[box type=”bio”] What to Learn from this Article?[/box]
CT scans and pelvic binders remain crucial in the management of trauma patients. Pelvic binders can achieve a near anatomical level of reduction of unstable injuries, making their radiographic signs more subtle and easier to miss.
Case Report | Volume 6 | Issue 1 | JOCR Jan-Mar 2016 | Page 44-47 | James Fletcher, George Yerimah, Gorav Datta DOI: 10.13107/jocr.2250-0685.374
Authors: James Fletcher[1], George Yerimah[2], Gorav Datta[2]
[1] Department of Orthopaedics, Musgrove Park Hospital, Taunton.
[2] Department of Trauma & Orthopaedic Surgery, University Hospital Southampton, Tremona Road, Southampton.
Address of Correspondence
Mr. James Fletcher,
Registrar in Trauma & Orthopaedic Surgery, Musgrove Park Hospital, Taunton. Email: jwa.fletcher@doctors.net.uk
Abstract
Introduction: Pelvic injuries are common in high energy trauma. It is now a standard practice to reduce the potential space for haemorrhage with the use of pelvic binders and slings in the resuscitative scenario as this has been shown to reduce mortality. Most trauma centres have CT based trauma protocols so that alongside increased awareness of pelvic injuries, there is a higher detection rate of pelvic fractures.
Case Report: We present two cases of high energy pelvic injuries that were missed on initial presentation. In both the instances, pelvic binders were applied with the level of anatomical reduction being achieved meaning that pelvic injuries were missed on the initial CT scan reports.
Conclusion: CT scans continue to be an essential tool in the management of trauma, especially with regards to pelvic injuries. The increased availability and improvements in imaging techniques has confirmed CT scans as an important tool in the detection of life threatening injuries, resulting in a marked reduction in the overall number of pelvic fractures missed. However, these cases highlight the fact that the orthopaedic surgeon should not reply on an essentially ‘normal’ CT scan report and when possible, one must perform an accurate clinical assessment of the patient with the involvement a pelvic specialist at an early stage if there is any suspicion of a pelvic injury. Repeated reporting of the initial CT scan additionally reduces the incidence of missed injuries.
Keywords: Pelvic fracture, Trauma, Missed injuries, Pelvic binder.
Introduction
Pelvic fractures constitute about 3-6% of all fractures in adults and occur in up to 20% of all polytrauma cases [1]. They have an overall mortality between 6.4% to 30% which rises to 40-60% when associated with significant pelvic haemorrhage [2]. Given the adjacent anatomy, haemorrhage, often as a result of disruption of the pre-sacral and paravesical venous plexus, is the most common and life threatening complication (80% of such complications) associated with pelvic injuries [3,4].
Given the high mortality associated with pelvic injuries, it is now standard practice to reduce the potential space for pelvic haemorrhage with the use of pelvic binders and slings in the resuscitative scenario [4]. The advent of this practice alongside increased awareness of pelvic injuries is credited with the reduction in mortality seen in recent decades [5-10]. Further to this, greater access to whole body CT scans have contributed to the higher detection rates that are observed with most trauma centres implementing CT based trauma protocols [5,11].
CT scans are very sensitive at detecting subtle pelvic fractures and displacements that are commonly missed on pelvic radiographs [12]. However, the use of pelvic binders can reduce fractures sufficiently well to make even these subtle signs hard to diagnose, especially during the first ‘hot’ report performed by the radiologist. The incidence of missed injuries following CT scans ranges from 1.3% to 47% [13] and these omissions have been shown to increase the morbidity, mortality and costs associated with trauma [14-18].
We report two cases where the use of pelvic binders contributed to the failure in reporting significant pelvic injuries on trauma CT scans due to the near anatomical reduction that was achieved.
Case Report 1
A 55 year-old cyclist lost control of his bicycle and fell into the path of an oncoming car. He was managed according to the advanced trauma life support (ATLS) protocol, including triple immobilisation and the application of a pelvic binder prior to transfer to the regional trauma centre. With the completion of primary and secondary surveys, this demonstrated no more than significant superficial bruising across his anterior chest, abdomen and pelvis. An urgent trauma CT was undertaken with the pelvic binder remaining insitu.
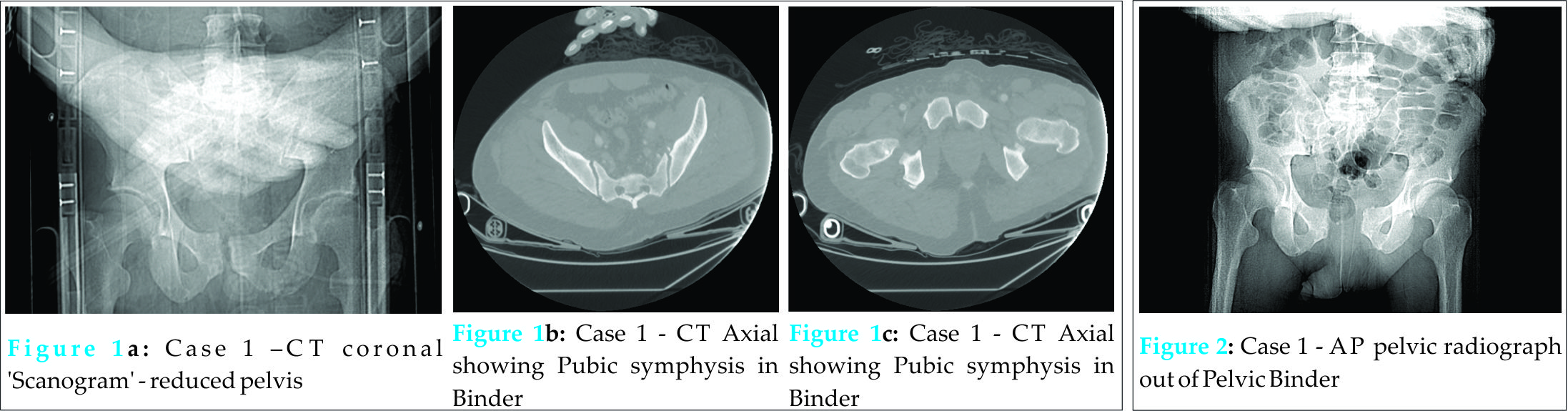
His initial CT scan reported his injuries as bilateral lung contusions, a left L5 transverse fracture, left lower rib fractures, some soft tissue swelling on the anterior abdominal wall along the right lateral pelvis with no abdominal bleed, no pelvic bony injury (Figs. 1a, 1b and 1c) and no solid organ damage. Once his cervical spine was clinically and radiographically cleared, the pelvic binder was removed and he was sat up. He complained of lower back and left hip pain, which was attributed to the transverse process fracture and extensive bruising. However, following transfer to an orthopaedic ward his left hip pain continued despite analgesia with marked tenderness being found on left hip examination.
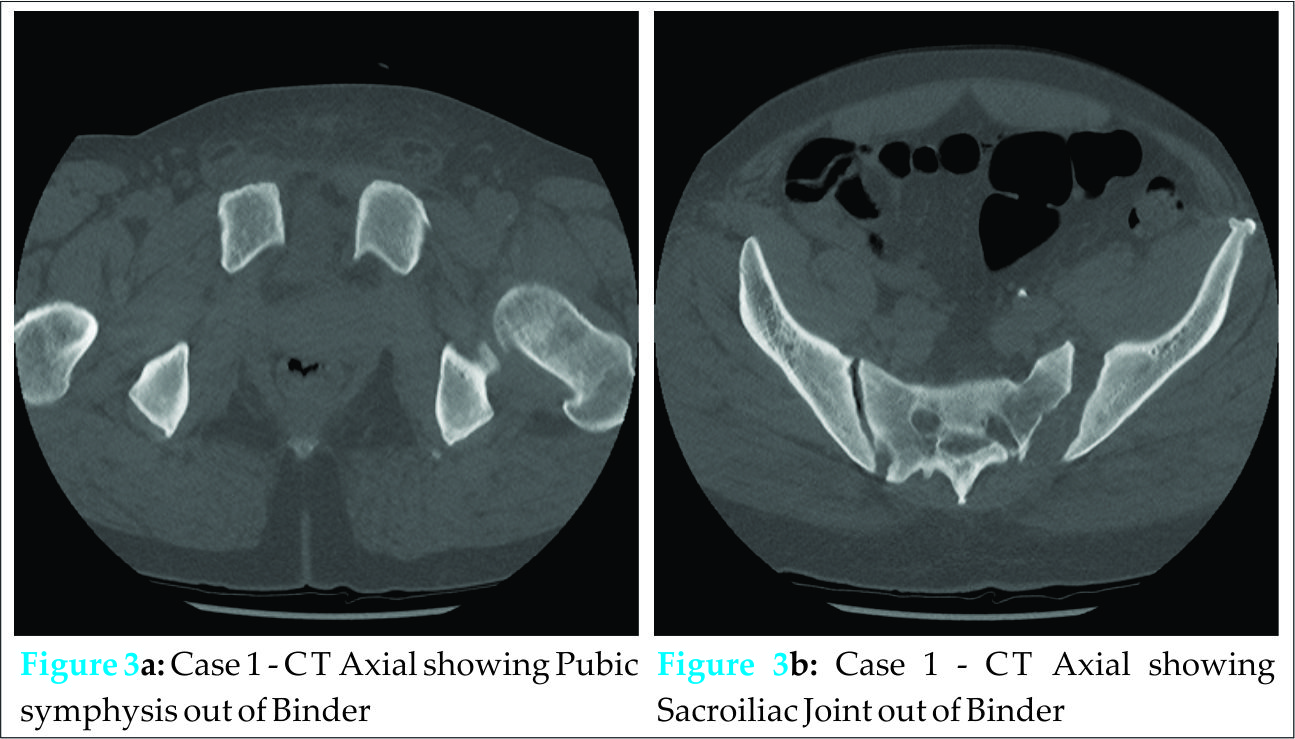
A pelvic radiograph was performed (Fig. 2) that showed diastasis of the pubic symphysis with an open sacroiliac joint on the left. His initial CT images were reviewed and a repeat pelvic CT was performed, which confirmed the radiographic findings (Figs. 3a and 3b).
Subsequently, he underwent open reduction and internal fixation and percutaneous iliosacral screws four days following admission.
Case Report 2
A 54-year-old male, was a motorcyclist versus car at a combined speed of 60mph. He was managed using the ATLS protocols and was transferred directly to the regional trauma centre. His assessments demonstrated superficial facial bruising with significant bruising and tenderness over the right clavicle with demonstrable crepitus. He also had blood around the external urethral meatus associated with a scrotal haematoma, tenderness over T6 with an obvious bony deformity and associated distal complete neurological deficit.
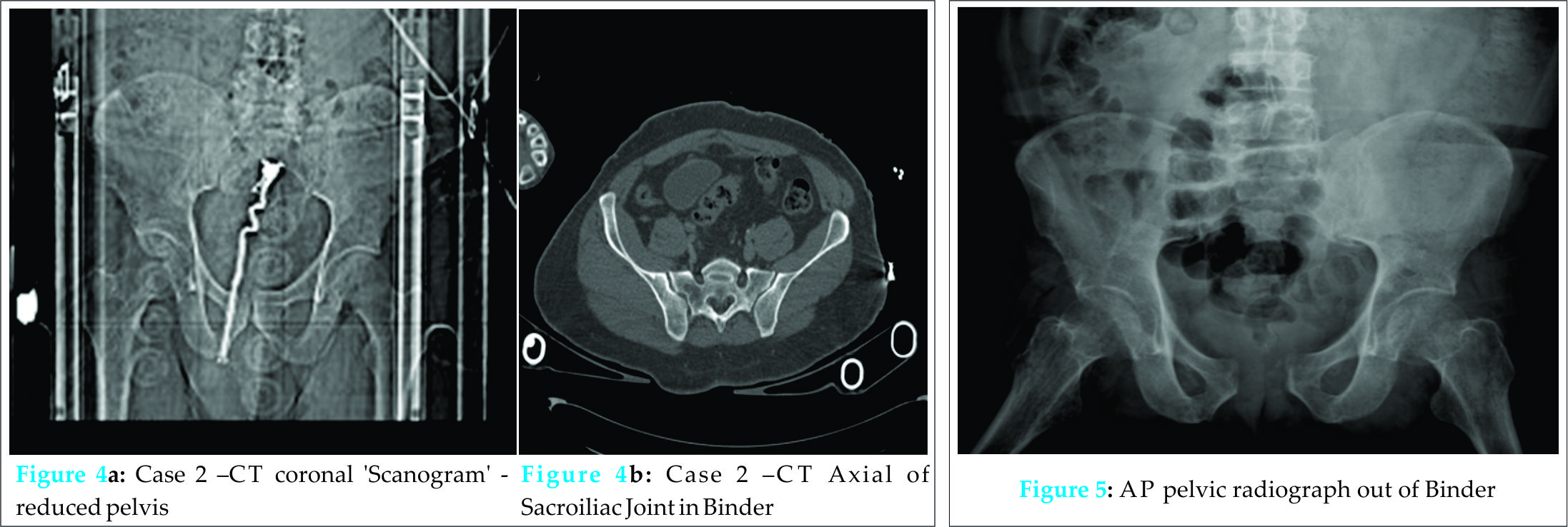
A trauma CT was performed, which showed multiple vertebral fractures at C1, T4 and T6. The worst was at the level of T6 with extensive damage to the pedicles and intervertebral discs. The CT was reported as no solid organ damage, vascular damage nor pelvic bony injury (Figs. 4a and 4b). His pelvic binder was removed, though he remained triple immobilised due to his spinal injury. When he was stable he was admitted to the high dependency neurosurgical ward and a MRI showed narrowing of the vertebral canal at T5 and T6 without cord compression. The cord was swollen and oedematous at both levels in keeping with an acute cord injury; his spinal fractures were managed non-operatively. He was transferred to a spinal rehabilitation unit for on-going management due to his neurological deficit. Fig. 5 – Case 2 – AP pelvic radiograph out of Binder At a 3 month spinal follow up appointment, a plain radiograph of his spine was repeated which showed widening of the pubic symphysis. Plain pelvic radiography showed this widening with a widened left sacroiliac joint (Fig. 5); injuries that were missed on his initial assessments.
Following discussion with the patient, especially regarding his mobility as he had not had neurological return below T6, his pelvic injuries were managed non-operatively.
Discussion
The trauma CT continues to be an essential tool in the management of trauma emergencies [12]. The increase in 24 hr availability and improved imaging techniques has made it an important imaging tool in the detection of life threatening injuries, additionally resulting in a marked reduction in the number of pelvic fractures missed [1]. With CT scans, it is easier to assess spatial fragments and three-dimensional images can be reformatted [12] and thus allow for subtle fractures and displacements not appreciated on radiographs to become more apparent. In this report, both patients had significant injuries that were very effectively reduced by the pelvic binders. Due to the high mortality associated with haemorrhage in pelvic fractures [19], there is an appropriate reluctance to remove a pelvic binder by emergency department staff for fear of dislodging a thrombus; hence most patients will and, if there are concerns of a pelvic injury, should have a CT with the pelvic binder in situ.
Whilst these are excellent examples of the benefits of well-placed pelvic binders in reducing and stabilising pelvic injuries, their use and the CT reports contributed to the delayed in diagnosing them.These patients both sustained Anterior-Posterior Compression type III (Young-Burgess Classification) fractures [20] with resultant pelvic instability and, whilst not in these cases, these fracture patterns have increased transfusion requirements and can lead to life threatening haemorrhage [21]. In one of the patients the recognition of the pelvic fracture led to a change in the management requiring urgent surgery, whilst in the second patient, given his paraplegic and delayed diagnosis, he was treated conservatively.
Conclusion
In both the cases, initial CT reports regarding the pelvis were reported as normal, but to the expert eye there were signs of pelvic injuries, namely very minimal displacement of the symphysis (in both cases) and an L5 transverse process fractured in case one. Alone, these are not very specific findings, but when they are complimented with systematic assessment and clinical suspicion it can lead to less of such cases being missed. Indeed, the presence of a L5 transverse process fracture has been shown to correlate with an increased relative risk of 2.5 for an unstable pelvic fracture [22]. Clinical examination in polytrauma patient is often of limited relevance due to the frequently encountered obtunded or comatose status of the patient and thus there is more reliance on imaging to guide management [11]. These cases show that it is essential not to rely on a ‘normal’ CT scan report but that further assessment of the CT scan should be undertaken once the patient is stabilised to ensure that injuries are not missed in the heat of the moment. When possible, one must perform an accurate clinical assessment of the patient and involve a pelvic specialist at an early stage if there is any suspicion of a pelvic injury. Repeat radiography is also a valuable tool in confirming diagnosis and clarifying appropriate management plans.
Clinical Message
Pelvic binders have a crucial, life-saving role in trauma situations, however interpretation of pelvic imaging with them insitu must involve a higher degree of suspicion for unstable injuries given the near anatomical reduction that can be achieved.
References
1. Gänsslen, A, Pohlemann, T, Paul, C, Lobenhoffer P & Tscherne, H. Epidemiology of pelvic ring injuries. Injury 1996;27(1):13-20.
2. Moreno, C, Moore E E, Rosenberger A & Cleveland H C Hemorrhage associated with major pelvic fracture: a multispecialty challenge. J. Trauma 1986;26:987-994.
3. Wubben R C. Mortality rate of pelvic fracture patients. Wis. Med. J. 1996;95:702-704.
4. Scheid D, Kellam J & Tile M. Open reduction and internal fixation of pelvic ring fractures. J Orthop Trauma. 1991;5:112.
5. Rockwood C J, Green D, Bucholz R & Heckman J. Fractures in Adults. (Lippincott, 1996).
6. Biffl W L, Harrington D T & Cioffi W G. Implementation of a tertiary trauma survey decreases missed injuries. J. Trauma 2003;54:38-43. 7. Ball C G. et al. Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J. Trauma 2005;59:917-924. 8. Huber-Wagner S. et al. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet Lond. Engl. 2009;373:1455-1461.
9. MacKenzie E. J. et al. A national evaluation of the effect of trauma-center care on mortality. N. Engl. J. Med. 2006;354:366-378.
10. American College of Surgeons & Committee on Trauma. ATLS, advanced trauma life support for doctors. American College of Surgeons 2008.
11. Eurin M. et al. Incidence and predictors of missed injuries in trauma patients in the initial hot report of whole-body CT scan. Injury 2012;43:73-77.
12. Reiger M, Knollman F & Coakley F. In Multi-slice CT: Principles and protocols Saunders Elsevier 2006;221–239.
13. Geyer L L et al. Incidence of delayed and missed diagnoses in whole-body multidetector CT in patients with multiple injuries after trauma. Acta Radiol.2013;54:592-598.
14. Brooks A, Holroyd B & Riley B. Missed injury in major trauma patients. Injury 2004;35:407-410.
15. Buduhan G & McRitchie D I. Missed injuries in patients with multiple trauma. J. Trauma 2000;49:600-605.
16. Gruen R L, Jurkovich G J, McIntyre L K, Foy H M & Maier R V. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann. Surg. 2006;244:371-380.
17. Houshian S, Larsen M S & Holm C. Missed injuries in a level I trauma center. J. Trauma 2002;52:715-719.
18. Robertson R et al. Missed injuries in a rural area trauma center. Am. J. Surg. 1996;172:564-567.
19. Pereira S J et al. Dynamic helical computed tomography scan accurately detects hemorrhage in patients with pelvic fracture. Surgery 2000;128:678-685.
20. Young J W, Burgess A R, Brumback R J & Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology 1986;160:445-451.
21. Manson T et al. Young-Burgess Classification of Pelvic Ring Fractures: Does It Predict Mortality, Transfusion Requirements, and Non-orthopaedic Injuries? J. Orthop. Trauma 2010;24:603-609.
22. Starks I, Frost A, Wall P & Lim J. Is a fracture of the transverse process of L5 a predictor of pelvic fracture instability? Bone Jt. Jr. 2011;93(B):967-969.
| How to Cite This Article: Fletcher J, Yerimah G, Datta G. The False Security of Pelvic Binders: 2 Cases of Missed Injuries due to Anatomical Reduction. Journal of Orthopaedic Case Reports 2016 Jan-Mar;6(1): 44-47. Available from: https://www.jocr.co.in/wp/2016/01/02/2250-0685-374-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com