[box type=”bio”] What to Learn from this Article?[/box]
It is important to prevent bone mineral density loss in patients taking long-term anti-epileptic drugs.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 85-87 | Yoshikuni Mimata[1], Kotaro Sato[1], Ryunosuke Oikawa[1], Minoru Doita[1] DOI: 10.13107/jocr.2250-0685.526
Authors: Yoshikuni Mimata[1], Kotaro Sato[1], Ryunosuke Oikawa[1], Minoru Doita[1]
[1]Department of Orthopaedic Surgery, Iwate Medical University, Morioka, Japan.
Address of Correspondence
Dr. Yoshikuni Mimata,
Department of Orthopaedic Surgery, School of Medicine, Iwate Medical University, 19-1 Uchimaru, Morioka, 020-8505 Japan.
E-mail: mimata-iwt@umin.ac.jp
Abstract
Introduction: Introduction: The occurrence of non-traumatic vertebral compression fractures (VCFs) in a healthy young male is very rare. We present a rare case of non-traumatic thoracic VCFs in a young epileptic patient.
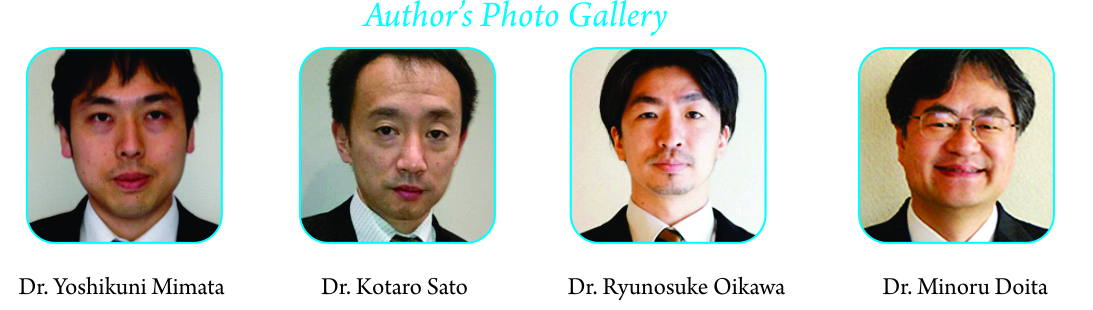
Case Report: A 19-year-old healthy male experienced severe back pain. There had been no significant traumatic event. A radiograph of the spine showed collapsed vertebra at Th6 and Th7 and magnetic resonance image of the spine showed intensity changes at Th6, Th7 and Th8. Bone mineral density (BMD) at the radius was low and urine N-terminal telopeptide (NTx) was very high. The patient was diagnosed with VCFs caused by low BMD. The patient had a medical history of epilepsy and had taken valproate for thirteen years. We instructed the patient to stop taking valproate and to begin taking bisphosphonate. As a result, urine NTx became normal.
Conclusion: It was previously reported that valproate reduced BMD in epileptic children and reduction in BMD increased with the duration of valproate therapy. We propose that regular BMD screening and measurement of bone metabolic markers should be conducted for all patients taking long-term antiepileptic drugs to prevent BMD loss and associated fractures.
Key word: non-traumatic, vertebral compression fractures, young, epilepsy, valproate,bone mineral density
Introduction
Vertebral compression fractures (VCFs) are the most common fractures in patients who have reduced bone mineral density (BMD). VCFs in patients with osteoporosis can be caused by simple daily activities. In contrast, people with healthy spines most commonly suffer VCFs through severe trauma, such as a car accident, a fall. The occurrence of non-traumatic thoracic vertebral compression fractures in a healthy young male is very rare. We present a rare case of non-traumatic thoracic vertebral compression fractures in a young epileptic patient.
Case Presentation
A 19-year-old healthy male, college student, experienced back pain in the morning and was unable to leave his bed; he was later shifted to our hospital. There was no significant traumatic event on the previous day; however, he had a medical history of epilepsy (normal daily activity and normal diet), and had used sodium valproate (VPA) for thirteen years. His last seizure took place 10 years ago. Fatal cardiovascular diseases, such as acute myocardial infarction or acute aortic dissection, were suspected due to the sudden onset, and a blood test, an electrocardiogram, an echocardiogram, and an enhanced computed tomography (CT) were performed. Following detailed examinations, these fatal cardiovascular diseases were rejected. In contrast, a radiograph of the spine revealed collapsed vertebra at Th6 and Th7 (Fig. 1). Magnetic resonance image (MRI) of the spine showed low intensity in a T1-weighted image and high intensity in a short-T1 inversion recovery image at Th6, Th7 and Th8 (Fig. 2). 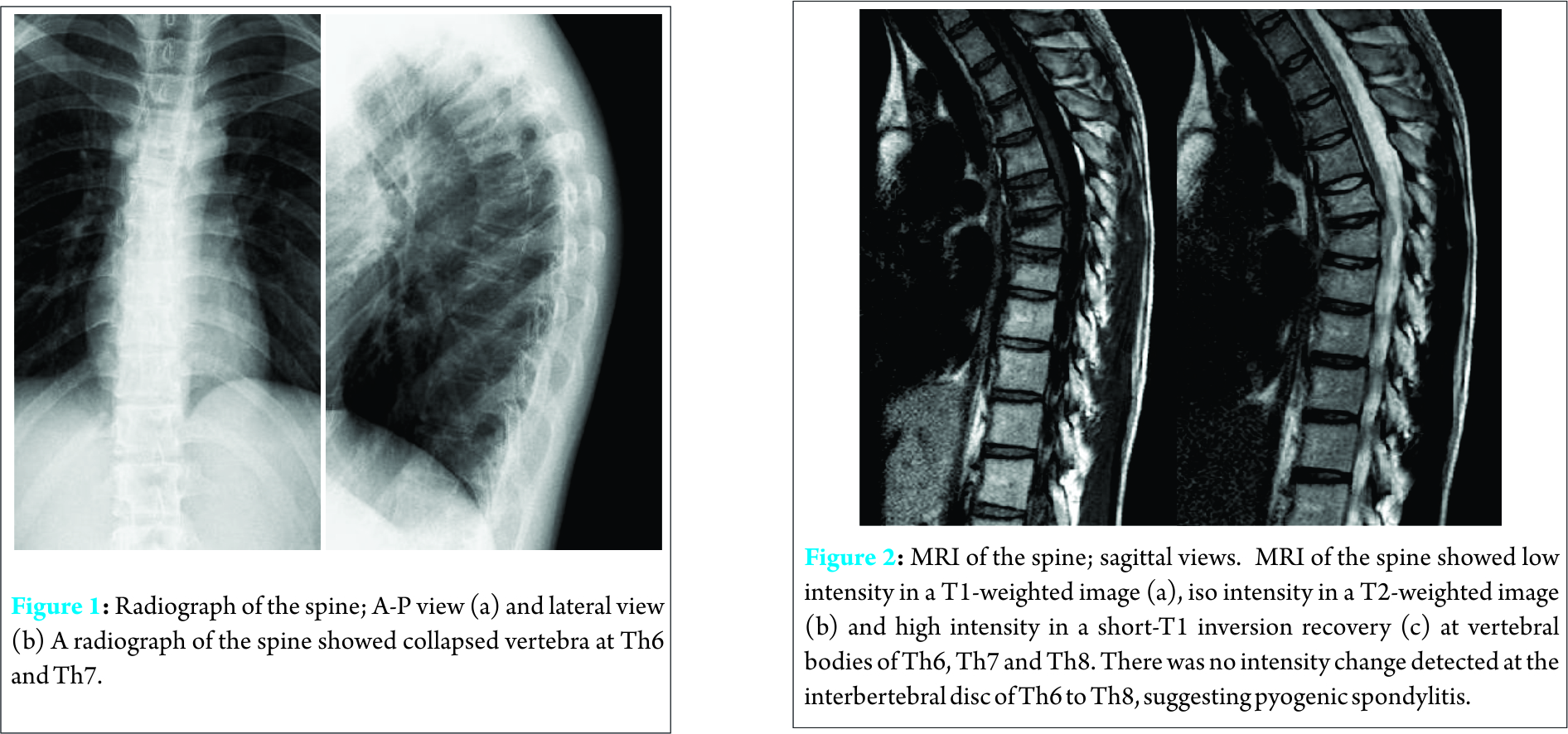
Discussion
Epilepsy is a group of long-term neurological disorders characterized by epileptic seizures and is associated with several comorbidities; such as developmental disorder, movement disorder, mental retardation, and bone health. There is increasing evidence suggesting that epilepsy and its treatment can affect bone mineralization and calcium metabolism. Many studies have demonstrated a significant reduction of BMD and an increased risk of fractures in patients taking antiepileptic drugs (AEDs) [1-4]. Sheth reported the effect of carbamazepine and VPA on BMD in epileptic children [1]. They concluded that VPA significantly reduces BMD in epileptic children and reduction in BMD increased with the duration of VPA therapy [1]. Kafali [2] and Ecevit [3] also reported VPA reduced BMD in children. Vestergaard assessed the fracture risk associated with antiepileptic drug therapy and suggested that VPA was significantly associated with the risk of fracture [4]. We consider loss of BMD is commonly asymptomatic; therefore, patients aren’t usually aware of the condition until they suffer fractures. In addition, we regret many clinicians don’t have knowledge that AEDs can reduce BMD in children. The mechanisms of the adverse effects of AEDs on calcium metabolism remain elusive in spite of many reports. Abnormal calcium metabolism was considered to result from the cytochrome P450 enzyme-inducing properties of some AEDs, such as carbamazepine, phenytoin, and the resultant reduction in vitamin D levels. However, the effect of VPA cannot be readily explained by vitamin D metabolism because VPA is not an inducer. In an experimental study, oral administration of VPA to epileptic rats for 6 months resulted in a significant increase of bone specific alkaline phosphatase (BAP), osteocalcin, NTx, etc compared with the control group [5]. The authors postulated that the increase of these bone formation markers was caused by increased osteoblast activity in order to compensate for increased osteoclastic activity [5]. VPA may facilitate bone turn over, resulting in a balance between bone formation and resorption [5]. To prevent BMD loss, vitamin D3, and/or bisphosphonate was recommended for high-risk patients who receive long-term treatment with AEDs. Takahashi reported the co-administration of activated vitamin D3 (alfacalcidol) or bisphosphonate (alendronate) with VPA did not induce osteopenia in growing rats [6]. According to this result, we administered bisphosphonate to our patient. As a result, the bone absorption marker drastically decreased and BMD was slightly increased (0.656 g/cm2). In summary, we presented a rare case of vertebral compression fractures that occurred in a young epileptic patient who had been on VPA for thirteen years. We propose that regular BMD screening and measurement of bone metabolic markers should be conducted for all patients taking long-term AEDs to prevent BMD loss and associated fractures.
Conclusion
We presented a rare case of non-traumatic thoracic vertebral compression fractures occurred in a young epileptic patient. BMD was low and urine NTx was very high. Regular BMD screening and measurement of bone metabolic markers should be conducted for all patients taking long-term antiepileptic drugs to prevent BMD loss.
Clinical Message
One of the causes of vertebral compression fractures was low bone density. Antiepileptic drug valproate can reduce BMD in epileptic patients. However, in many cases, BMD screening and appropriate treatments for BMD loss are not performed. Bisphosphonates of vitamin D3 therapy is effective to prevent loss of BMD. Regular BMD screening and measurement of bone metabolic markers should be conducted for all patients taking long-term antiepileptic drugs.
References
1. Sheth RD, Wesolowski CA, Jacob JC, Penny S, Hobbs GR, Riggs JE, Bodensteiner JB. Effect of carbamazepine and valproate on bone mineral density. J Pediatr 1995; 12: 256-62.
2. Kafali G, Erselcan T, Tanzer F. Effect of antiepileptic drugs on bone mineral density in children between age 6 and 12 years. Clin Pediatr 1999;38:93-8.
3. Ecevit C, Aydogan A, Kavakli T, Altinoz S. Effect of carbamazepine and valproate on bone mineral density. Pediatr Neurol 2004;31:279-82.
4. Vestergaad P, Rejnmark L, Mosekilde L. Fracture risk associated with use of different antiepileptic drugs. Epilepsia 2004;45:1330-7.
5. Elwakkad AS, El Elshamy KA, Sibaii H. Fish liver oil and propolis as protective natural products against the effect of the anti-epileptic drug valproate on immunological markers of bone formation in rats. Epilepsy 2008; 80: 47-56.
6. Takahashi A and Onodera K. Valproic acid induced osteopenia and its prevention with alfacalcidol and alendronate. J Hard Tissue Biology 2005;14: 275-6.
| How to Cite This Article: Mimata Y, Sato K, Oikawa R, Doita M. Non-traumatic Thoracic Vertebral Compression Fractures Occurred in a Young Epileptic Patient: A Case Report. Journal of Orthopaedic Case Reports 2016 July-Aug: 6(3):85-87. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-526-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com