[box type=”bio”] What to Learn from this Article?[/box]
To encourage clinicians to question a radiograph that does not fit with the clinical findings of a neck of femur fracture and consider further imaging to obtain a more definitive picture.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 14-16 | Saleem Ashley Farooqui, David Alexander Ranford, Al-Ashraf Khoriati. DOI: 10.13107/jocr.2250-0685.608
Authors: Saleem Ashley Farooqui[1], David Alexander Ranford[2], Al-Ashraf Khoriati[1]
[1]Department of Orthopaedics, Kingston Hospital, London, England,
[2]Department of Orthopaedics, King’s College London, London, England.
Address of Correspondence
Dr. Al-Ashraf Khoriati,
68 Daybook Road, SW19 3DH London, England.
E-mail: alkhoriati@doctors.org.uk
Abstract
Introduction: On rare occasions, hip fractures can be missed. Approximately 75,000 neck of femur fractures occur in the United Kingdom per annum. Up to 10% of hip fractures are occult on plain radiograph. This case demonstrates a usual presentation of an “incidental” neck of femur fracture, which had been missed 1 year prior.
Case Presentation: A 91-year-old gentleman presented with incidental finding of left neck of femur fracture on a routine radiograph. A quick review of the patient notes revealed a fall, with a lengthy hospital admission, approximately 1 year previously. Despite his initial inability to weight-bear and protracted slow progress with physiotherapy no further imaging of the hip was obtained beyond an initial, negative pelvic radiograph.
Conclusion: Doctors must be bold in questioning a radiograph that does not fit with the clinical picture. Clinical suspicion of neck of femur fracture in the face of a negative radiograph necessitates further imaging to obtain a definitive answer.
Keywords: Fracture, incidental, neck of femur, radiograph.
Introduction
Many doctors regard diagnosing a hip fracture as a simple task. The more experienced doctor knows that some cases are not clear-cut, as between 2% and 10% are occult on conventional radiography [1-4]. In cases, where there is clinical suspicion of a neck of femur fracture, but imaging has been negative or equivocal, further imaging (e.g. magnetic resonance imaging/computed tomography) is required [5]. Hip fractures, like everything else, can be missed and this can have serious implications for patients. A delay of over 48 h from admission to surgery doubles the risk of death within 1 year postoperatively [6].
Case Report
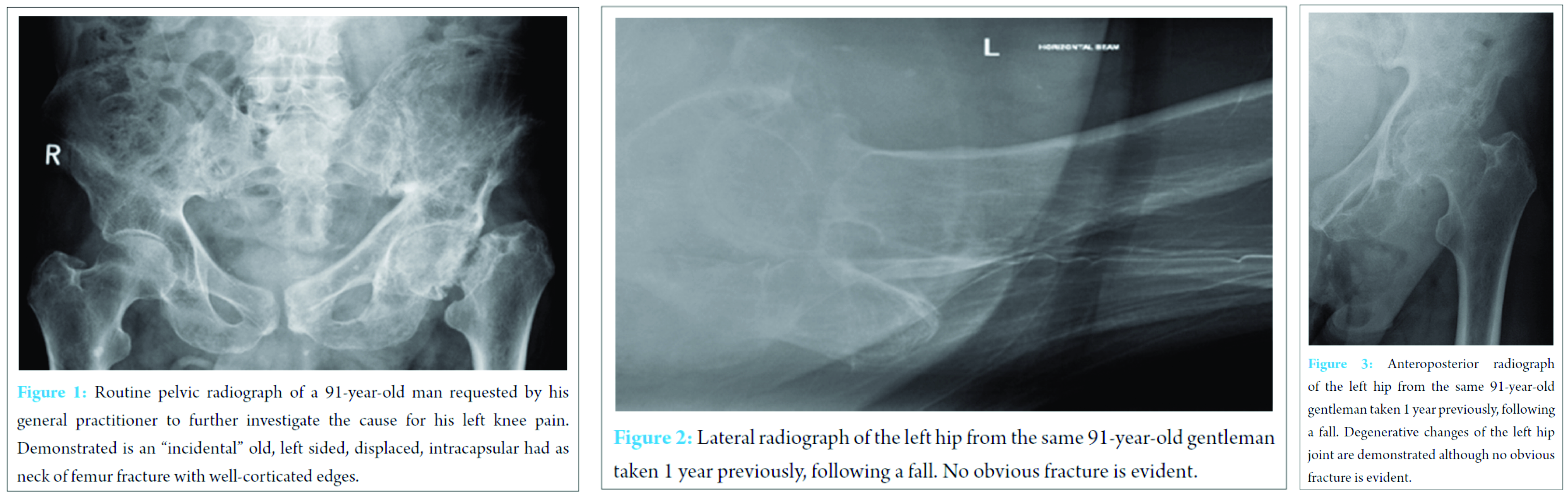
Following a routine radiograph performed by his general practitioner a 91-year-old gentleman was referred to accident and emergency with an incidental finding of fractured left neck of femur (Fig. 1). His general practitioner had requested a pelvic radiograph to further investigate the cause of this gentleman’s left knee pain. Despite no falls within the previous year, he had been experiencing worsening left knee pain for several months. The radiograph demonstrated the well-corticated edges of an old fracture, and the patient was able to mobilize using his frame. A decision was taken not to operate, and the patient was discharged.
Review of past incidents to find a cause for this neck of femur fracture quickly illuminated a possible event. Approximately 1 year prior, the patient had been admitted to hospital following a mechanical fall at home, after which he was unable to weight-bear. Clinical examination had demonstrated none of the salient features of a neck of femur fracture or had initial radiographs of the pelvis exposed a fracture (Fig. 2); only degenerative changes consistent with osteoarthritis (Fig. 3). Radiographs of the knee demonstrated no abnormality, yet the gentleman was unable to walk and was admitted.
Three weeks later, the patient continued to make poor progress with physiotherapy. No further imaging of the patient’s pelvis was obtained. Magnetic resonance imaging of his left knee was requested to exclude the possibility of soft tissue injury, which demonstrated a tear of the medial meniscus. Felt to be the cause of his delayed progress, further physiotherapy was encouraged and eventually this gentleman managed to mobilize independently with a frame. He was discharged home from hospital via rehabilitation facility.
Discussion
Hip fractures are often simple to diagnose clinically and radiologically, with initial imaging sensitivity estimated as 90-98% [1-4]. Approximately 75,000 femoral necks are fractured in the UK per annum [7] and this is projected to rise further [8]. If initial radiographs alone are used to exclude a neck of femur fracture then this poses the alarming possibility that up to 7,500 (of the known) neck of femur fractures could have been missed. Delays in diagnosis increase the risk of avascular necrosis, arthroplasty, nonunion, thromboembolic events, and mortality [9, 10].
This case and figures above demonstrates the need for clinicians to have a high index of suspicion when evaluating elderly patients following a fall. If there is clinical suspicion of a neck of femur fracture, then a negative radiograph is not enough and further imaging is required; magnetic resonance imaging – or computed tomography, if unavailable or contraindicated [5].
Conclusion
The sheer prevalence of neck of femur fractures, combined with the knowledge that up to 10% are occult on radiograph [1, 2, 3, 4] necessitates clinicians to have a high index of suspicion of occult neck of femur fractures in elderly patients following a fall. Although occult fractures are well documented in the literature, Hilton’s law, as well as referred pain from the joint above or below, are reasons for the threshold for further imaging modalities to be lowered. The aim of this case report is to raise awareness, to encourage doctors to be bold in questioning a radiograph that does not fit with the clinical picture and to increase requests for further imaging to obtain a definitive answer; the numbers and guidelines [7] are on your side.?
Clinical Message
To encourage clinicians to question a radiograph that does not fit with the clinical findings of a neck of femur fracture and consider further imaging to obtain a more definitive picture.
References
1. Kim KC, Ha YC, Kim TY, Choi JA, Koo KH. Initially missed occult fractures of the proximal femur in elderly patients: implications for need of operation and their morbidity. Arch Orthop Trauma Surg 2010;130(7):915-920.
2. Rubin G, Malka I, Rozen N. Should we operate on occult hip fractures? Isr Med Assoc J 2010;12(5):316-317.
3. Beloosesky Y, Hershkovitz A, Guz A, Golan H, Salai M, Weiss A. Clinical characteristics and long-term mortality of occult hip fracture elderly patients. Injury 2010;41(4):343-347.
4. Lubovsky O, Liebergall M, Mattan Y, Weil Y, Mosheiff R. Early diagnosis of occult hip fractures MRI versus CT scan. Injury 2005;36(6):788-792.
5. Gill SK, Smith J, Fox R, Chesser TJ. Investigation of occult hip fractures: the use of CT and MRI. ScientificWorldJournal 2013;2013:830319.
6. Chana R, Noorani A, Ashwood N, Chatterji U, Healy J, Baird P. The role of MRI in the diagnosis of proximal femoral fractures in the elderly. Injury 2006;37(2):185-189.
7. NICE 2011. CG124 – Hip Fracture: The Management of Hip Fracture in Adults. Available from: http://www.nice.org.uk/guidance/cg124/. [Last accessed on 2015 Jan 07].
8. Verbeeten KM, Hermann KL, Hasselqvist M, Lausten GS, Joergensen P, Jensen CM, et al. The advantages of MRI in the detection of occult hip fractures. Eur Radiol 2005;15(1):165-169.
9. Cabarrus MC, Ambekar A, Lu Y, Link TM. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol 2008;191(4):995-1001.
10. Marottoli RA, Berkman LF, Leo-Summers L, Cooney LM Jr. Predictors of mortality and institutionalization after hip fracture: the New Haven EPESE cohort. Established Populations for Epidemiologic Studies of the Elderly. Am J Public Health 1994;84(11):1807-1812.
| How to Cite This Article: Farooqui SA, Ranford DA, Khoriati A. A Case Report of an “Incidental” Neck of Femur Fracture. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):14-16. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-608-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com