[box type=”bio”] What to Learn from this Article?[/box]
Femoral neck fractures in below-knee amputees should be managed by total hip arthroplasty as a primary procedure before the onset of post-traumatic complications which are much more challenging to treat.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 63-66| Karim Masmoudi, Hédi Rbai, Ayman Ben Fradj, Jecem Saâdena, Anouar Boughattas. DOI: 10.13107/jocr.2250-0685.510
Authors: Karim Masmoudi[1], Hédi Rbai[1], Ayman Ben Fradj[1], Jecem Saâdena[1], Anouar Boughattas[1]
[1]Department of Orthopedics, Ibn Jazzar Kairouan Hospital, Les aghlabites Surgical Unit, Kairouan, Tunisia.
Address of Correspondence
Dr. Karim Masmoudi,
Department of Orthopedics, Ibn Jazzar Kairouan Hospital, Les aghlabites Surgical Unit,3100, Kairouan, Tunisia.
E-mail: mkfms@yahoo.fr
Abstract
Introduction: Femoral neck fracture on amputated limb is an uncommon lesion and challenging to manage.
Case Report: We report a case of a displaced neck fracture of the left femur in a 57-year-old female. She underwent at the age of the three a below-knee amputation of the ipsilateral limb for post traumatic ischemia. The fracture was managed by a total hip arthroplasty (THA), as a primary procedure. In this article we describe our experience of this unusual entity.
Conclusion: Total hip arthroplasty in patients with lower limb amputation is a challenging and uncommon intervention, especially when it’s a primary procedure. It may provide satisfactory outcome, and allows early rehabilitation.
Keywords: amputations, total hip arthroplasty, femoral neck, hip fracture.
Introduction
Hip fractures are a common source of morbidity and mortality worldwide. Nevertheless, the discovery and development of hip arthroplasty has improved its prognosis, with a high survival rate, and satisfactory functional results [1, 2, 3]. Although total hip replacement has been well described in the literature especially for healthy individuals, we found few pieces of information about the technical characteristics and results of this procedure in patients with lower extremity amputation [1, 2, 3, 4 5; 6]. Lower limb amputees can have many musculoskeletal problems such as osteoporosis, severe osteoarthritis, and muscle deficiency. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. Femoral neck fracture on amputated limb is an uncommon lesion and challenging to manage because of technical difficulties such as the patient setup, the surgical approach and the stump manipulation[2, 8, 11]. We report a rare case of femoral neck fracture in a patient with homolateral transtibial amputation, managed by a primary total hip arthroplasty.
Case Report
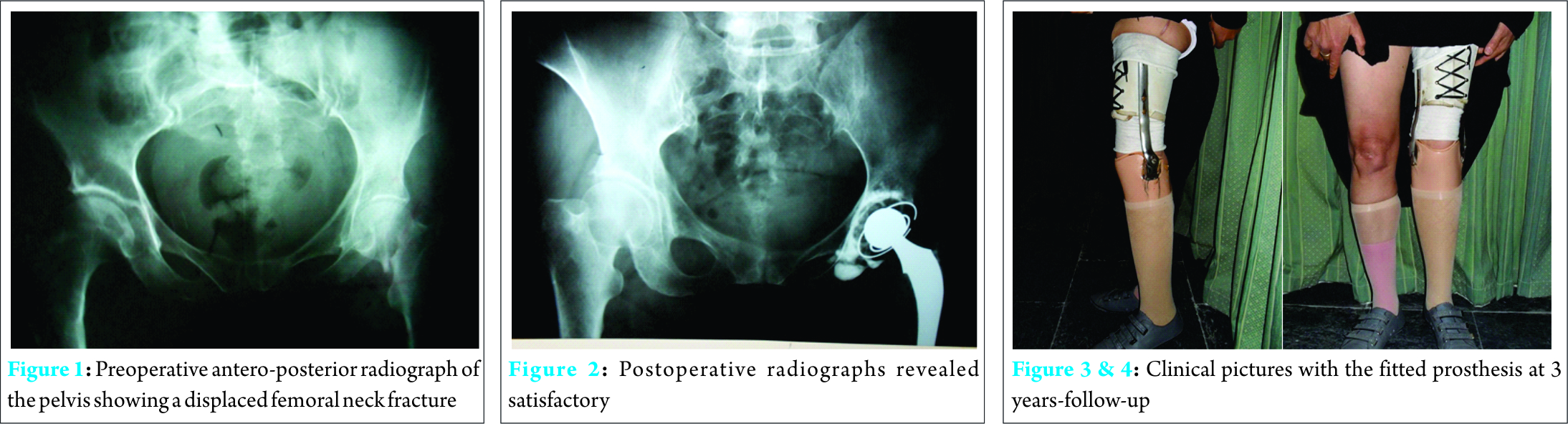
A 57-year-old female, who underwent at the age of 3 a below-knee amputation of the left lower limb for post traumatic ischemia, was taken to the emergency room for homolateral hip trauma. She tripped and fell from standing height striking the lateral aspect of her left hip on the ground. She was diagnosed with a grade IV femoral neck fracture, according to Garden’s classification (Fig. 1). Physical examination did not reveal any vascular or neurologic complications. No history of vascular or neurological diseases was found. Under general anesthesia, the patient was positioned on her right side with the spine parallel to the operating table. She underwent a cemented total hip arthroplasty with a trans-gluteal lateral approach: the arthroplasty included a modular metallic femoral implant with a 28mm head, and a polyethylene retentive cup (Fig. 2). Post-operatively, antibio prophylaxis for 72 hours as well as sub cutaneous anticoagulation was prescribed to prevent thrombo-embolic and infectious complications. The post-operative course was uneventful, and the patient was allowed weight bearing using his prosthesis, and progressive ambulation with two crutches on the third post-operative day. Physical therapy included isometric strengthening of the hip abductors and flexors, as well as active range-of-motion exercises. At the last follow-up (thirty-six months), no dislocation episode or infectious complication were noted. The operative wound was healed and dry. The patient had a satisfactory range of motion: her hip flexion was 90°, external and internal rotation was 30°, abduction was 40° and adduction was 20°. The patient was painless, able to walk with only one cane and to undertake all pre-morbid activity independently, using her usual prosthesis (Fig. 3 & 4)
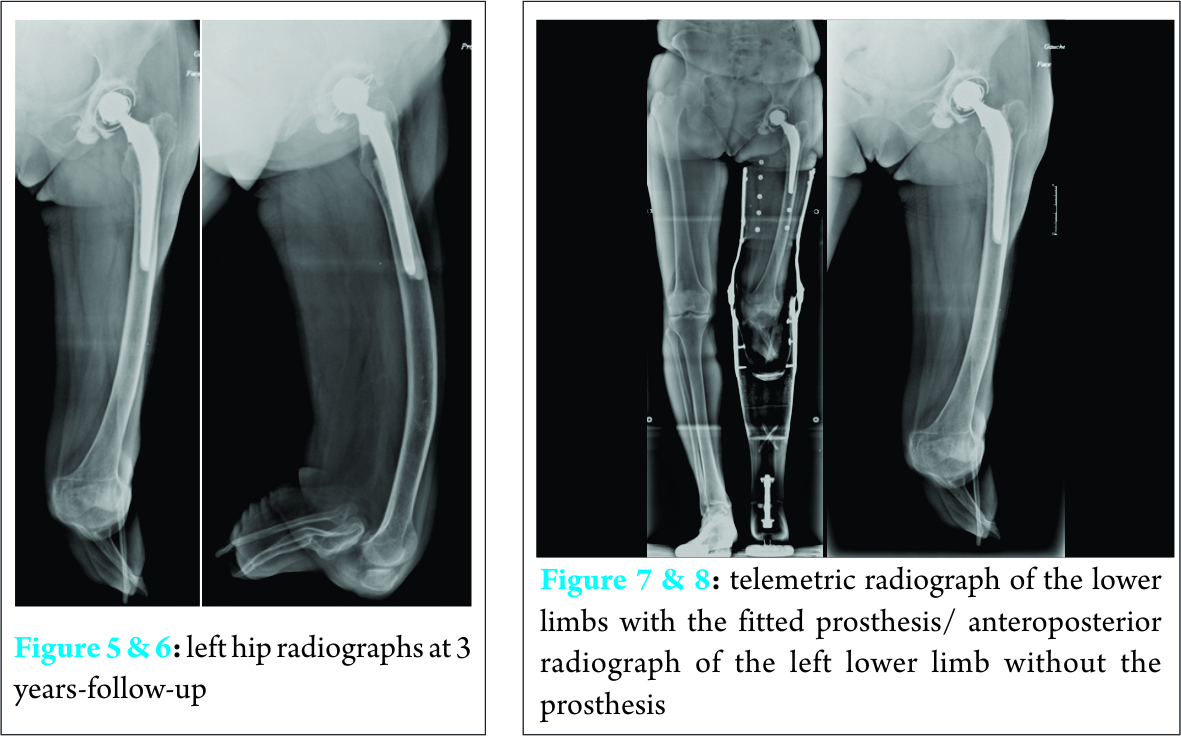
The functional outcome was good with a Harris Hips score at 87/100, and a Paustel-Merle-D’Aubigné at 16/18. The left hip radiographs did not reveal any signs of loosening or migration of the femoral and acetabular implants, neither signs of polyethylene wear (Fig. 5, 6 & 7).
Discussion
Total hip replacement is usually preconized to manage displaced femoral neck or sub-capital fracture of the femur. This injury can lead to major morbidity and mortality, especially for elderly patients. Discovery and constant evolution of hip arthroplasty has radically changed the prognosis of femoral neck fractures. [2, 11]
Residual lower limb fracture is a rare entity, with little information available in the previous literature [2, 8, 11]. Its review has shown that below knee amputation may induce osteo-articular as well as muscular modifications [1, 2, 3, 4, 5, 6, 7, 8, 9, 10] :
– Increase in the tibiofemoral and the patellofemoral osteo-arthritis on the un-amputated side
– Increase in osteoporosis on the amputated side
– Amyotrophy on both amputated and intact side: This amyotrophy results from the anatomical consequences of the surgical act and the loss of the muscle’s insertions or its re-implantation into a non-physiological site [9]
Some authors have established that amputee patients have a high risk of homolateral fracture because of the lever arm carried by the prosthesis, as well as the high rate of osteoporosis [2, 8, 10, 11]. This has been explained by the lack of mechanical stress on the amputated limb, while the unamputated one carries more loads [10].
Analysis of precedent literature showed that most surgeons preconize non –operative or conservative treatment for hip fracture in amputees patients, especially for the young ones, such as reduction and fixation or hip arthrodesis [11, 12, 13, 14]. Nevertheless, the risk of non-union of the fracture in such patients is higher. This can be explained by the biomechanic changes in the site of fracture: in patients with lower limb amputation, there is lateral shifting of the center of gravity that lead to increase the shearing forces on the fracture [11].
To our knowledge, there have been few publications reporting a THA in patients with below Knee amputation: Solomon and al [3], Salai.M and al [11].
Solomon [3] described a total hip replacement for severe osteoarthritis for a dysvascular below-knee amputee. Salai [11] reported a small series of five patients with below knee-amputation who underwent total hip arthroplasty for a subcapital femoral fracture. In only two cases, the THA was a primary procedure.
We believe that, up to date, this article is one of the rare case reports of a primary THA for a femoral neck fracture in a below-knee amputee, in the same side.
Total hip arthroplasty after lower extremity amputation can be very challenging, with serious technical issues such as surgical preparation, hip dislocation and reduction, component positioning and rehabilitation.
For above-knee amputees (AKA), the major problems are:
– the short lever arm with difficulties to handle the proximal femur during the hip dislocation and implants insertion. Some surgeons resorted to the use of a traction pin with a bone clamp or a bone holder in the sub-trochanteric area to have a satisfactory rotational and traction control on the stump [1, 2, 7, 8]
– the contracture of the hip flexors and abductors which may require soft tissue release [3, 4, 7]
– the placement of the femoral implant with an adequate length and in the appropriate depth according to the level of amputation [2]
– the dislocation of the hip may require, in some cases, a trochanteric or a femoral neck osteotomy [4, 7].
For patients with through-knee amputation, the knee and the calf which can be used as a fulcrum to manipulate the stump are missing. In this category of patients, several technical tips may be necessary such as a distal traction pin. This type of construct should be placed rather in the distal femoral shaft than the femoral condyles that are more osteopenic in through-knee amputees. [1]
Regarding below-knee amputees (BKA), THA would be less intricate, and the principal difficulty would be the correct positioning of the femoral component, with a risk of retroversion that was reported in several studies [1, 4, 7]. This malposition could be avoided by establishing a reference point prior to dislocation. [4]
Some of the technical issues are common for all three categories such as:
– prevention of the swelling of the limb after surgery, in order to allow an early return to ambulation with the usual prosthesis [7, 8]
– choice of implants that must be suitable for total weight bearing, which allows the patient to regain a satisfactory function [1, 4, 7]
– additional care should be brought to the skin of residual limb during closure of the operative wound to avoid troublesome scars, and conflicts with the prosthesis. [2, 4 8; 12]
– Osteoporosis caused by the amputation can lead to peroperative or post-operative peri prosthetic fractures [2, 4]
– Bone stock loss can cause an early loosening of the implant [4; 5; 7], especially in case of cementless arthroplasty.
– Muscular deficiency in the amputated limb increases the risk of hip dislocation [7].
In our case, we chose a total hip replacement because of the relative young age of the patient (fifty-seven years old), the high level of activity and autonomy using her usual prosthesis, as well as the high life expectancy (no medical history of cardio-vascular or respiratory diseases).
She underwent a total hip arthroplasty through a transgulteal approach, according to Hardinge. This approach was chosen because it offers a better exposure of the implants [2]. Several techniques have been perfomed by orthopaedic surgeons worldwide to prevent arthroplasty dislocation in patients with neuro-muscular diseases, such as constrained implants. [15]. The arthroplasty included a stainless steel, monoblock, cemented, femoral implant and a cemented, polyethylene retentive cup. The muscular deficiency due to amputation, which increases the risk of instability, has encouraged us to choose a constrained acetabular implant. We preferred a cemented arthroplasty rather than the cementless one, because of the lower risk of loosening on an osteoporotic field.
In this case, we didn’t have to use neither specific materials nor technical tips that were previously described, for multiple reasons:
-the procedure didn’t require a hip dislocation given that the patient had an acute femoral neck fracture
-the constructs that were suggested in the literature may lead to serious complications: infection, skin and soft tissue damage, per operative fractures [1; 2]
-this type of technical tricks (traction pin, bone holder), according to some authors, weren’t effective without excessive force which may pull out the osteoporotic bone of the stump [1; 8]
-the sufficient length of the stump and the low BMI (Body Mass index) of the patient allowed a satisfactory manipulation by grasping the limb from the knee (popliteal fossa)
-the normal anatomy of the hip enabled us to use the anatomic landmarks, such as the lesser trochanter, the femoral calcar, the linea aspera [4, 7] and the native acetabulum, to avoid malposition of the implants. Therefore, we used the physiological orientations with 10° of anteversion in the femoral component and 45° of abduction in the acetabular one.
Conclusion
The authors present this case because THA has rarely been reported as a primary treatment for acute femoral neck fracture in BKA while internal fixation is still relevant for this type of entity [13]. Most orthopedists resort to technical tips using material or specific constructs unlike our report in which we chose to use the normal anatomy of the patient’s hip as a guide in the implants positioning.
Through our limited experience combined with a brief literature review, we would suggest the following guidelines:
– Acute femoral neck fracture in BKA should be managed by THA as a primary treatment, before the onset of post-traumatic osteoarthritis of the hip and avascular necrosis of the femoral head. At these stages, the procedure would be much more intricate since a hip dislocation is required.
– Total hip arthroplasty provides a better rehabilitation with an early full-weight bearing and return to ambulation, unlike internal fixation, in the management of femoral neck fractures, even the non-displaced ones.
– The high risk of sustaining a fracture in osteoporotic residual stump should be included in the health education of amputee patient.
Clinical Message
THA can be performed for acute femoral neck fractures in patients with ipsilateral below-knee amputation, even as a primary procedure. This intervention reduces morbidity, allows early rehabilitation, and total weight bearing since the first week after surgery. Orthopedic surgeons should not wait for the failure of conservative treatment (non-union or avascular necrosis of the femoral head) to indicate a THA for below-knee amputees
References
1. Murat Pekmezci, MD, Ryan M. Nunley, MD, and Robert L. Barrack, MDd. Technique for Total Hip Arthroplasty in a Patient With Through-Knee Amputation. The Journal of Arthroplasty. 2010, Vol. Vol. 25 , No. 4. [PMID: 19447002]
2. Hassan Boussakri, Ihab Alassaf, Samir Hamoudi, Abdelhalim Elibrahimi, Hip Arthroplasty in a Patient with Transfemoral Amputation: A New Tip. Hindawi Publishing Corporation; Case Reports in Orthopedics; 2015, Vols. Volume 2015, Article ID 593747, 5 pages. [PMID: 25737790 ]
3. JENSON MAK, MICHAEL SOLOMON & STEVEN FAUX. Ipsilateral total hip arthroplasty in a dysvascular below-knee amputee for advanced hip osteoarthritis: A case report and review of the literature. Prosthetics and Orthotics International . 2008, Vols. June 2008; 32(2): 155 – 159. [PMID: 18569883 ]
4. Derek F. Amanatullah, MD, PhD, Robert T. Trousda le, MD and Rafa el J. Sierra, MD. Total Hip Arthroplasty After Lower Extremity Amputation. Orthopedics. 2015; . 2015, Vols. 38(5):e394-e400. [PMID: 25970366 ]
5. ScottM.M. Sommerville, James T. Patton, Jonathan C. Luscombe, and Robert J. Grimer. Contralateral Total Hip Arthroplasty After Hindquarter Amputation. Hindawi Publishing Corporation Sarcoma. 2006, Vols. Volume 2006, Article ID 28141, Pages 1–4. [PMID: 17496994]
6. Nejat1, Edward J. et al. TOTAL HIP ARTHROPLASTY AND REHABILITATION IN AMBULATORY LOWER EXTREMITY AMPUTEES—A CASE SERIES. The Iowa Orthopaedic Journal Total Hip Arthroplasty and Rehabilitation. 2005, Vol. Volume 25. [PMID: 16089069]
7. Sathappan S. Sathappan, MB ChB, James Wee, MBBS, Daniel Ginat, BS, Mathew Teicher, BS,Patrick Meere, MD, and Paul E. Di Cesare, MD. Total Hip Arthroplasty in Patients With Above-Knee Amputation: A Case Report. Am J Orthop. 2011, Vols. February 2011 40(2):E17-E19. [PMID: 21720599]
8. Leonid Kandel*1, Miguel Hernandez1, Ori Safran1, Isabella Schwartz2,Meir Liebergall1 and Yoav Mattan. Bipolar hip hemiarthroplasty in a patient with an above knee amputation: a case report. Journal of Orthopaedic Surgery and Research 2009. 2009, Vol. 4:30. [PMCID: PMC2734558; DOI: 10.1186/1749-799X-4-30]
9. N. Fraisse a, N. Martinet a, T.-J. Kpadonou a, J. Paysant a,*, A. Blum b, J.-M. Andre. Muscles of the below-knee amputees. Annales de readaptation et de medecine physique . Vols. 51 (2008) 218–227. [PMID: 18358554 ]
10. M. J. BURKE, * V. ROMAN, AND V. WRIGHT. Bone and joint changes in lower limb amputees. Annals of the Rheumatic Diseases . 1978, Vols. 37, 252-254. [PMID: 150823]
11. Moshe Salai, MD, Yehuda Amit, MD, Aharon Chechik, MD,Alexander Blankstein, MD, and Israel Dudkiewicz, MD. Total Hip Arthroplasty in Patients With Below-Knee Amputations. The Journal of Arthroplasty . 2000, Vol. Vol. 15 No. 8 2000. [PMID: 11112194]
12. J. H. Bowker, B. M. Rills, C. A. Ledbetter, G. A. Hunter, and P.Holliday. Fractures in Lower Limbs with Prior Amputation. The Journal of Bone and Joint Surgery. 1981, Vols. American Volume, vol. 63,, no. 6, pp. 915–920. [PMID: 7240332]
13. Anderson Freitas, MD, Diogo R.M. Souto, MD, Juliano F. da Silva, MD, Bruno R. Dantas, MD, and Ana Patricia de Paula, PhD. Treatment of an Acute Fracture of the Femoral Neck in a Young Female Adult with a Transfemoral Amputation. JBJS . 2015, Vol. Case Connect 2015;5:e58. [DOI : 10.2106/JBJS.CC.N.00119 ]
14. Denton JR, McClelland SJ. Stump fractures in lower extremity amputees. J Trauma. 1985 Nov;. 1985, 25(11):1074-8. [PMID: 4057296]
15. Philippe Hernigou MD, Paolo Filippini MD, Charles-Henri Flouzat-Lachaniette MD, Sobrinho Uirassu Batista MD, Alexandre Poignard MD. Constrained Liner in Neurologic or Cognitively Impaired Patients Undergoing Primary THA. Clin Orthop Relat Res (2010) . 2010, Vols. 468:3255–3262. [PMID: 20376709]
| How to Cite This Article: Karim Masmoudi, Hédi Rbai, Ayman Ben Fradj, Jecem Saâdena, Anouar Boughattas. Primary Total Hip Replacement for a Femoral Neck Fracture in a Below-Knee Amputee . Journal of Orthopaedic Case Reports 2016 July-Aug;6(3):63-66. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-510-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com