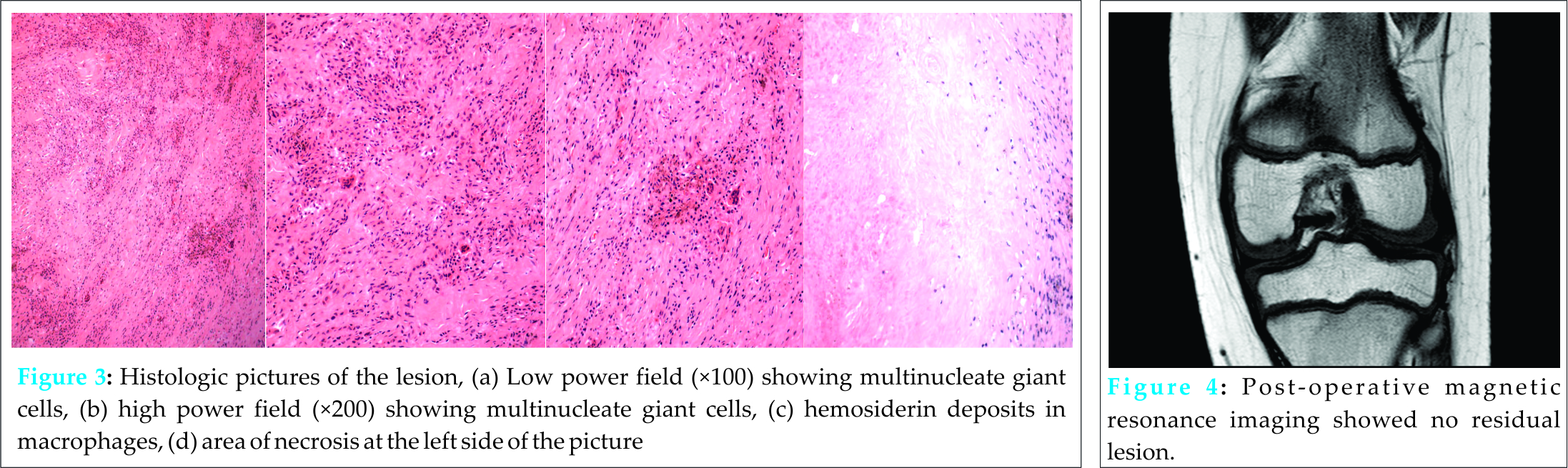
A 10-year-old boy had sudden onset of left knee pain and swelling 1-day before admission. There was no recent injury reported. He was unable to move the knee or walk due to the pain. There was no other joint pain, fever, or systemic upset. Clinical examination showed an irritable boy with marked left knee effusion. The knee joint was extremely painful with diffuse tenderness and increase in local temperature. The joint was not erythematous. The range of movement of the knee was markedly limited from 30° to 40°. Knee aspiration yielded 40 ml of blood-stained fluid. Radiographs of the knee showed local soft tissue swelling without any bone lesion (Fig. 1). 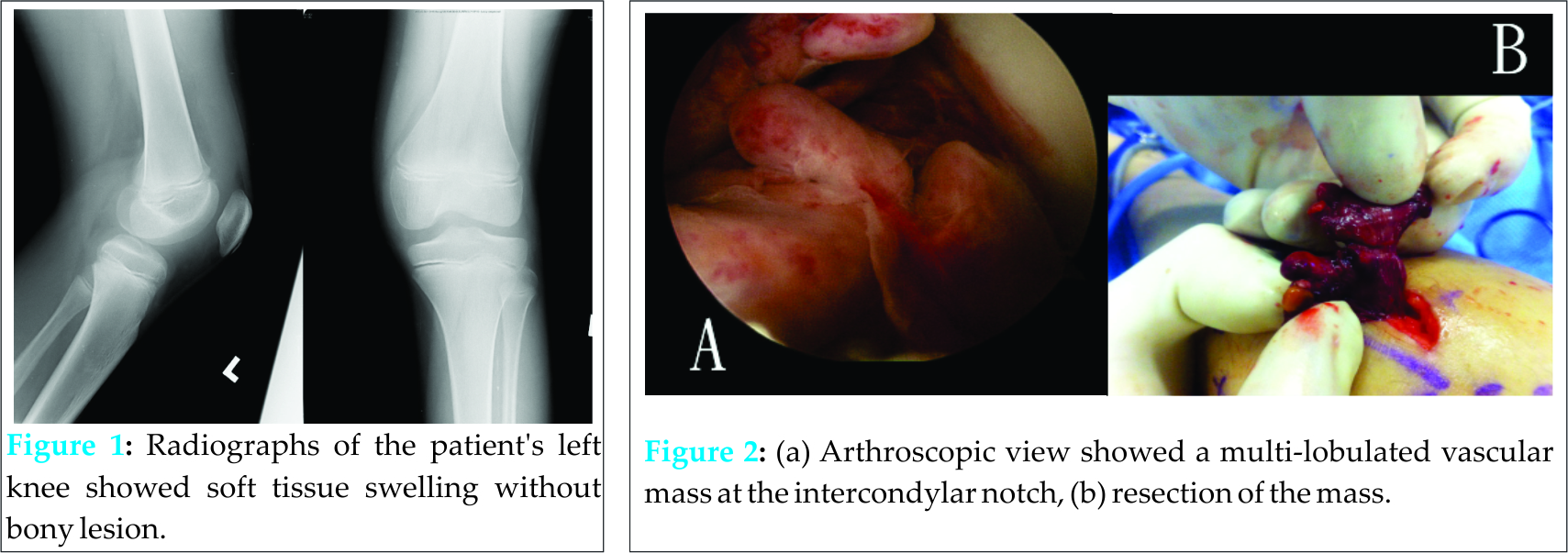
Discussion
Acute, non-traumatic, irritable knee in children is not uncommon in daily practice. The presence of effusion should alert the physician to a diagnosis of infective arthritis and consideration of arthrocentesis. Other differential diagnoses include reactive arthritis, transient synovitis, hemophilia, inflammatory arthritis, and malignancy, e.g., leukemia. The common causes of inflammatory arthritis include rheumatic fever, Reiters syndrome and vasculitis (e.g. Henoch-Schonlein Purpura) [2]. To the best of our knowledge, our patient is the first case in English literature in which PVNS presented as an acute irritable knee.
First described by Jaffa et al. in 1941, PVNS is a rare inflammatory granulomatous condition of unknown etiology [3]. It can classified into diffuse or localized/nodular type, with knee joint being the most commonly affected joint. The World Health Organization classification now defines localized PVNS under the group of giant cell tumor of the tendon sheath, which encompasses a group of lesion arising from the synovium of joints, bursae, and tendon sheath. While diffuse PVNS with diffuse intra-articular involvement is under the group of diffuse-type giant cell tumor [4]. PVNS has estimated the incidence of 1.8 per million [5]. It is even rarer in children and has only been presented as a case report or small case series [6-10]. Among the reported cases, there was a considerable delay in diagnosis and subsequent surgery. The delay ranged from a few months to more than 1-year [6]. The typical presentation was that of a child presenting with chronic recurrent knee pain or swelling, who had sought multiple medical workup. Not until a magnetic resonance imaging (MRI) or arthroscopy examination was the diagnostic opinion confirmed. Delay in diagnosis has been shown to be a risk factor of future morbidity [6]. Moreover, the diffuse PVNS usually presented with insidious onset of pain, swelling, and stiffness in the involved joint; while the local PVNS more commonly presented with locking, catching, and instability [11-16]. The clinical presentation of our case was atypical. The patient presented with acute irritable and swollen knee, which clinically was highly suggestive of infective arthritis. In our practice, MRI is not readily available in such an acute setting. Under such clinical scenario, emergency arthroscopy is a justified choice for early diagnosis and treatment of the suspected infection, as a delay in treatment of septic arthritis can lead to the long-term morbidity of the patient. As a result, emergency arthroscopy was arranged, ultimately revealing the causative pathology. Fortunately, a complete excision of the lesion was achieved which lead to complete recovery. To the best of our knowledge, this is the first reported case of PVNS mimicking infective arthritis in children. Only one similar case has been reported in an adult, in which a pregnant patient presented with acute knee arthritis mimicking infective arthritis [17]. Microscopic evaluation revealed hemorrhage and necrosis, which may suggest torsion or bleeding of the tumor as the cause of the acute symptom. Area of necrosis was also noted in the lesion in our case. Since the stalk of the lesion was quite narrow, this might suggest acute torsion or strangulation of the lesion as the cause of the acute severe knee pain. The lesion was noted to be quite vascular with contact bleeding during arthroscopic manipulation. Together with the presence of hemarthrosis, this might suggest an episode of spontaneous hemorrhage from the lesion into the joint leading to acute massive hemarthrosis, which can mimic clinically an infective arthritis. The treatment of pediatric PNVS of the knee follows that of the adult counterparts. For the local/nodular form of PVNS in adult, it is well-reported in many studies that local excision can lead to excellent or very good result with complete and persistent regression of the pathology [18-21]. Although no comprehensive data are available for the pediatric group in view of the small case load, the similar result has been obtained from the available literature [6-9].
Concerning the diffuse type of PVNS, studies from the adult age group had shown a higher risk of recurrence and morbidity [19,22]. Subtotal or total synovectomy, either arthroscopic or open, can reduce the risk of recurrence [19,23,24]. In contrary to adult, the role of radiotherapy as an adjunctive therapy is not recommended in children in view of potential damage of epiphyseal growth plate and post-radiation sarcomas [25,26].
Conclusion
PVNS of the knee in children is a rare entity. It can be one of the causes of acute irritable knee. Complete resection of the nodular PVNS can cure the disease.
Clinical Message
PVNS, although rare, should be considered as one of the differentials in acute irritable knee in children. Prompt and proper treatment can lead to an excellent clinical result..
Reference
1. Durr HR, Stabler A, Maier M, Refior HJ. Pigmented villonodular synovitis: Review of 20 cases. J Rheumatol 2001;28(7):1620-1630.
2. Clinical Practice Guidelines on The Acutely swollen joint. The Royal Chldren’s Hospital Melbourne webpage. URL:
http://www.rch.org.au/clinicalguide/guideline_index/The_Acutely_Swollen_Joint/.
3. Jaffa HL, Lichstenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol 1941;31:731-65.
4. Fletcher CD, Unni KK, Mertens F. World Health Organization. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon: IARC Press; 2002.
5. Rao AS, Vigorita VJ. Pigmented villonodular synovitis (giant-cell tumor of the tendon sheath and synovial membrane). A review of eighty-one cases. J Bone Joint Surg Am 1984;66(1):76-94.
6. Baroni E, Russo BD, Masquijo JJ, Bassini O, Miscione H. Pigmented villonodular synovitis of the knee in skeletally immature patients. J Child Orthop 2010;4(2):123-127.
7. Neubauer P, Weber AK, Miller NH, McCarthy EF. Pigmented villonodular synovitis in children: A report of six cases and review of the literature. Iowa Orthop J 2007;27:90-94.
8. Van Emelen K, Moens P, Wouters K, Fabry G. Villonodular synovitis of the knee in a 5-year-old child. Apropos of a case. Rev Chir Orthop Reparatrice Appar Mot 1999;85:621-626.
9. Maric D. Pigmented villonodular synovitis of the knee in a child – Case report. Arch Onco 2004;12:75-77.
10. Pannier S, Odent T, Milet A, Lambot-Juhan K, Glorion C. Pigmented villonodular synovitis in children: Review of six cases. Rev Chir Orthop Reparatrice Appar Mot 2008;94(1):64-72.
11. Tyler WK, Vidal AF, Williams RJ, Healey JH. Pigmented villonodular synovitis. J Am Acad Orthop Surg 2006;14(6):376-385.
12. Flandry F, Hughston JC. Pigmented villonodular synovitis. J Bone Joint Surg Am 1987;69(6):942-949.
13. Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59(3):223-238.
14. Granowitz SP, D’Antonio J, Mankin HL. The pathogenesis and long-term end results of pigmented villonodular synovitis. Clin Orthop Relat Res 1976;335-351.
15. Asik M, Eralp L, Altinel L, Cetik O. Localized pigmented villonodular synovitis of the knee. Arthroscopy 2001;17:E23.
16. Delcogliano A, Galli M, Menghi A, Belli P. Localized pigmented villonodular synovitis of the knee: Report of two cases of fat pad involvement. Arthroscopy 1998;14(5):527-531.
17. Uslu M, Cetik O, Atasoy P, Eksioglu F, Engin M. Localized pigmented villonodular synovitis of the knee: Acute onset in pregnancy. Rheumatol Int 2006;26(11):1054-1056.
18. Kim SJ, Shin SJ, Choi NH, Choo ET. Arthroscopic treatment for localized pigmented villonodular synovitis of the knee. Clin Orthop Relat Res 2000;224-230.
19. De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy 2003;19(6):602-607.
20. Dines JS, DeBerardino TM, Wells JL, Dodson CC, Shindle M, DiCarlo EF, et al. Long-term follow-up of surgically treated localized pigmented villonodular synovitis of the knee. Arthroscopy 2007;23(9):930-937.
21. Akgün I, Ogüt T, Kesmezacar H, Dervisoglu S. Localized pigmented villonodular synovitis of the knee. Orthopedics 2003;26(11):1131-1135.
22. Jain JK, Vidyasagar JV, Sagar R, Patel H, Chetan ML, Bajaj A. Arthroscopic synovectomy in pigmented villonodular synovitis of the knee: Clinical series and outcome. Int Orthop 2013;37(12):2363-2369.
23. Chin KR, Barr SJ, Winalski C, Zurakowski D, Brick GW. Treatment of advanced primary and recurrent diffuse pigmented villonodular synovitis of the knee. J Bone Joint Surg Am 2002;84-A(12):2192-2202.
24. Nakahara H, Matsuda S, Harimaya K, Sakamoto A, Matsumoto Y, Okazaki K, et al. Clinical results of open synovectomy for treatment of diffuse pigmented villonodular synovitis of the knee: Case series and review of literature. Knee 2012;19(5):684-687.
25. Bruns J, Schubert T, Eggers-Stroeder G. Pigmented villonodular synovitis in children. A case report. Arch Orthop Trauma Surg 1993;112(3):148-151.
26. Park G, Kim YS, Kim JH, Lee SW, Song SY, Choi EK, et al. Low-dose external beam radiotherapy as a postoperative treatment for patients with diffuse pigmented villonodular synovitis of the knee: 4 recurrences in 23 patients followed for mean 9 years. Acta Orthop 2012;83(3):256-260.
| How to Cite This Article: Cheung Man Hong, Lui Tun Hing.Acute Knee Pain in a Child Due to Pigmented Villonodular Synovitis. Journal of Orthopaedic Case Reports 2015 July – Sep;5(3): 78-80 . Available from: https://www.jocr.co.in/wp/2015/07/10/2250-0685-316-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com