[box type=”bio”] What to Learn from this Article?[/box]
Posterolateral rotary knee dislocation is a rare orthopedic injury that is considered to be irreducible by closed reduction. However, we experienced a case of posterolateral rotary knee dislocation reduced and reproduced by closed manipulation. We considered the mechanism of posterolateral knee dislocation as valgus and external rotation stress during knee flexion.
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 20-23 | Satoshi Tateda, Atsushi Takahashi, Toshimi Aizawa, Jutaro Umehara. DOI: 10.13107/jocr.2250-0685.412
Authors: Satoshi Tateda[1], Atsushi Takahashi[1], Toshimi Aizawa[1], Jutaro Umehara[2]
[1] Department of Orthopaedic Surgery, Tohoku University Graduate School of Medicine. Japan.
[2] Omagari Orthopaedic Clinic. Japan.
Address of Correspondence
Dr. Satoshi Tateda,
Department of Orthopaedic Surgery, Tohoku University Graduate School of Medicine. Japan.
E-mail: tateda3104@gmail.com
Abstract
Introduction: Posterolateral rotary knee dislocation is a rare orthopedic injury that is considered to be irreducible by closed reduction because of soft tissue incarceration. Here, we present a case of posterolateral rotary knee dislocation, which was reduced by closed manipulation.
Case report: The patientwas a 33-year-old man who sustained a twisting injury to his right knee that was diagnosed as posterolateral rotary knee dislocation by plain radiographs and the characteristic physical finding known as a dimple sign. Under general anesthesia, the knee dislocation was reduced by closed manipulation with internal rotation of the lower leg at knee flexion and reproduced by valgus and external rotation stress. There were was complete tear of posterior cruciate ligament, and partial tear of the anterior cruciate ligament which were not reconstructed. The medial collateral ligament that was detached from the femoral footprint was repaired. One year postoperatively, the range of motion was 0–145°. There was no knee symptom and no ligament instability.
Conclusion: This is the first report of a successful closed reduction for posterolateral knee dislocation. The mechanism of dislocation was considered valgus and external rotation stress during knee flexion.
Key words: Posterolateral knee dislocation, Closed reduction, Injury mechanism.
Introduction
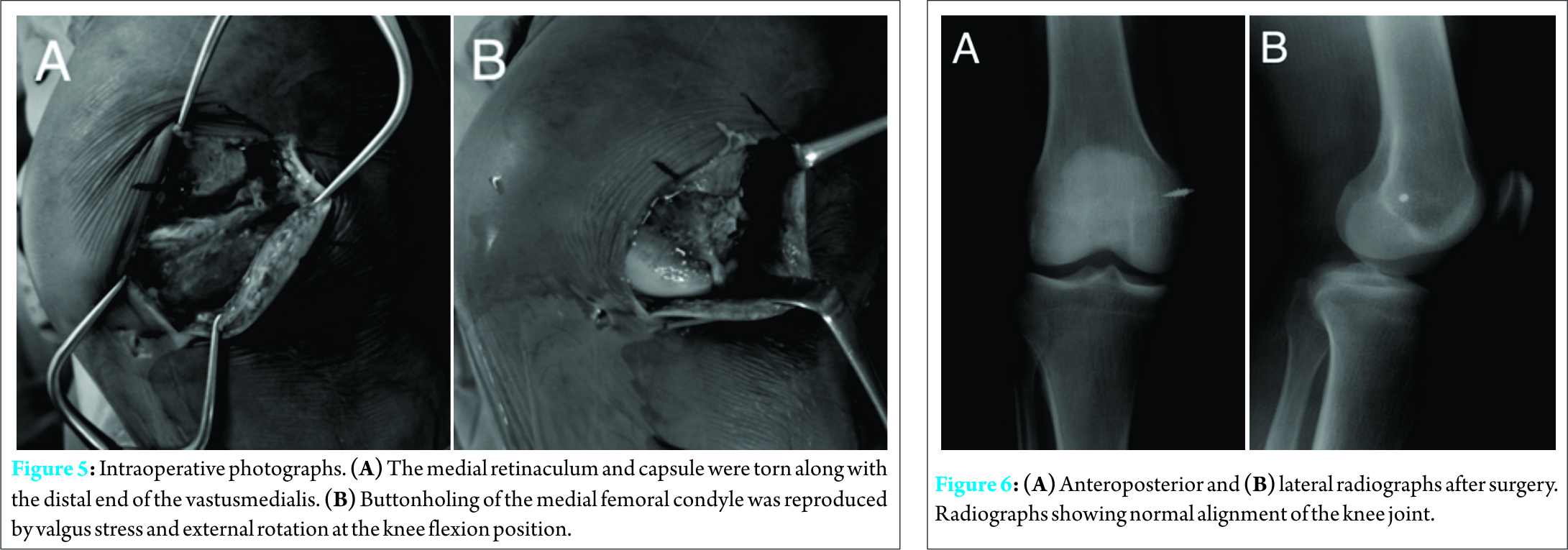
Dislocation of the knee is a serious but rare injury, representing less than 0.2% of all orthopedic injuries. Posterolateral rotary dislocation is much rarer and considered to be irreducible by closed reduction because of incarceration of soft tissues such as the medial capsule and retinaculum, vastusmedialis , and medial meniscus. The dimple sign is a physical finding caused by invagination of the skin and soft tissues into the medial joint space and is known to be characteristic of irreducible knee dislocation . To the best of our knowledge, there has been no reported case of posterolateral rotary knee dislocation successfully reduced by closed manipulation. Here, we present a case of posterolateral rotary knee dislocation with a clear dimple sign, which was reduced using a closed procedure. We believe that this is the first report of a successful closed reduction for posterolateral knee dislocation.
Case Report
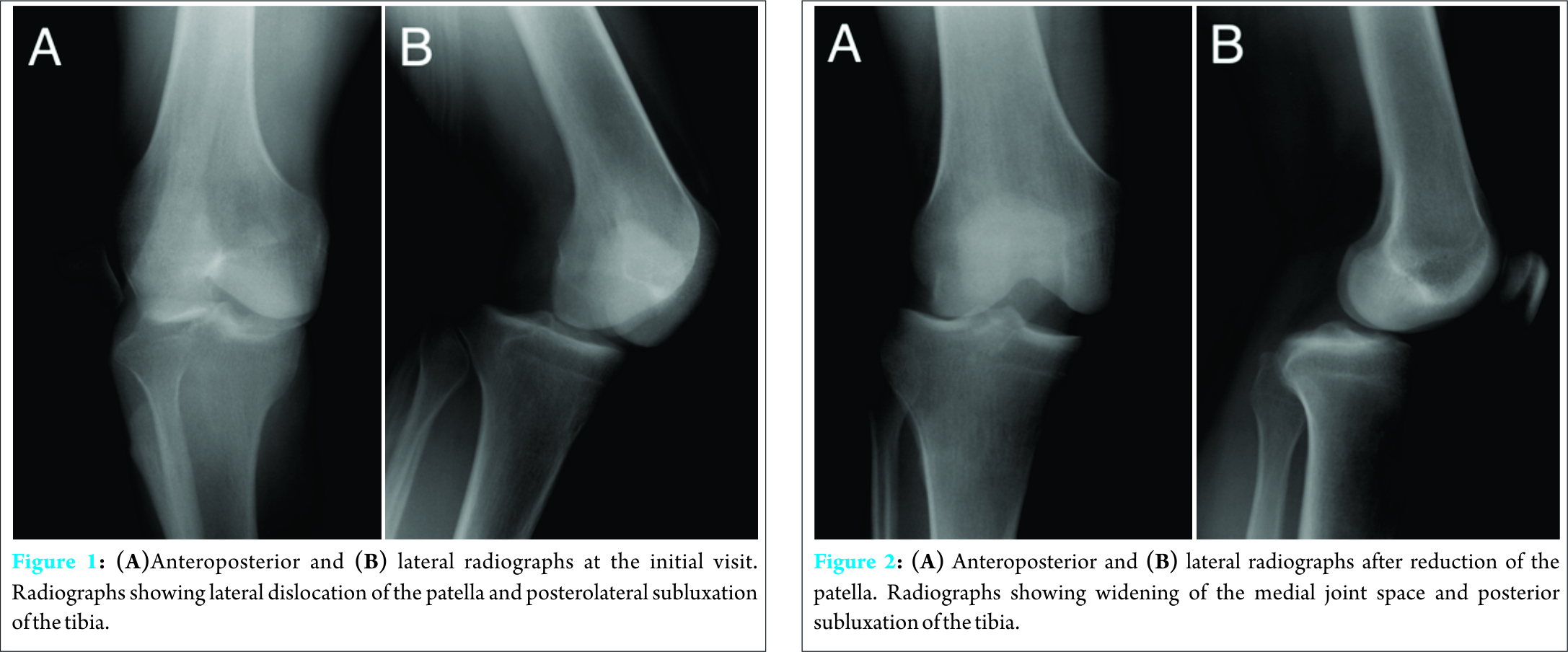
A 33-year-old man presented to the emergency department of our hospital with a twisting injury to his right knee and an open fracture of the left lower thigh that occurred while he was operating a rotary snow removal vehicle and his left lower thigh became trapped in the rotary blade. Physical examination revealed that the right knee joint was fixed at 30° flexion with a lateral shift of the patella. The contralateral open fracture was classified as grade 3A using the Gustilo–Anderson classifications ystem. No neurovascular injury to either leg was detected. Radiographic evaluation confirmed lateral dislocation of the patella and posterolateral subluxation of the knee (Fig. 1).
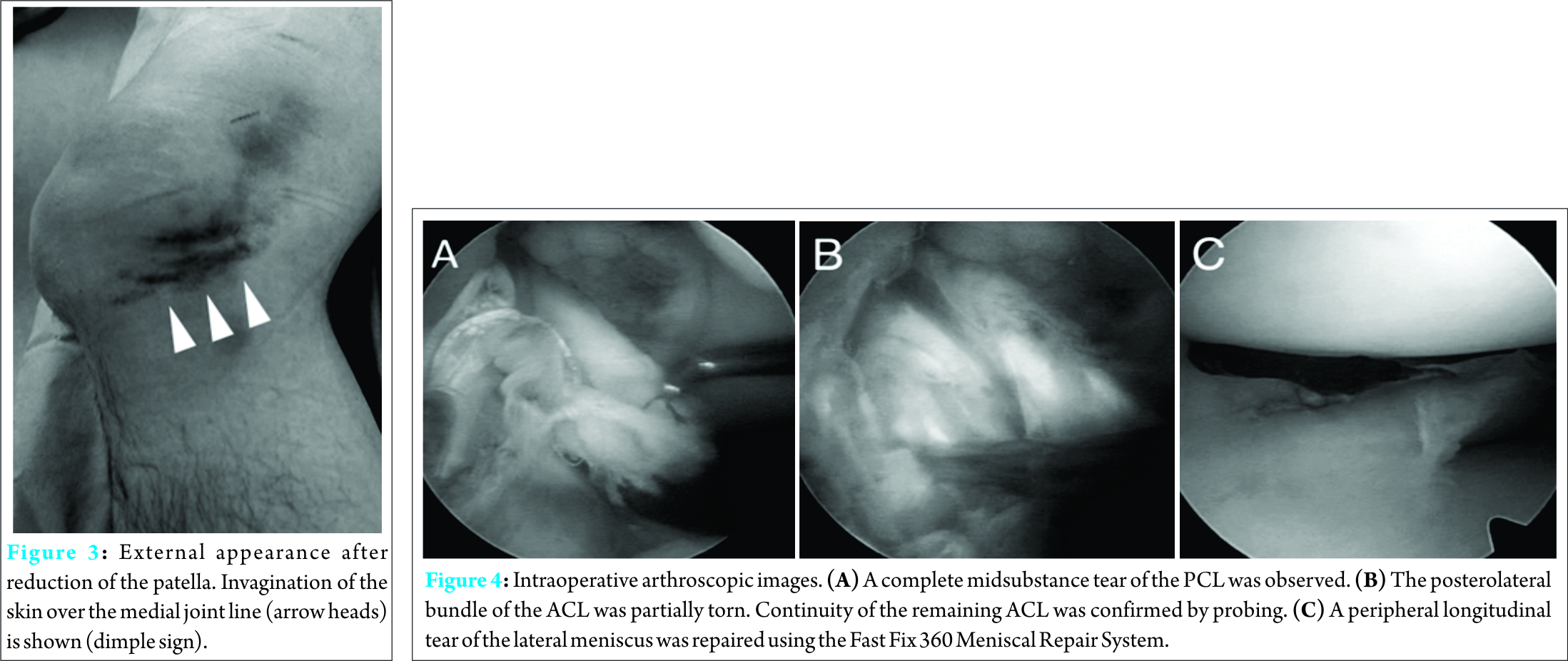
On the day of injury, the open fracture of the left lower thigh was stabilized with an external fixator after debridement and the dislocated patella of the right knee was reduced. However, closed reduction for knee joint dislocation could not be performed successfully. Plain radiographs after manipulation showed widening of the medial joint space and tibial posterolateral displacement (Fig. 2). The characteristic dimple sign was observed over the medial joint line (Fig. 3). On the medial aspect of the injured knee, the medial femoral condyle was palpable just beneath the skin. Two days after the injury, closed reduction was attempted under general anesthesia. The knee was flexed to 120° and valgus stress and internal rotation of the lower thigh were applied. The dislocated knee was reduced and the dimple sign disappeared. The posterolateral dislocation could be reproduced by external rotation at 100–120° flexion. After reduction, ligament instability tests were positive for valgus stress, with signs of posterior sagging in the posterior drawer test, and negative for the Lachman test, pivot shift test, extension recurvatum test, and dial test. A subsequent arthroscopic examination also revealed a complete midsubstance tear of the posterior cruciate ligament (PCL) (Fig. 4A) and a partial tear of the posterolateral bundle of the anterior cruciate ligament (ACL), which were not reconstructed (Fig. 4B). A peripheral longitudinal tear of the lateral meniscus was repaired using the Fast Fix 360 Meniscal Repair System (Smith & Nephew, Andover, MA, USA) (Fig. 4C).
Thereafter, a 7-cm medial longitudinal incision was made to repair the medial collateral ligament (MCL). The medial retinaculum and capsule were torn along with the distal end of the vastusmedialis. The MCL was completely detached from the femoral footprint. Button holing of the medial femoral condyle through the medial retinaculum and the capsule could be reproduced by valgus stress and external rotation in the knee flexion position (Fig. 5). In addition, the dislocation could be reduced by internal rotation of the lower thigh. The MCL was fixed to the femoral footprint using Suture Anchors (Mitek Products, Johnson & Johnson Company, Westwood, MA, USA). The medial retinaculum and the capsule were also repaired. Postoperative radiographs showed normal alignment (Fig. 6). Range of motion (ROM) exercises was started after 3 weeks of immobilization with a cylinder cast. Full weight bearing with a knee brace was allowed 4 weeks after surgery. One year postoperatively, no knee symptoms were observed and the ROM was 0–145°. There was no ligament instability except for the PCL at grade II.
Discussions
The most effective mechanism for posterolateral knee dislocation is considered valgus and rotational stress during knee flexion. However, the direction of rotational stress is reportedly internal rotation or external rotation . In the present case, the dislocation was reduced by internal rotation of the lower leg with knee flexion and reproduced by valgus and external rotation stress. In addition, lateral dislocation of the patella was observed at the initial visit. Therefore, valgus and external rotation stress during knee flexion may have been the cause of knee dislocation in our patient.
Reportedly, the MCL, ACL, and PCL are usually completely ruptured in posterolateral knee dislocation, whereas the posterolateral structures are usually left intact ; however, some recent studies have shown that a posterolateral injury may occur in combination with this type of dislocation. Therefore, combined ligament injuries should be carefully assessed by magnetic resonance imaging (MRI) or physical examination after reduction. In the present case, complete tearing of the MCL and PCL was observed, which is consistent with the findings of previous reports. However, the ACL in our case was only partially torn and exhibited no instability. Only one report by Jeevannavar et al. has described a partial ACL tear associated with posterolateral knee dislocation. The remaining ACLs may prevent complete button holing of the medial femoral condyle through the medial retinaculum and produce reducibility. Posterolateral knee dislocation is rarely accompanied by meniscal injuries . Bistolfil et al. and Samini et al. reported cases of this type of dislocation with medial and lateral meniscal injuries. In the present case, the patient had a peripheral longitudinal tear of the lateral meniscus. However, meniscal tears can sometimes be misdiagnosed by MRI. Therefore, arthroscopic examination may be useful in treating patients with posterolateral knee dislocation. The first-line therapeutic approach for posterolateral knee dislocation is conventionally considered immediate reduction by open surgery . However, as we demonstrated in the present case of posterolateral rotary dislocation, it may be possible to reduce this injury by closed manipulation. Closed manipulation by valgus stress and internal rotation could be tried as a first-line choice. Combined ligament injuries should be treated in consideration of patient age and activities of daily living. In the present case, MCL detachment was repaired using suture anchors and healed without any instability. The partial ACL tear did not cause any instability, where the PCL injury was left untreated and a posterior drawer test of grade II was identified at the final follow-up, although no clinical symptoms originated from this instability.
Conclusion
We experienced the case of posterolateral rotary knee dislocation which was reduced by closed manipulation. This is the first report of a successful closed reduction for posterolateral knee dislocation. In the present case, the dislocation was reduced by internal rotation of the lower leg with knee flexion and reproduced by valgus and external rotation stress. The mechanism of posterolateral knee dislocation was considered valgus and external rotation stress during knee flexion.
Clinical Message
Posterolateral rotary knee dislocation is a rare orthopedic injury that is considered to be irreducible by closed reduction because of soft tissue incarceration. However, with the result of the presented case, the closed manipulation by valgus stress and internal rotation could be tried as a first-line choice.
References
1. Robertson A., Nutton R W, and Keating J F. Dislocation of the knee. J Bone Joint Surg Br, 2006;88:706-711.
2. Cinar M., Derincek A, and Akpinar S. Irreducible dislocation of the knee joint: two-stage treatment. Acta Orthop Traumatol Turc 2011;45:280-283.
3. Harb A., Lincoln D, and Michaelson J. The MR dimple sign in irreducible posterolateral knee dislocations. Skeletal Radiol 2009;38:1111-1114.
4. Jeevannavar S.S. and Shettar C M. ‘Pucker sign’ an indicator of irreducible knee dislocation. BMJ Case Rep 2013;2013.
5. Said H.G. and Learmonth D J. Chronic irreducible posterolateral knee dislocation: two-stage surgical approach. Arthroscopy 2007;23:564 e561-564.
6. Bistolfi A., Massazza G, Rosso F, Ventura S, Cenna E, Drocco L, and Crova M. Non-reducible knee dislocation with interposition of the vastus medialis muscle. J Orthop Traumatol 2011;12:115-118.
7. Kilicoglu O., Akman S, Demirhan M, and Berkman M. Muscular buttonholing: An unusual cause of irreducible knee dislocation. Arthroscopy 2001; 17: E22.
8. Durakbasa M.O., Ulku K, and Ermis M N. Irreducible open posterolateral knee dislocation due to medial meniscus interposition. Acta Orthop Traumatol Turc, 2011;45:382-386.
9. Wand J.S. A physical sign denoting irreducibility of a dislocated knee. J Bone Joint Surg Br 1989;71:862.
10. Gustilo R.B. and Anderson J T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 1976;58:453-458.
11. Hughston, J.C. and Norwood L A Jr. The posterolateral drawer test and external rotational recurvatum test for posterolateral rotatory instability of the knee. Clin Orthop Relat Res 1980:82-87.
12. Jung Y.B., Lee Y S, Jung H J, and Nam C H. Evaluation of posterolateral rotatory knee instability using the dial test according to tibial positioning. Arthroscopy 2009;25:257-261.
13. Hill J.A. and Rana N A. Complications of posterolateral dislocation of the knee: case report and literature review. Clin Orthop Relat Res 1981:212-215.
14. Quinlan A.G. and Sharrard W J. Postero-lateral dislocation of the knee with capsular interposition. J Bone Joint Surg Br 1958;40(B):660-663.
15. Nystrom M., Samimi S, and Ha’Eri G B. Two cases of irreducible knee dislocation occurring simultaneously in two patients and a review of the literature. Clin Orthop Relat Res 1992:197-200.
16. Samimi S. and Shahriaree H. Arthroscopic view of an irreducible knee dislocation. Arthroscopy1993;9:322-326.
17. Urguden M., Bilbasar H, Ozenci A M, Akyildiz F F, and Gur S.. Irreducible posterolateral knee dislocation resulting from a low-energy trauma. Arthroscopy 2004;20(2):50-53.
18. Wilson T.C., Talwalkar J, and Johnson D L. Lateral patella dislocation associated with an irreducible posterolateral knee dislocation: literature review. Orthopedics 2005;28:459-461.
19. Nikolaou V.S., Chronopoulos E, Savvidou C, Plessas S, Giannoudis P, Efstathopoulos N, and Papachristou G. MRI efficacy in diagnosing internal lesions of the knee: a retrospective analysis. J Trauma Manag Outcomes 2008;2:4.
| How to Cite This Article: Tateda S, Takahashi A, Aizawa T, Umehara J. Closed Reduction of “Irreducible” Posterolateral Knee Dislocation – A Case Report. Journal of Orthopaedic Case Reports 2016 April – June;6(2): 20-23. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-412-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com