box type=”bio”] What to Learn from this Article?[/box]
Fixation devices that hold the mandibular fractures in three dimensions counteracting the shear, torsional and bending forces eliminate the use of intermaxillary fixation which is advantageous to the patient.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 35-40| Shreyas H Gupte, Shruti Chaddva, Yash Jethwani, Aditi Mohandas, Digvijay P Kumavat, Nirali Jhaveri DOI: 10.13107/jocr.2250-0685.620
Authors: Shreyas H Gupte[1], Shruti Chaddva[1], Yash Jethwani[1], Aditi Mohandas[1], Digvijay P Kumavat[1], Nirali Jhaveri[1]
[1]Department of Oral and Maxillofacial Surgery. YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India.
Address of Correspondence
Dr. Shreyas H Gupte,
Department of Oral and Maxillofacial Surgery, YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India.
E-mail: gshreyas@rediffmail.com
Abstract
Introduction: The purpose of the study was to analyze whether adequate fracture fixation can be achieved by three-dimensional (3D) stainless steel mini-plates its ease of placement, whether the patient can resume function early and to find out the need to do intermaxillary fixation.
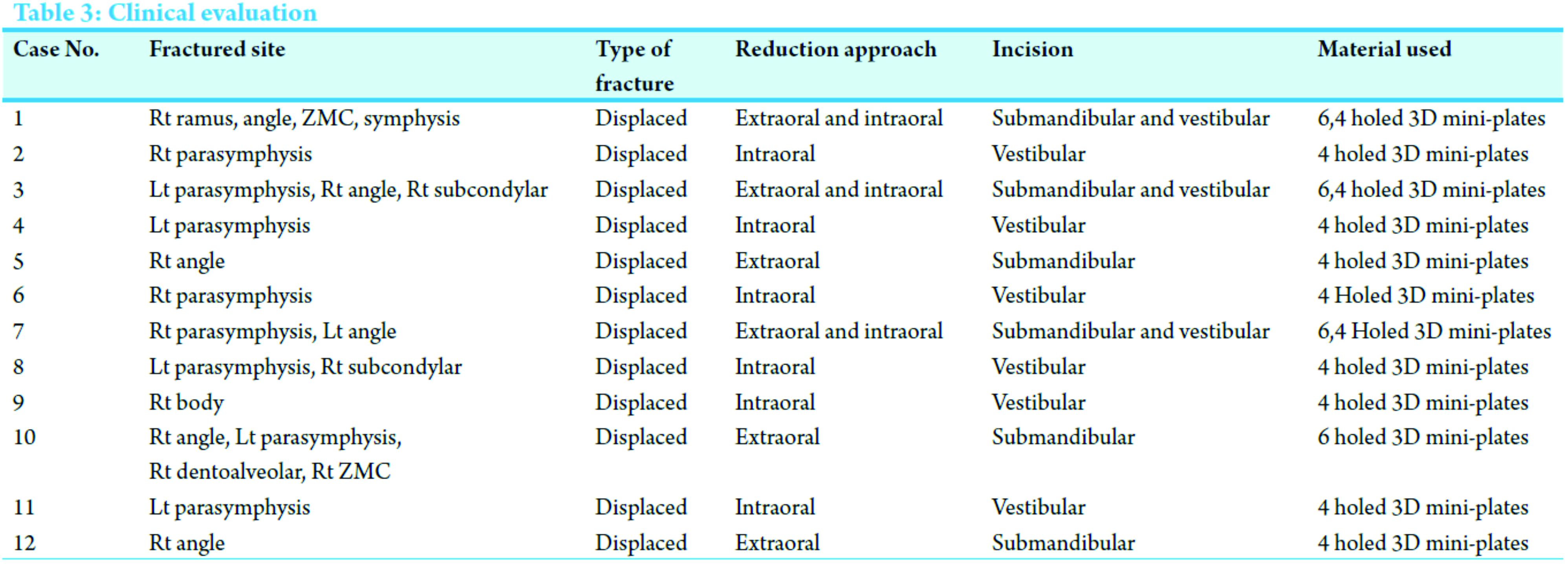
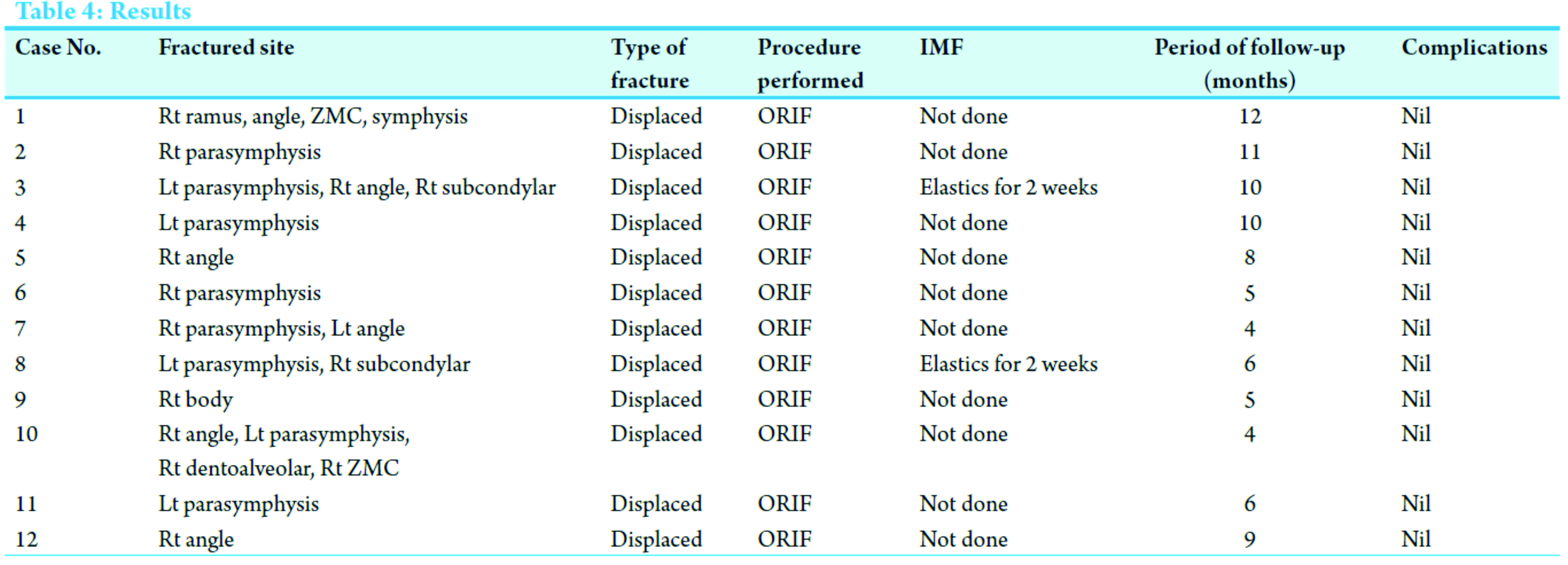
Materials and method: In the prospective study, we treated 12 patients and 17 fractured sites using 3D mini-plates. Once fracture reduction was achieved temporary intermaxillary fixation (IMF) was done occlusion was achieved and the fractured segments were fixed using 3D plates either 4-holed or 6-holed of 2.5 mm thickness and 6-8 mm length screws. IMF was removed subsequently.
Conclusion:In none of the cases non-union or malocclusion was noted. Similarly except for 2 cases which had associated subcondylar fractures IMF was not done postoperatively. The patients were able to achieve function immediately with a reasonable level of success. The interincisal opening ranged from 18 to 23 mm in the first week to 40-56 mm after 1 month.
Keywords: Three-dimensional stainless steel mini-plates, mandibular fractures, intermaxillary fixation.
Introduction
Science is always in a state of flux. The treatment options in the management of maxillofacial injuries are numerous and not without controversies. If put on the time line, the management of trauma has evolved from supportive bandages to splints and has changed from closed to open reduction and direct fixation using bone plates and screws [1, 2, 3, 4, 5]. It is known that intermaxillary fixation causes significant degree of airway obstruction which is particularly harmful for patients with chronic obstructive pulmonary disease. Thus, alternative management for jaw stabilization should be researched to avoid intermaxillary fixation [6, 7]. Rigid fixation can be achieved by compression plates, however, they have many disadvantages [8, 9]. Preference should be given to a plate which is not a compression plate but still gives enough rigidity to fractures. Michelet in 1973, ended the search for simple osteosynthesis that would guarantee fracture healing without compression which was modified, developed and put to practical use by Champy’s in 1978 [1]. While Michelet and Champy’s study was based on two-dimensional (2D) models which took only bending and torsional forces into account [1, 10] a more recent study shows at a given point in fracture site, there are three forces acting on the mandible namely; bending, torsional, and shear [11]. A three-dimensional (3D) stainless steel plate is based on the principal of a quadrangle, as a geometrically stable configuration for support [12, 13]. Inter-connections of the plate reduce the vertical displacement and shearing of the bone to minimal. Hence, intermaxillary fixation can be avoided completely [13, 14]. The term 3D mini-plates itself is a misnomer as the plates themselves are not 3D, but hold the fractured segments rigidly by resisting the 3D forces namely shearing, bending, and torsional acting on the fractured site in function.
Materials and Methods
The aim and objectives of this study were to analyze whether fracture fixation can be achieved by 3D stainless steel mini-plates, to analyze whether the patient can resume function early, to find out the need to do intermaxillary fixation and to analyze the ease of fixation of 3D stainless steel mini-plates.
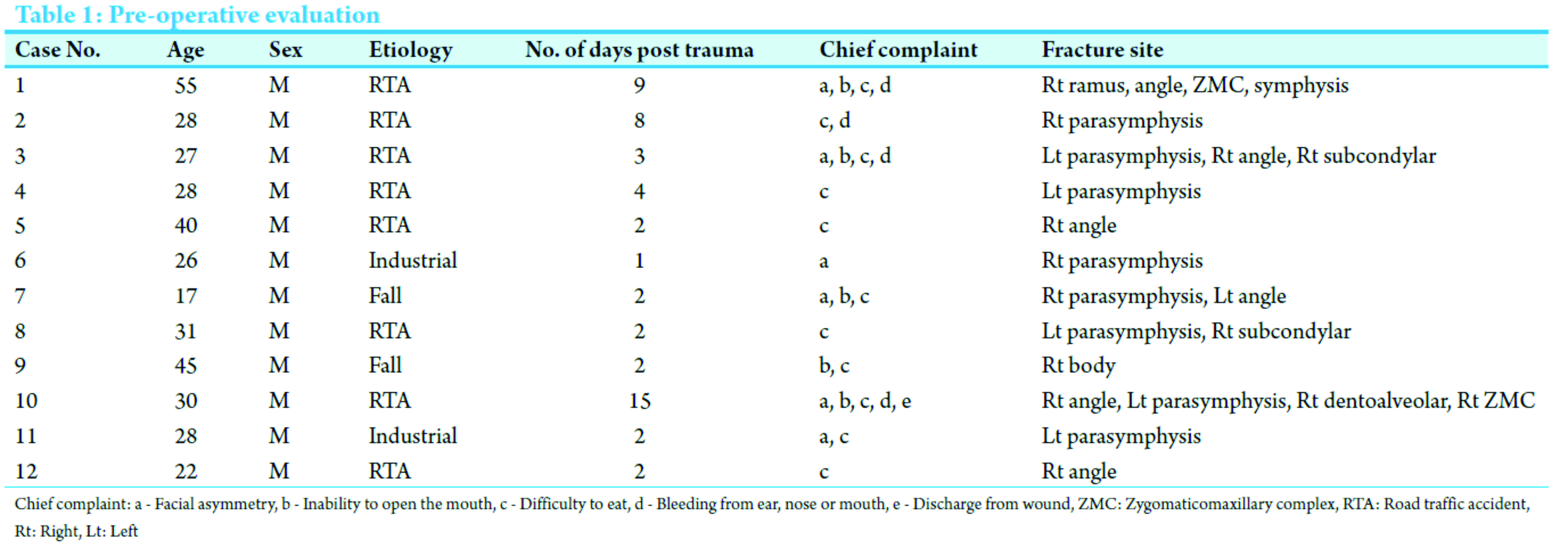
12 cases who had sustained fractures in the maxillofacial region reporting to the institute were selected (Tables 1 and 2).
Patients having fracture with displacement requiring or indicative of open reduction, those fractures, showing early signs of infection or with occlusal deformities and patients available for periodic review were included in the study.
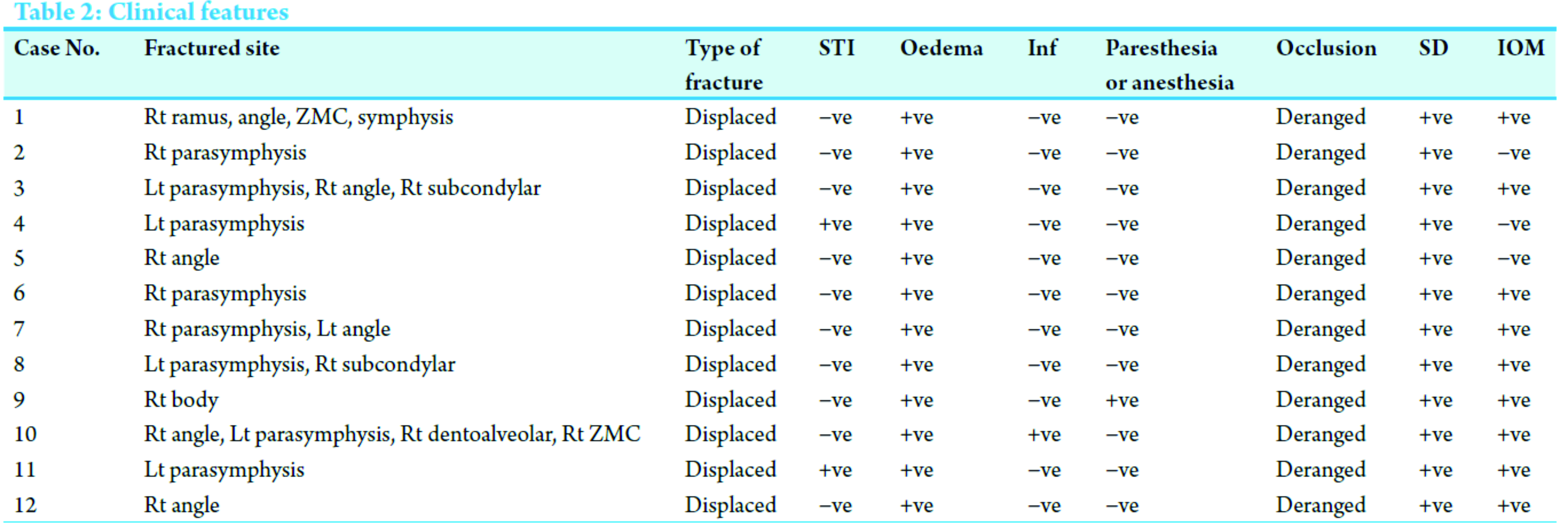
Un-displaced fractures requiring conservative treatment and those patients who would not be available for follow-up were excluded from the study. The selected cases were treated by open reduction and fixation with of 3D stainless steel mini-plates exclusively for fractures of the mandible (Fig. 1). The other associated fractures of the maxilla or those of the condyle which required open reduction and fixation were treated as per the routine using stainless steel mini-plates and screws.
The quality of stainless steel used was of AISI 316 grade [15].
The 3D stainless steel mini-plates
These are formed by joining two mini-plates with interconnecting vertical cross bars. The fundamental idea of a 3D stainless steel mini-plate is based on the principle of a quadrangle as a geometrically stable configuration for support. Increased stability is achieved by the geometric shape of the quadrangular plate rather than its thickness or length (Fig. 1).
When the mandible is in function primarily three forces are of concern namely bending, vertical displacement, and shearing [10]. In the 3D mini-plates, since the two horizontally placed mini-plates are further joined using vertical bars they act as vertical struts and minimize bending. Since the entire plate acts as a single unit vertical displacement and shearing of the bone is reduced o-minimal thus holding the fractured bony fragments in three dimensions and hence the name [13, 16, 17].
The plates used for our study had thickness of 2.5 mm and screws had a length of 6 mm and 8 mm, respectively.
Case history was taken as per standard pro forma, photographic records of operative procedure were maintained, radiographic records pre-operative, post-operative, orthopantomograms were taken at 2, 3, and 9 month intervals postoperatively [18].
Routine general physical examination and local intraoral examinations, radiographs, computed tomography scans, and all standard investigations for general anesthesia were carried out.
Standard surgical procedures were followed. The surgical approach for all the fractures was either through standard intraoral or extraoral incisions (Table 3, Fig. 2 and 3).
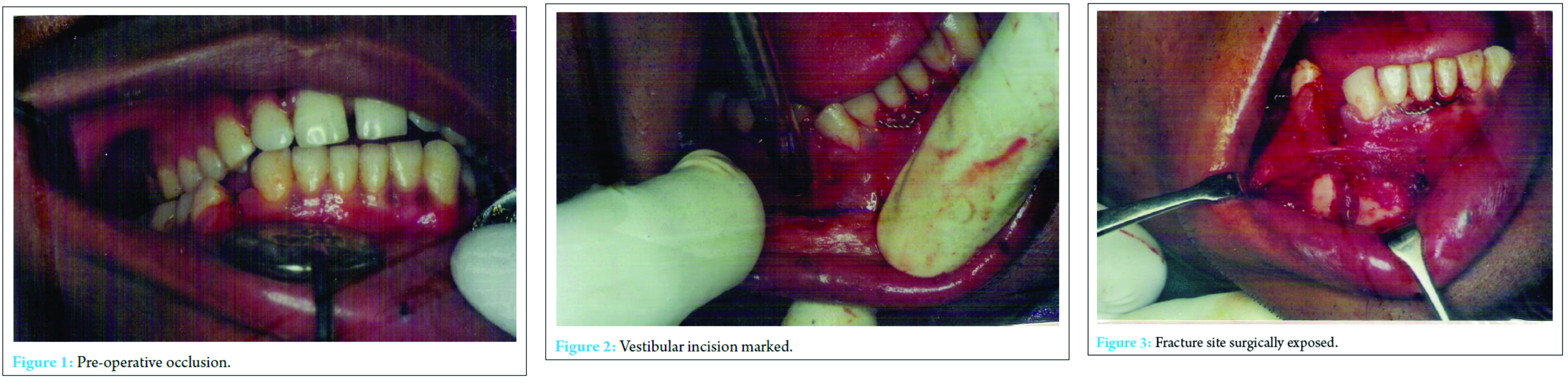
Once fracture reduction was achieved intermaxillary fixation was done, occlusion was achieved and the fractured segments were fixed using 3D plates (Fig. 4).
Fixation was achieved using either 4-holed or 6-holed 3D plates of 2.5 mm thickness and 6-8 mm length screws. Intermaxillary fixation was removed subsequently (Table 3, Fig. 5 and 6).
All patients were postoperatively put on injection ciprofloxacin 100 ml/IV/BD 5 days, injection metroniadazole 100 ml/IV/BD 5 days, injection diclofenac sodium 2 cc/IM/TID 5 days, injection dexamethasone 8 mg/IV/TID on day one and tapered thereafter and chlorhexidine mouth-wash QID 7 days.
Results (Table 4)
In our prospective study, we had an age group ranging from 17 to 55 years with 58% in the 25-34 years age group (Pie Chart 1). In total 17 fractured sites were treated using 3D plates. Road traffic accident was the etiological factor in 67% of our cases (Pie Chart 2), 42% had fracture at parasymphysis while 32% had at the angle followed by 11% at condyle and 5% at ramus, body and symphysis, respectively (Pie Chart 3). After application of the bone plates, all fractured appeared well reduced and stable. Except for two cases in which there was a concomitant subcondylar fracture intermaxillary fixation was not done in any of the cases postoperatively. Interincisal mouth opening by the end of 5th week on an average was 46.583 mm. We did not come across any complications in our study.
Discussion
With open reduction and internal fixation, the reported rate of incidence of infection ranges from 3% to 32%. Infection rates in the clinical studies in 3D mini-plates are 4-9% [19]. In our prospective study, we did not experience any complications. With the ongoing research in the development of new plating systems there was a simultaneous research on the type of biomaterials to be used for these plating systems. Titanium is proved to be a highly biocompatible material while poly (L-lactide) materials show nonspecific foreign body reaction which results in persistent swelling around the implanted site [11, 20]. Stainless steel is a time-tested material that is rigid. Although the chances of corrosion are high they can be minimized by suitable manufacturing formula and correct manipulation techniques.
While Michelet and Champy’s study was based on 2D models which took only bending and torsional forces into account [1, 11] a more recent study reveals that at a given point in fracture site there are three forces acting on the mandible, namely, bending, torsional, and shear [2]. Literature indicated that use of single noncompression mini-plate for treatment of mandibular angle fractures had a high complication rate [11]. Furthermore, it suggested that individual fracture constellations did play a part in selecting the number of plates that fractures may be benefited by the use of two noncompression mini-plates for the treatment of mandibular fractures [12, 20, 21, 22, 23, 24, 25].
Thus a more hybrid plate, which is formed by joining two mini-plates with interconnecting vertical cross bars, was used for this study. The fundamental idea of a 3D plate is based on the principle of a quadrangle as a geometrically stable configuration for support [5, 21, 22]. Interconnections of the plate reduce the vertical displacement and shearing of the bone to minimal hence intermaxillary fixation is avoided [6, 7] and the plate is reinforced by itself as a single unit. The term 3D plate itself is a misnomer as the plates are not 3D but the hold the fractured segments rigidly by resisting the 3D forces namely shearing, bending, and torsional forces acting on the fractured site in function [16, 26, 27, 28, 29]. Plate fracture was a most important complication in the study by Zix et al. Farmand and Dupoirieux had treated, 95 fractures of the mandibular body in which only one late infection and one plate fracture were reported [30, 31], however in our study no such complications were encountered. However, some amount of difficulty was experienced while adapting the 3D stainless steel plate in the symphysis region due to the excessive curvature.
Conclusion
In the prospective study, we treated 12 patients and 17 fractured sites using 3D mini-plates. In none of the cases nonunion or malocclusion was noted. Similarly except for 2 cases who had associated subcondylar fractures intermaxillary fixation was not done postoperatively. The patients were able to achieve function immediately with a reasonable level of success. The interincisal opening ranged from 18 to 23 mm in the first week to 40-56 mm after 1 month (Table 4).
Clinical message
It would be advantageous to use one 3D mini-plate instead of using two parallel mini-plates, for reduction and fixation of fractures these would also eliminate the use of intermaxillary fixation which would be advantageous to patients.
References
1. Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg 1978;6(1):14-21.
2. Raymond JF, Walter RV. Oral and Maxillofacil Trauma. 2nd ed. Pennsylvania: WB. Saunders Company; 1997. p. 474-478.
3. Eberhard K, Schilli W. Oral and Maxillofacial Traumatology. Chicago: Quiestense Publishing Co; 1982. p. 308-370.
4. Peter WB, Schendel SA, Jarg-Erich H. Maxillofacial Urgery. Vol. 1. Hongkong: Churchill Livingstone; 1999. p. 45-75.
5. Ikemura K, Kouno Y, Shibata H, Yamasaki K. Biomechanical study on monocortical osteosynthesis for the fracture of the mandible. Int J Oral Surg 1984;13(4):307-312.
6. Williams JG, Cawood JI. Effect of intermaxillary fixation on pulmonary function. Int J Oral Maxillofac Surg 1990;19(2):76-78.
7. Kayani SG, Ahmed W, Farooq M, Rehman AU, Nafees Q, Baig AM. Weight loss due to maxillomandibular fixation in mandibular fractures. Pak Oral Dent J 2015;35(3):374-376.
8. Iizuka T, Lindqvist C, Hallikainen D, Paukku P. Infection after rigid internal fixation of mandibular fractures: A clinical and radiologic study. J Oral Maxillofac Surg 1991;49(6):585-593.
9. Pogrel MA. Compression osteosynthesis in mandibular fractures. Int J Oral Maxillofac Surg 1986;15(5):521-524.
10. Kárász I, Köröndi L, Szabó G. Photoelastic stress analysis on mandibular osteosynthesis. Int J Oral Maxillofac Surg 1986;15(3):259-262.
11. Tams J, van Loon JP, Rozema FR, Otten E, Bos RR. A three-dimensional study of loads across the fracture for different fracture sites of the mandible. Br J Oral Maxillofac Surg 1996;34(5):400-405.
12. Wittenberg JM, Mukherjee DP, Smith BR, Kruse RN. Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg 1997;26(1):68-73.
13. Farmand M. The 3-D plating system in maxillofacial surgery. J Oral Maxillofac Surg 1993;51:166-167.
14. Wittenberg JM, Smith BR, Trigg DD. Treatment of mandibular fractures with 3-D titanium miniplates. J Oral Maxillofac Surg 1994;51:106-107.
15. Peter B. Killeys Fractures of the Mandible. 4th ed. Bombay: Varghese Publication House; 1991. p. 53-57.
16. Sadhwani BS, Anchlia S. Conventional 2.0 mm miniplates versus 3-D plates in mandibular fractures. Ann Maxillofac Surg 2013;3(2):154-159.
17. Meaike JD, Hollier LH. Updates in facial fracture management. J Trauma Treat 2015;4:4.
18. Kawai T, Murakami S, Hiranuma H, Sakuda M. Radiographic changes during bone healing after mandibular fractures. Br J Oral Maxillofac Surg 1997;35(5):312-318.
19. Gokkulakrishnan S, Singh S, Sharma A, Shahi AK. An analysis of postoperative complications and efficacy of 3-D miniplates in fixation of mandibular fractures. Dent Res J 2012;9(2):414-421.
20. Williams DF. Corrosion and corrosion prevention in orthopaedic implants. Proc R Soc Med 1972;65(11):1027.
21. Ellis E 3rd, Walker L. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg 1994;52(10):1032-1036.
22. Yadav S, Agarwal A, Singh S, Kumar S, Anand KR, Chhabra V. 3-D locking titanium miniplates in management of mandibular fracture: A prospective clinical study. J Dent Specialit 2015;3(1):64-67.
23. Singh V, Puri P, Arya S, Malik S, Bhagol A. Conventional versus 3-dimensional miniplate in management of mandibular fracture: A prospective randomized study. Otolaryngol Head Neck Surg 2012;147(3):450-455.
24. Kumar BP, Kumar J, Mohan AP, Venkatesh V, Kumar HR. A comparative study of three dimensional stainless plate versus stainless steel miniplate in the management of mandibular parasymphysis fracture. J Bio Innov 2012;1(2):19-32.
25. Al-Tairi NH, Shoushan MM, Saaf Khedr MM, Abd-alal SE. Comparision of three-dimensional plate versus double miniplate osteosynthesis for treatment of unfavourable mandibular angle fractures. Tanta Dent J 2015;12:89-98.
26. Jain K, Sankar K, Ramesh C. Management of mandibular interforaminal fractures using 3 dimensional locking and standard titanium miniplates-A comparative preliminary report of 10 cases. J Cranio Facial Surg 2012;40:e475-e478.
27. Balakrishnan R, Ebenezer V, Dakir A. Three dimensional titanium mini plates in management of mandibular fractures. Biomed Pharmacol J 2014;7(1):241-246.
28. Khalifa ME, El-Hawaey HE, Hussein MM. Titanium three dimensional miniplate versus convensional titanium miniplate in fixation of anterior mandibular fractures. Life Sci J 2012;9(2):1006-1010.
29. Barde DH, Mudhol A, Ali FM, Madan RS, Kar S, Ustaad F, et al. Efficacy of 3-Dimensional plates over champys miniplates in mandibular anterior fractures. J Int Oral Health 2014;6(1):20-26.
30. Zix J, Lieger O, Iizuka T. Use of straight and curved 3-dimensional titanium miniplates for fracture fixation at the mandibular angle. J Oral Maxillofac Surg 2007;65(9):1758-1763.
31. Farmand M. The 3-dimensional plate fixation of fractures and osteotomies. Facial Plast Surg Clin North Am 1995;3:39-56.
| How to Cite This Article: Gupte SH, Chaddva S, Jethwani Y, Mohandas A, Kumavat DP, Jhaveri N. Evaluation of Efficacy of Three-dimensional Stainless Steel Mini-Plates in the Treatment of Fractures of the Mandible: A Prospective Study. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):35-40. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-620-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com