[box type=”bio”] What to Learn from this Article?[/box]
This article provides a new surgical option for proximal hamstrings tendinopathy among active patients with chronic, debilitating, and refractory symptoms in lower gluteal region associated with typical imaging findings with good clinical results after 12 months of follow-up.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 69-72 | Lincoln Paiva Costa, Antônio Augusto Guimarães Barros, Carlos Cesar Vassalo, Bertrand Sonnery-Cottet, Victor Atsushi Kasuya Barbosa, Eduardo Frois Temponi. DOI: 10.13107/jocr.2250-0685.638
Authors: Lincoln Paiva Costa[1], Antônio Augusto Guimarães Barros[1], Carlos Cesar Vassalo[1], Bertrand Sonnery-Cottet[2], Victor Atsushi Kasuya Barbosa[1], Eduardo Frois Temponi[1]
[1]Department of Orthopaedics, Hospital Madre Teresa, Belo Horizonte, Minas Gerais, Brazil,
[2]Department of Orthopaedics, Hospital Ramsay-Generale de Sante, Hopital Prive Jean Mermoz, Centre Orthopedique Santy, FIFA Medical Center of Excellence, Lyon, France.
Address of Correspondence
Dr. Eduardo Frois Temponi, M.D., M.Sc.
Hospital Madre Teresa, Belo Horizonte, Minas Gerais, Brazil.
E.mail: dufrois@hotmail.com
Abstract
Introduction: Proximal hamstring tendinopathy is the result of chronic overload caused by repetitive eccentric contraction. Surgical treatment becomes an option for patients with chronic symptoms that do not respond to conservative treatment.
Case presentation: This report describes a case of a 48-year-old man, an amateur triathlete, with deep gluteal pain in the left hip for 12 months, leading to a decline in sports performance. Magnetic resonance imaging revealed abnormalities that suggested a proximal hamstring tendinopathy. Surgery was indicated following the failure of conservative treatments. Debridement of the conjoint tendon and its reinsertion associated with semimembranosus tenotomy showed good results and is thus an option for the treatment of this pathology after 12 months of follow-up.
Conclusion: This article provides surgeons with a new surgical option for this debilitating condition with clinical and functional improvement after 12 months of follow-up.
Keywords: Proximal hamstrings tendinopathy, musculotendinous lesion, sports injuries, athlete
Introduction
Diseases and injuries of the tendons are among the most common problems encountered in sports, and are difficult to treat with a direct impact on the reduction of performance [1-4]. The most common chronic lesions in the lower limbs involve the patellar and achilles tendons. Limited information exists about chronic proximal hamstring tendon disorders [5-7]. Proximal hamstring tendinopathy (PHT) is the result of chronic overload caused by repetitive eccentric contraction in hamstrings and in conjoined tendon origin [2-8]. It has been seen in athletes of various sports activities, especially in jumpers, sprinters and runners of middle and long distance [1, 9-11].
The main finding of PHT is chronic pain in the lower gluteal region and progressive pain during sports activity, especially during running with a faster pace or sprinting, and most of them also suffer from pain at the site of the ischial tuberosity while sitting for a prolonged time, occasionally radiating to the midthigh [6, 7, 9]. No acute event is associated with the onset of pain, but most patients report prior hamstring injuries. Magnetic resonance imaging (MRI) is the method of choice for the diagnosis of this condition [12-14].
The initial treatment is conservative and follows the same principles applied to other tendinopathies, including relative rest and ice to relieve symptoms, nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy and intratendinous injections of platelet-rich plasma (PRP) or corticosteroids [14-15]. However, up to 20% of patients fail to respond to conservative treatment and remain symptomatic for longer than 6 months [6]. Surgical treatment becomes an option for patients with chronic, debilitating and refractory symptoms associated with typical imaging findings of PHT [7,11,12].
This study presents a case of refractory PHT-treated surgically through modification of an existing technique for PHT treatment. The Ethics Committee at the Hospital Madre Teresa/Brazil approved this study, and a written informed consent was obtained from the patient’s family before inclusion in the study.
Case presentation
A 48 years, male, triathlete with 1.82 m, 69 kg and body mass index of 20.8 kg/m2 presented at the Orthopedic Department of Hospital Madre Teresa/Brazil in January 2015. The patient reported chronic pain in the deep gluteal region with 12 months of evolution, exacerbated mainly by race and while sitting for long periods, which caused a significant drop in his athletic performance after the onset of symptoms. Pain had nonradiating with the absence of neurovascular symptoms and without any episode of acute trauma. Previous orthopedic surgery or comorbidity was not reported.
Physical examination demonstrated pain on palpation of the left ischial tuberosity and pain at the origin of the hamstrings caused by passive
stretching of these muscles. The three pain provocation tests examined (Puranen–Orava, bent-knee stretch and modified bent knee stretch tests)
were positive. The Victorian Institute of Sport Assessment proximal hamstring tendons (VISA-H) questionnaire on initial presentation is 23 [16]. The MRI revealed thickening of the proximal hamstrings complex with intrasubstancial heterogeneity and rupture, besides bone edema in ischial tuberosity (Fig. 1). The patient underwent conservative treatment for 6 months with relative rest, NSAIDs, specific physiotherapy and percutaneous corticosteroid injection guided by ultrasound. Due to maintenance of pain and functional limitation, surgical treatment was indicated.
Surgical technique
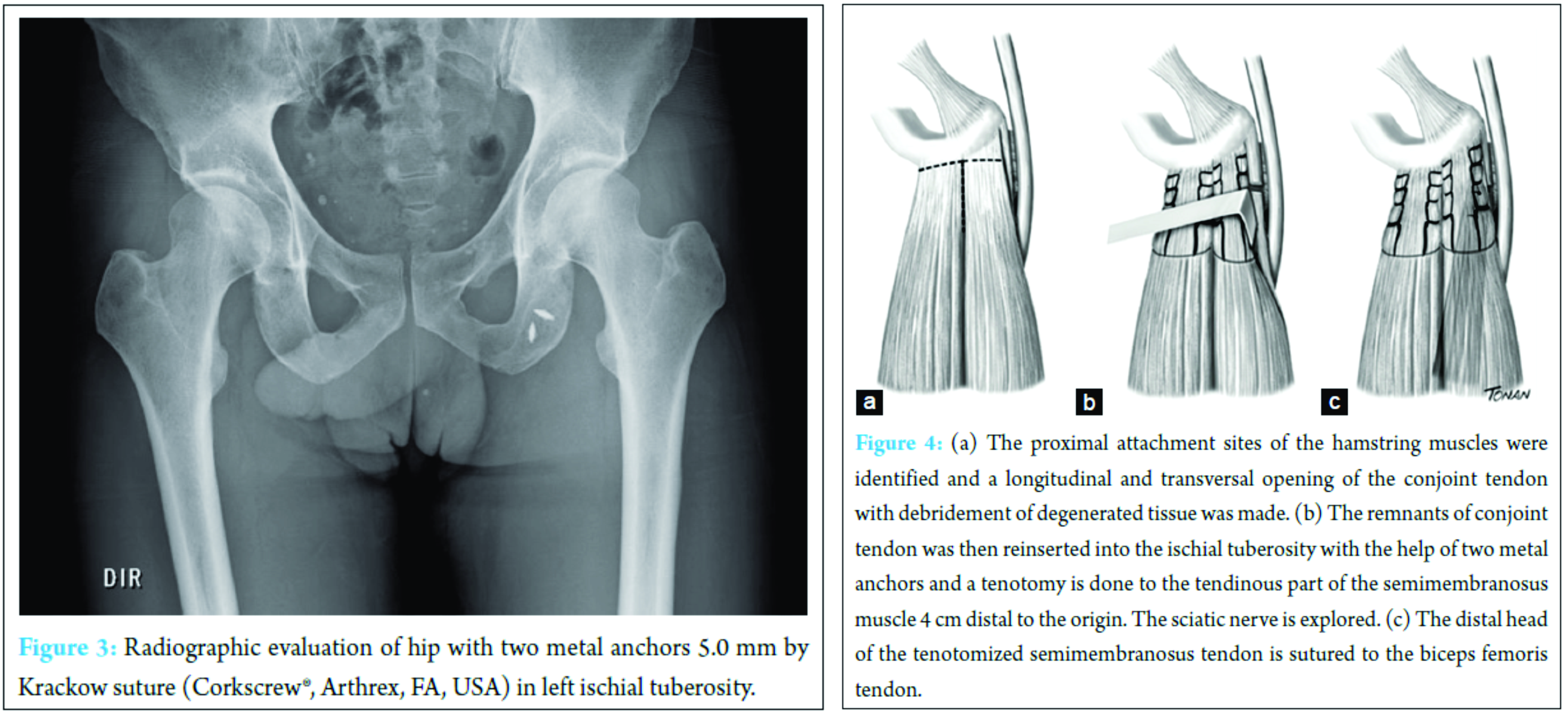
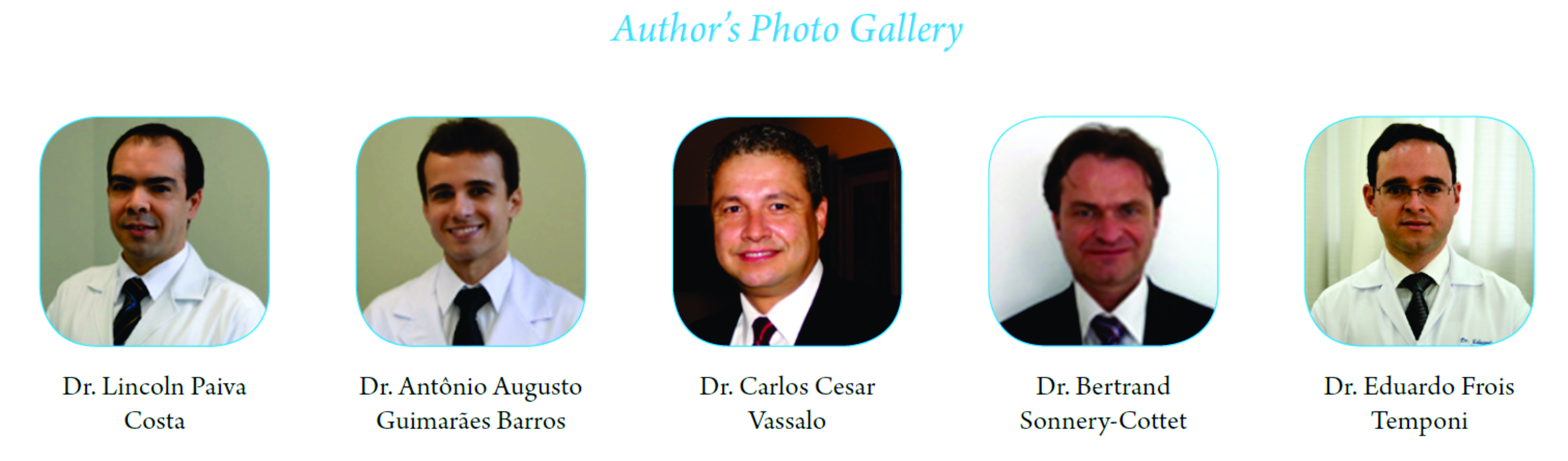
Surgery was performed under spinal anesthesia with the patient in the prone position and the knee slightly flexed to relax the hamstring muscles and the sciatic nerve. A transversal posterior incision in the gluteal fold centered in the ischial tuberosity of 6 cm was made. The lower edge of the gluteus maximus muscle was freed and the posterior cutaneous femoral nerve was identified and spared. The ischial tuberosity was easily exposed by retraction of the inferior border of the gluteus maximus muscle. The proximal attachment sites of the hamstring muscles were identified (Fig. 2) and a longitudinal and transversal opening of the conjoint tendon with debridement of degenerated tissue was made. The remnant tendon was then reinserted into the ischial tuberosity with two metal anchors 5.0-mm by Krackow suture (Corkscrew®, Arthrex, FA, USA). After this, a transversetenotomy was done to the thickened semimembranosus tendon 4 cm distal to the origin. The tenotomized semimembranosus tendon was then sutured securely to the biceps femoris tendon to prevent excessive retraction. After tenotomy, the sciatic nerve was explored and the adhesions were freed (Fig. 3).
Postoperatively, the patient was immobilized with a brace (X-Act™ ROM Hip Brace, DonJoy, CA, USA) in hip extension for three weeks. The patient was allowed to begin full weight bearing gradually during the first 3 weeks following surgery.. Swimming and water training were allowed 3 to 4 weeks after surgery. Isometric and eccentric muscle exercises and bicycling with gradually increasing time and intensity were initiated after 4 weeks. On physical examination, the patient had significantly decreased tenderness to palpation of the proximal hamstring tendon, decreased pain with the aforementioned provocative maneuvers, and a significant decrease in pain with sitting (maximum, 1/10 intensity). He was able to begin speed training approximately 12 weeks after the initial examination, at which point his VISA-H score was 83 and he had complete resolution of the previously reported pain complaints with forward bending at the trunk or sitting. He continued to do the same eccentric hamstring exercise on the treadmill without change of form. One year after initial evaluation, the patient had not had a recurrence of pain, had a VISA-H score of 100, and had returned to competition 8 months after procedure.
Discussion
PHT was first described by Puranenand Orava in 1988 with the name of hamstring syndrome [8,9]. The cause and pathophysiology of tendinopathy in humans has not yet been scientifically known, but it has been proposed that the tendon’s failed healing response to repetitive stretch and mechanical overload may be associated to the development of tendinosis [6, 8]. The differential diagnosis should consider acute hamstrings injury, piriformis syndrome, ischial bursitis and chronic posterior thigh compartment syndrome [12,17,18].
There is still no consensus on the best treatment for patients with PHT. Usually, the conservative treatment should be tried first. The same principles appy to other tendinopathies including relative rest and ice to relieve symptoms, NSAIDs drugs, eccentric strengthening of the hamstrings and core stabilization [6, 19]. The time required for full recovery ranges from 1 to 3 months and most patients have good results and return to sport activities, however, up to 20% of patients have conservative treatment failure and remain symptomatic for longer than 6 months [7, 19, 20]. In refractory cases to conventional treatment, other measures can be tried such as infiltration with corticosteroids, platelet-rich plasma therapy or shock wave [14-15].
The surgical procedure is an alternative for patients with chronic, debilitating and refractory symptoms [7]. The semimembranosus tenotomy is the classical choice for being one of the most affected in PHT, transfering stress from the semimembranosus tendon to the biceps femoris and to the semitendinosus muscles. This stress-shielding may assist the semimembranosus tendon to recover [8,12]. The difference of the technique presented in this case relates to the fact of incorporating debridement of degenerated tissue with reinsertion of remnant tendon into the ischial tuberosity, which until the present has not been described for the treatment of chronic conditions; this reinsertion takes into account the anatomy of the proximal hamstring described by Philippon et al. [21]. The elimination of fibrous scar tissue combined with intermuscular suturing allows integral healing of muscle to muscle. It is believed that this decreases the chances of re-injury by eliminating the remodeling tissue that attempts to heal the musculotendinous injury. In addition, it allows the muscle to heal to the adjacent muscle in a tension-free manner, and thus, a stronger healing process will occur [2, 11, 18].
Previous studies have shown that satisfactory results can often be expected after surgical treatment of PHT, even after failed conservative therapy [5, 8]. Lempainen et al. reported a semimembranosus tenotomy and exploration of the sciatic nerve with 89% of excellent and good results after 49 months of follow-up [8]. Benazzo et al. performed partial or multiple punctures in order to relax the myotendinous unit with an excellent result in 88% and good in 12% of cases respectively. There were no regular or poor results, and no recurrence. All patients returned to sports activity in the pre-symptom level. Both studies showed only transient complications [12].
The limitations of this study are the report of a singular case and relatively short follow-up, which means that data must be interpreted with caution when extrapolated; however, the results are significant due to rarity of injury and specific treatment. Because of low description, most of the published studies are case reports, so comparative studies addressing different methods have not been reported.
Conclusion
This article provides surgeons with a new surgical option for this debilitating condition with clinical and functional improvement after 12 months of follow-up.
Clinical message
Proximal hamstring tendinopathy (PHT) is a common and limiting clinical condition among active patients. Surgical treatment becomes an option for patients with chronic, debilitating and refractory symptoms associated with typical imaging findings. Debridement of the conjoint tendon and its reinsertion associated with semimembranosus tenotomy is a new technique described and has shown good results and is thus an option for the treatment of this pathology after 12 months of follow-up.
References
1. Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. Phys Sportsmed. 2005;33(5):32-43.
2. Petchprapa CN, Bencardino JT. Tendon injuries of the hip. Magn Reson Imaging Clin N Am. 2013;21(1):75-96.
3. Carfagno DG, Hendrix JC, 3rd. Overtraining syndrome in the athlete: current clinical practice. Curr Sports Med Rep. 2014;13(1):45-51.
4. Winsley R, Matos N. Overtraining and elite young athletes. Med Sport Sci. 2011;56:97-105.
5. Puranen J, Orava S. The hamstring syndrome. A new diagnosis of gluteal sciatic pain. Am J Sports Med. 1988;16(5):517-21.
6. Lempainen L, Johansson K, Banke IJ, Ranne J, , et al. Expert opinion: diagnosis and treatment of proximal hamstring tendinopathy. Muscles Ligaments Tendons J. 2015;5(1):23-8.
7. Benazzo F, Marullo M, Zanon G, Indino C, et al. Surgical management of chronic proximal hamstring tendinopathy in athletes: a 2 to 11 years of follow-up. J Orthop Traumatol. 2013;14(2):83-9.
8. Lempainen L, Sarimo J, Mattila K, Vaittinen S, et al. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009;37(4):727-34.
5. van der Made AD, Reurink G, Gouttebarge V, Tol JL, et al. Outcome After Surgical Repair of Proximal Hamstring Avulsions: A Systematic Review. Am J Sports Med. 2015;43(11):2841-51.
6. Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal Hamstring Tendinopathy: Clinical Aspects of Assessment and Management. J Orthop Sports PhysTher. 2016 ;46(6):483-93.
7. Lempainen L, Johansson K, Banke IJ, Ranne J, et al. Expert opinion: diagnosis and treatment of proximal hamstring tendinopathy. Muscles Ligaments Tendons J. 2015;5(1):23-8.
8. Lempainen L, Sarimo J, Mattila K, Vaittinen S, et al. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009 ;37(4):727-34.
9. Puranen J, Orava S. The hamstring syndrome. A new diagnosis of gluteal sciatic pain. Am J Sports Med. 1988 ;16(5):517-21.
10. Brudermanns B. [Suspected hamstring tendinopathy? Pain provocation!]. Sportverletz Sportschaden. 2012;26(2):64.
11. Sonnery-Cottet B, Daggett M, Gardon R, Pupim B, et al. Surgical Management of Recurrent Musculotendinous Hamstring Injury in Professional Athletes. Orthop J Sports Med. 2015 ;3(10):2325967115606393.
12. Benazzo F, Marullo M, Zanon G, Indino C, et al. Surgical management of chronic proximal hamstring tendinopathy in athletes: a 2 to 11 years of follow-up. J OrthopTraumatol. 2013;14(2):83-9.
13. De Smet AA, Blankenbaker DG, Alsheik NH, Lindstrom MJ. MRI appearance of the proximal hamstring tendons in patients with and without symptomatic proximal hamstring tendinopathy. AJR Am J Roentgenol. 2012;198(2):418-22.
14. Zissen MH, Wallace G, Stevens KJ, Fredericson M, et al. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010;195(4):993-8.
15. Davenport KL, Campos JS, Nguyen J, Saboeiro G, et al. Ultrasound-Guided Intratendinous Injections With Platelet-Rich Plasma or Autologous Whole Blood for Treatment of Proximal Hamstring Tendinopathy: A Double-Blind Randomized Controlled Trial. J Ultrasound Med. 2015;34(8):1455-63.
16. Cacchio A, De Paulis F, Maffulli N. Development and validation of a new visa questionnaire (VISA-H) for patients with proximal hamstring tendinopathy. Br J Sports Med. 2014;48(6):448-52.
17. Cacchio A, Borra F, Severini G, Foglia A, et al. Reliability and validity of three pain provocation tests used for the diagnosis of chronic proximal hamstring tendinopathy. Br J Sports Med. 2012;46(12):883-7.
18. Hamming MG, Philippon MJ, Rasmussen MT, Ferro FP, et al. Structural properties of the intact proximal hamstring origin and evaluation of varying avulsion repair techniques: an in vitro biomechanical analysis. Am J Sports Med. 2015 ;43(3):721-8.
19. Cushman D, Rho ME. Conservative Treatment of Subacute Proximal Hamstring Tendinopathy Using Eccentric Exercises Performed With a Treadmill: A Case Report. J Orthop Sports PhysTher. 2015 ;45(7):557-62.
20. Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. J Orthop Sports PhysTher. 2014;44(3):198-205.
21. Philippon MJ, Ferro FP, Campbell KJ, Michalski MP, et al. A qualitative and quantitative analysis of the attachment sites of the proximal hamstrings. Knee Surg Sports TraumatolArthrosc. 2015;23(9):2554-61.
| How to Cite This Article: Costa LP, Barros AAG, Vassalo CC, Sonnery-Cottet B, Barbosa VAK, Temponi EF. A New Technique for Surgical Treatment of Proximal Hamstring Tendinopathy in a Triathlon Athlete. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):69-72. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-638-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com