[box type=”bio”] What to Learn from this Article?[/box]
Tuberculosis is a great mimicker hence to diagnose it promptly, it must be considered as a possibility in long standing pain and swelling of midfoot.
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 37-39 | K A Saindane, Aashish B Ghodke, Sameer S Patil, Neha N Godghate, Sagar Kelkar. DOI: 10.13107/jocr.2250-0685.422
Authors: K A Saindane[1], Aashish B Ghodke[1], Sameer S Patil[1], Neha N Godghate[1], Sagar Kelkar[1]
[1] Department of Orthopaedics, ACPMMC, Sakhri Road, Dhule, Maharashtra. India.
Address of Correspondence
Dr. Aashish B. Ghodke,
Junior Resident, Department of Orthopaedics, ACPMMC, Sakhri Road, Dhule, Maharashtra. India. Pin: 424001.
E-mail: aashishghodke@gmail.com
Abstract
Introduction: Children show a higher predisposition to the development of extrapulmonary tuberculosis. Osteoarticular tuberculosis, especially in the foot is uncommon therefore it has remained a diagnostic enigma. The non-specific, often indolent, clinical presentation of foot (navicular) tuberculosis, whose low prevalence and low index of suspicion among clinicians may convert a purely osseous lesion into one involving a joint with more local destruction and functional disability. However, prompt diagnosis and treatment of this curable disease remains critical for initiation of proper management, prevention of joint deformity and permanent bone destruction.
Case Presentation: A 6-year-old female child with pain and swelling over the mid-foot was the subject of this study. Clinical, haematological, radiological examination and FNAC was done which revealed it to be of tuberculous pathology. Treatment consisted of anti-tubercular regimen for a period of 15 months. Within 4 months of starting anti tubercular therapy the patient was pain free and fully weight bearing on the affected foot.
Conclusion: To make a diagnosis of tuberculosis one must consider it as a possibility. Long standing pain and swelling of the midfoot should include TB in the differential diagnosis of destructive osteoarticular lesions. Since the radiological features are non-specific, so a high degree of suspicion is required to avoid permanent articular disability, to obtain a supple, painless and weight bearing foot.
Keywords: Naviculum, Osteoarticular tuberculosis, Bone and joint TB, Osteolytic cystic lesion.
Introduction
Tuberculosis has been known to affect mankind since the dawn of human civilization and still remains a major problem in the developing countries. Extrapulmonary tuberculosis accounts for up to one third of all cases and can be encountered in various organ systems like lymph nodes, serous cavities, genitourinary tract, skeletal. Children show a higher predisposition to the development of extrapulmonary tuberculosis. Osteoarticular involvement occurs in 1 to 3% of patients with extrapulmonary tuberculosis and spine represents 50% of these lesions. Extraspinal manifestations are the least common. The reported frequency of peripheral arthritis is 60%, osteomyelitis 38%, and of tenosynovitis and bursitis 2%. Intercurrent active pulmonary TB is only seen in about one half of the patients. According to sites of predilection, involvement of foot comes after spine, hip and knee sequentially [1]. In foot, the lesion involves calcaneum, talus, first metatarsal and navicular bones in order of decreasing frequency [2]. Involvement of bone and joints is secondary to pulmonary lesions. TB of bone usually occurs two years or longer after the initial pulmonary disease. Bone and joint TB results from haematogenous spread from pulmonary, visceral or lymph node foci. Most of those lesions heal with immunity but in some cases bone and joint involvement may be manifested. Osteoarticular tuberculosis, especially in the foot is uncommon therefore it has remained a diagnostic enigma. The non-specific, often indolent, clinical presentation of foot (navicular) tuberculosis, whose low prevalence and low index of suspicion among clinicians may convert a purely osseous lesion into one involving a joint with more local destruction and functional disability [3]. However, prompt diagnosis and treatment of this curable disease remain critical for initiation of proper management, prevention of joint deformity and permanent bone destruction. We hereby present a rare case of an isolated, cystic lesion of naviculum, where a high index of suspicion led us to the prompt diagnosis of tuberculosis and helped us save the patient from functional disability.
Case Presentation
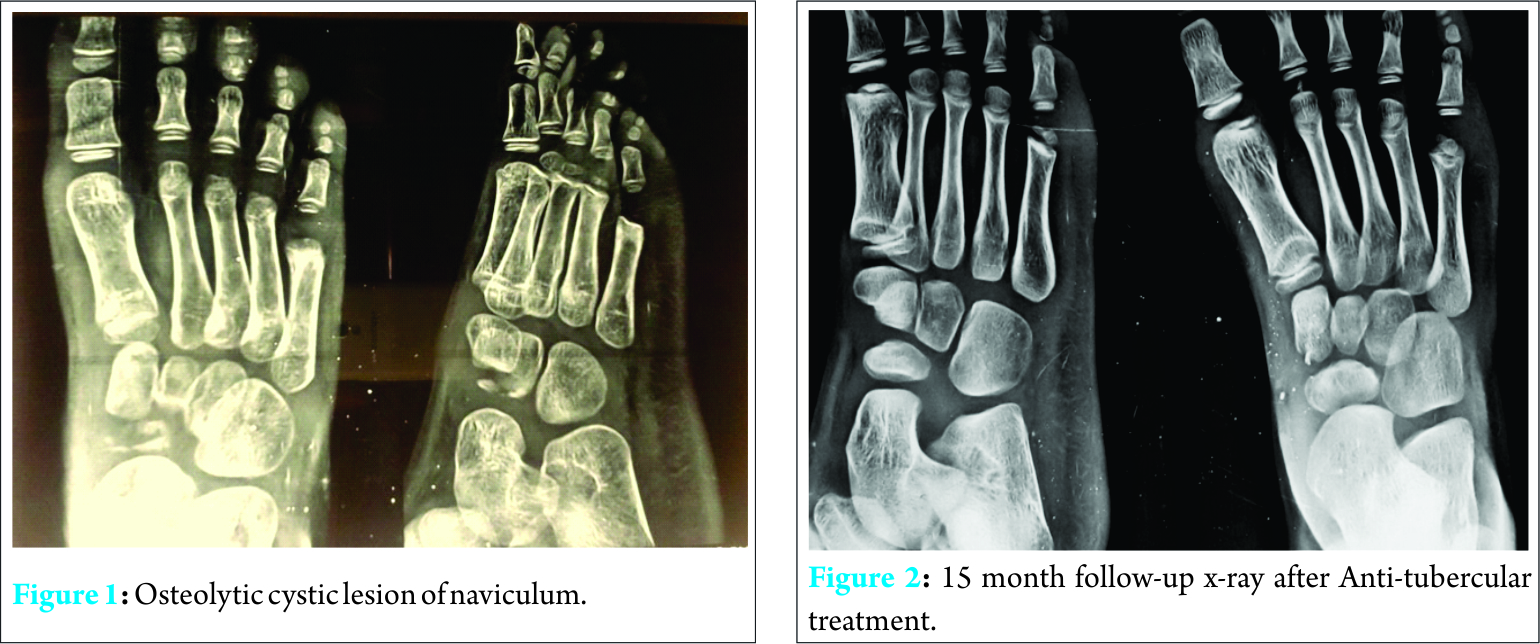
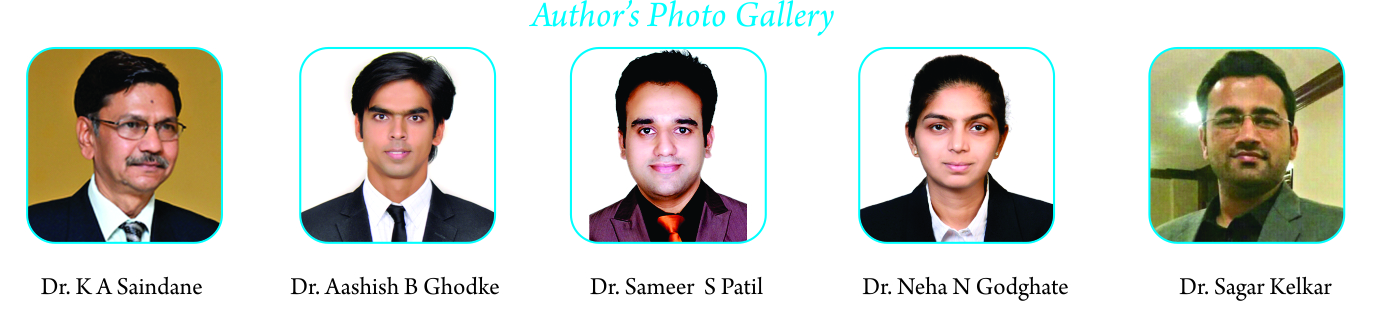
A 4-year-old female child was brought at our hospital with chief complaints of pain over the left mid-foot, pain was dull-aching in character and was present since 2 months. It was also associated with mild swelling. Weight bearing was painful since the last 15 days. There was no history of trauma, fever or weight loss. On examination, tenderness was present diffusely over the mid-foot, ankle movements were normal although limited by pain. Local temperature was slightly raised, no sinus or any induration felt. Ankle radiographs revealed an osteolytic, cystic lesion of the navicular bone (Fig. 1). Osteopenia was seen but the cortex were intact with no periosteal reaction evident. Heamatological investigations revealed a total leucocyte count of 11,200/cmm, lymphocytes 23%, ESR was 58 mm at the end of one hour, CRP was non-reactive. Lack of significant inflammatory changes and nonspecific findings on the X-rays led to a diagnostic dilemma. We then performed a FNAC of the lesion which revealed it to be of tuberculous pathology. Management consisted of isoniazid, rifampicin, pyrazinamide, and ethambutol for 2 months, followed by isoniazid and rifampicin for a total of 13 months. Immobilisation of the foot in plantigrade position with early active exercises of the involved parts was started as soon as the pain subsided after 4 to 6 weeks and within 4 months of starting anti tubercular therapy the patient was pain free with full weight bearing on the affected foot. At 15 month follow-up X-ray, the lesion was completely healed (Fig. 2).
Discussion
Bone and joint lesions are more frequent in childhood than in adults and occur up to 5% of all pediatric TB cases. In general, extra pulmonary TB is more common in children for the reason being, before adolescence the lesion in the foot, like any other skeletal lesion is usually the only gross lesion in the body with the exception of the lesion at the site of primary infection which is benign; but after adolescence, the disease changes its character, not in the foot, but in its distribution, because multiple lesions become the rule rather than the exception. This contrast between the incidence of associated tuberculosis lesions before and after puberty is due to the greater activity during childhood of the reticulo-endothelial and lymphatic tissues, groups of cells called the lympho-reticular apparatus, and on which the resistance of tuberculosis largely depends. After puberty, the lymphatic tissues wane and if immunity has not developed before then following primary infection, the resistance to primary infection is less. Tuberculosis of the foot and ankle occurs in less than 5% of the cases, most commonly involved bones are calcaneus, talus, first metatarsal, navicular, in decreasing order of frequency. Mid-tarsal joint is the most commonly affected joint. Pulmonary involvement is uncommon and seen in less than 50%of the cases. Tuberculosis is colloquially referred as the “The Great Mimicker” because no single pathognomonic finding can differentiate it from other pathologies [4]. As a result many cases of foot TB do not present in a classical manner. Treatment of BJTB which is a major public health problem is possible if it is recognized early and pre requisite for recognition is that a diagnostic possibility be considered [5]. Despite its importance, prompt diagnosis of TB in children is more difficult than in adults because it is complicated by the less dramatic signs and symptoms than that are seen in osteomyelitis of long bones [6]. Clinically, pain is the commonest symptom, as encountered in our case too. Local swelling and sinuses can be seen in some cases; in our case mild swelling was associated. Constitutional symptoms are not common; as were also absent in our case. Clinically, pyogenic osteomyelitis tends to be acutely painful, swollen, and hot with fever. Tuberculous osteomyelitis is relatively benign with mild pain and minimal pyrexia. Radiological assessment is often the first step in diagnostic workup of patients with osteoarticular TB and further investigations are determined by the findings of radiography. But both the radiologist and clinician should be aware of this diagnostic possibility. The most common radiologic finding is that of osteoporosis, which may be intense cancellous bone involvement and may present as a cystic lesion with or without sequestrum [7]. Other findings on plain radiograph include osteopenia, soft tissue swelling with minimal periosteal reaction, narrowing of joint space and subchondral erosions [8]. These non-specific radiologic features may be present in inflammatory arthritis, pyogenic osteomyelitis, Brodie’sabscess [9]. Mittal et al described some typical radiological features demonstrating 5 types: cystic, rheumatoid, subperiosteal, kissing, and spinaventosa. Of these, the cystic variety is relatively common as seen in our case. In the early stages and when the disease is limited to the bone, medical treatment leads to excellent healing and limited residual disabilities. Joint involvement occurs because of spread from a periarticular bony focus, and in the midfoot, the disease may spread to involve all the interconnected joints, leading to a stiff foot and residual deformities [10]. Next in line are the haematological investigations like total count, lymphocyte count, ESR, etc. Raised ESR has been observed, but it is neither specific nor reliable. Mantoux has limited role in adults in high prevalence area but can be useful in children under 5 years. USG allows a quick evaluation of soft tissue masses, abscesses, joint effusions, and the degree and extent of tendon and tendon sheath involvement. CT scan may be helpful for the detection of osseous or joint involvement, the presence or absence of periosteal reaction and soft tissue calcifications, sclerosis, and soft tissue abscesses. USG and CT scan are particularly useful for guiding fine needle aspiration or biopsy to provide material for histopathological examination, PCR-based assay for mycobacterial DNA, and culture. PCR technique can increase the sensitivity and help exclude non tuberculous mycobacterial infection of soft tissue [11]. However, it is not widely available. MRI is the preferred technique to demonstrate early bone marrow changes in tuberculous osteomyelitis and arthritis, joint effusion, and cartilage destruction. MRI of the foot shows periarticular osteoporosis, marginal erosion, and joint space narrowing (Phemister Triad). The radiological features of foot TB may be similar to rheumatoid arthritis, neuropathic joints, sarcoidosis and neoplasms so these entities should be excluded prior to institution of the therapy [12]. Radionuclide imaging for evaluating osteomyelitis includes three-phase bone scans, the use of leukocytes labeled with 99 -Tc or 111- In, 67-Ga citrate, and 18 F-FDG PET FDG tracer accumulates at sites of infection and inflammation and it can render false positive results in infection and inflammation differentiating malignancy. Because of the characteristics of tuberculosis disease, TB and malignancy can easily be confused [13]. Culture is considered to be the gold standard but since foot TB is a paucibacillary disease, so AFB culture is rarely positive. However, an ideal work up may not be possible under all circumstances. Wares et al. opined that attempts should be made to confirm by histopathologic examination and /or bacterial examination [14]. FNAC is a good alternative to biopsy in such isolated cystic lesions [10]; in our case we too did an FNAC and confirmed our findings on histopathological examination.
Isolated osteomyelitis of small bones like naviculum needs to be diagnosed promptly in the early stages of the disease, to prevent possible sequelae, such as septic arthritis of adjacent joints [10]. Multi anti-tuberculosis drugs is the cornerstone in the treatment of foot TB if an early and prompt diagnosis is done, although surgery is occasionally required. In our case, treatmentbconsisted of isoniazid, rifampicin, pyrazinamide,and streptomycin for 2 months followed by isoniazid and rifampicin for a total of 12 months. Prolonged treatment in osteoarticular tuberculosis is justified by the fact that it is a paucibacillary infection with many organisms being in a dormant state making them resistant to chemotherapy [15]. Immobilization with foot in the plantigrade position is essential in all cases to prevent pathological fractures and early active exercise of the involved parts/joints should be started as soon as clinical response to the treatment is observed. Clinical signs of healing are decreased pain and swelling of foot, disappearance of sinuses, improvement in gait, and increase in body weight. All the above clinical findings are evident as early as 5 weeks, but radiological signs of healing are evident after 5 months of treatment. Conservative treatment with antitubercular therapy regimen to all foot TB patients is must. Surgical intervention is reserved for patients with either a juxtaarticular focus threatening to involve a joint or an impending collapse of a midfoot bone with cystic destruction.
Conclusion
Long standing pain and swelling of the midfoot should include TB in the differential diagnosis of destructive osteoarticular lesions. Since the radiological features are non-specific, so a high degree of suspicion is required to avoid permanent articular disability, to obtain a supple, painless and weight bearing foot. Also, as children carry the greatest burden of developing disease and extra-pulmonary involvement, they reflect recent infection rather than secondary reactivation as in adults. Childhood TB may be considered as a marker of current transmission in the community and therefore the diagnosis of Tb in children is also a public health problem.
Clinical Message
To make a diagnosis of tuberculosis, one must consider it as a possibility.
References
1. Rao KM. Text Book of Tuberculosis. 2ndEdn. (Revised), Vikas Publishing House Pvt. Ltd. New Delhi 1981;408.
2. Tuli SM. In: Tuberculosis of the Skeletal system (Bones, Joints, Spine and Bursal Sheaths). 2ndEdn, Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, 1997;115
3. Dhillon MS, Tuli SM. Osteoarticular tuberculosis of the foot and ankle. Foot Ankle Int. 2001;22:679–86.
4. Lotfinia I, Vahedi P. Late-onset post-diskectomy tuberculosis at the same operated lumbar level: case report and review of literature. Eur Spine J 2010;19(2): 226-232.
5. Watts HG, Lifeso RM. Current Concepts Review: Tuberculosis of Bones and Joints. The Journal of Bone and Joint Surgery 1996;78(2):288-99.
6. A Anil, Dhami I, Kumar S, Nadkarni B. Calcaneal Tuberculosis : A Study of 39 Cases , J Bone Joint Surg Br 2002 vol. 84-B no. SUPP III.
7. Mittal R, Gupta V, Rastogi S. Tuberculosis of the foot. J Bone Joint Surg Br. 1999;81:997–1000.
8. Mkandawire NC, Kaunda E . Bone and joint TB at Queen Elizabeth Central Hospital 1986 to 2002 .Trop Doct 2005;35:14 – 6 .
9. Agarwal S, Caplivski D, Bottone EJ . Disseminated tuberculosis presenting with finger swelling in a patient with tuberculous osteomyelitis: a case report. Ann Clin Microbiol Antimicrob 2005;4 :18.
10. Dhillon MS, Nagi ON, Tuberculosis of the foot and ankle. Clin Orthop Relat Res. 2002;(398):107-13
11. Haider ALM. Bones and Joints Tuberculosis. Bahrain Medical Bulletin 2007;29:1-9.
12. Golden MP, Vikram HR. Extrapulmonary tuberculosis: An overview. Am Fam Physician 2005;72:1761–8.
13. Hardoff R, Efrat M, Gips S. Multifocal osteoarticular tuberculosis resembling skeletal metastatic disease. Evaluation with Tc-99m MDP and Ga-67 citrate. Clin Nucl Med 1995;20:279-281.
14. Wares F, Balasubramanian R., Mohan A , Sharma SK. Extrapulmonary Tuberculosis: Management & Control. In Agarwal and Chauhan, In Tuberculosis Control in India. Directorate General of Health Services/Ministry of Health and Family Welfare. Elsevier: India; 2005;95-114.
15. Dhillon MS, Aggarwal S, Prabhakar S, Bachhal V. Tuberculosis of the foot: An osteolytic variety. Indian J Orthop. 2012;46:206–11.
| How to Cite This Article: Saindane KA, Ghodke AB, Patil SS, Godghate NN, Kelkar S. Osteolytic Cystic Lesion of Naviculum: The Great Mimicker. Journal of Orthopaedic Case Reports 2016 April – June;6(2): 37-39. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-422-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com