[box type=”bio”] What to Learn from this Article?[/box]
The fractured fragment of coracoid in post seizure patients can be used for addressing bony deficiency in case of recurrent dislocation of shoulder.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 81-84 | Prateek Kumar Gupta, Ashis Acharya, Amit Mourya DOI: 10.13107/jocr.2250-0685.644
Authors: Prateek Kumar Gupta[1], Ashis Acharya[1], Amit Mourya[1]
[1]Department of Orthopaedics, Sir Ganga Ram Hospital, Rajendra Nagar, New Delhi, India.
Address of Correspondence
Dr. Prateek Kumar Gupta,
Room No. 1218-A, Department of Orthopaedics, Sir Ganga Ram Hospital, Rajendra Nagar, New Delhi, India.
E-mail: sportsmedicinedelhi@yahoo.com
Abstract
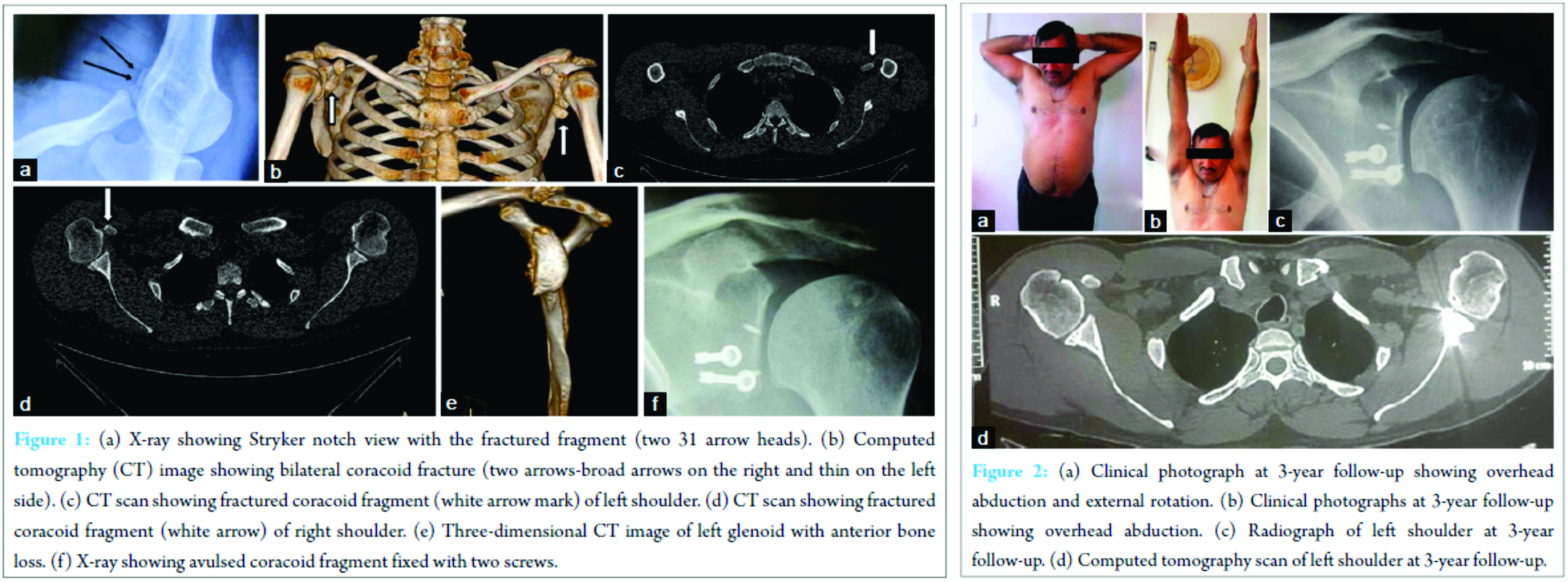
Introduction: Coracoid fractures are often missed since the fracture is not visualized in a routine anteroposterior view of the shoulder and special views are not ordered. Shoulder dislocation is common but it is rare to have a dislocation with a coracoid fracture. The purpose of this paper is to present the rare occurrence of bilateral coracoid fractures in a patient with unilateral anterior shoulder instability managed using the same fractured coracoid fragment by the latarjet procedure.
Case Report: We report a case of 48‑year‑old male who presented to us with a history of recurrent dislocations of the left shoulder. He had frequent episodes of tonic–clonic seizures 5 years back. He was diagnosed to be suffering from neurocysticercosis of the brain for which he was successfully treated. He did not have any episode of seizure later, but he continued to have repeated episodes of dislocation on his left side only. On examination of his left shoulder, he had normal range of motion. He was found to be very apprehensive, even in the midrange. This made us to suspect glenoid bone loss and hence both magnetic resonance imaging and three‑dimensional computed tomography (CT) scan of the left shoulder were ordered. The CT scan revealed bilateral coracoid fractures along with glenoid bone loss. An open bony procedure including iliac crest bone graft was planned after a diagnostic arthroscopy keeping in mind that the latarjet procedure may not be possible due to the coracoid fracture. During the operation, we found that the coracoid fragment was large enough to perform a latarjet procedure rather than doing an iliac crest bone graft. This itself provided stability of the shoulder on abduction and external rotation by providing a bony block not requiring any further procedure for the Hill‑Sachs lesion.
Conclusion: Epileptic patients should undergo CT scan evaluation for glenoid bone loss, large Hill‑Sachs lesion and to rule out coracoid fractures to plan for bony stabilization procedure and since we have used the same fractured coracoids fragment for latarjet procedure and found to be successful, this add on the knowledge to the orthopedic community.
Keywords: Coracoid process fracture, latarjet procedure, shoulder dislocation, shoulder joint, Hill‑Sachs lesion, superior labral anterior‑posterior.
Introduction
The coracoid process is an important link between the thorax and the upper limb providing attachments to several important structures around the shoulder. Multiple attachments in varying directions predispose the coracoid process to an avulsion fracture [1]. The prominence of the structure makes it prone to direct trauma. Shoulder dislocation is common but it is rare to have a dislocation with a coracoid fracture [2, 3]. Only a few studies are reported in the literature [4, 5]. Coracoid fractures are often missed since the fracture is not visualized in a routine anteroposterior (AP) view of the shoulder, and special views are not ordered [6, 7, 8]. The purpose of this paper is to present the rare occurrence of bilateral coracoid fractures in a patient with unilateral anterior shoulder instability managed using the fractured coracoid fragment by the latarjet procedure.
Case Report
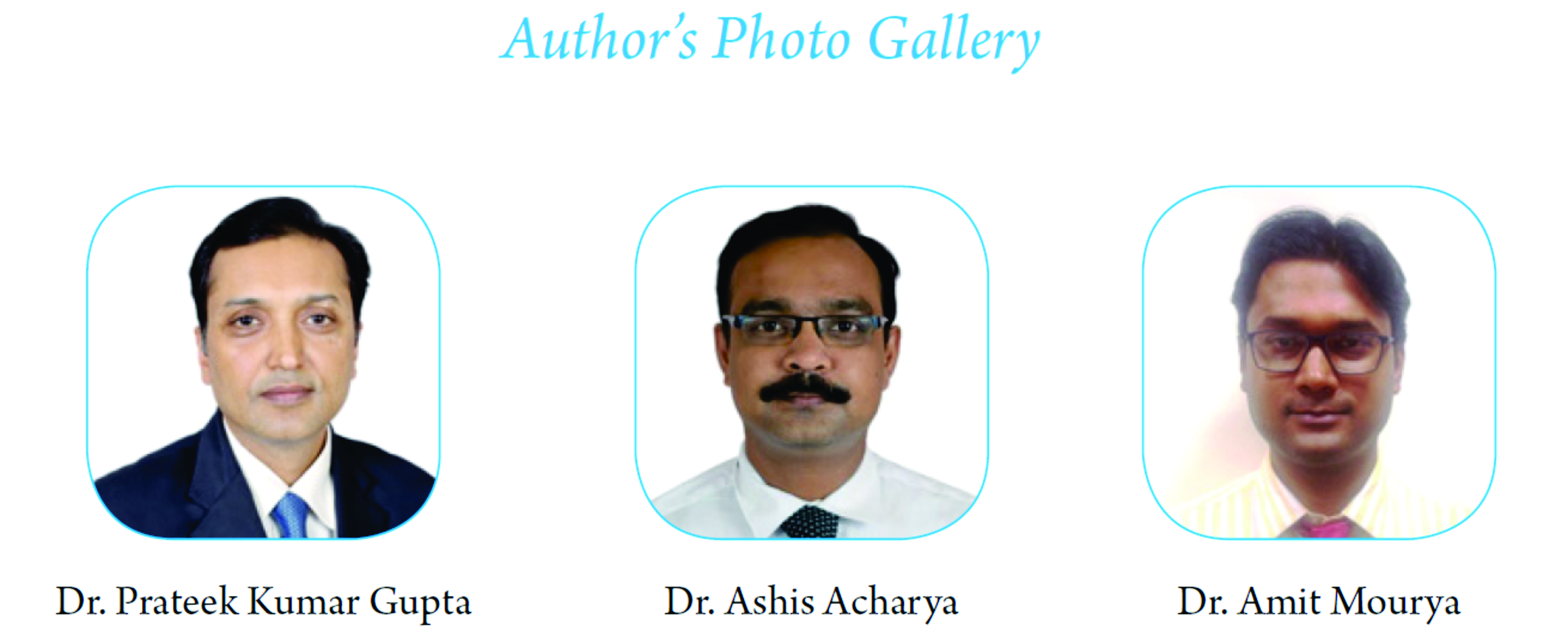
We report a case of 48‑year‑old male who presented to us with a history of recurrent dislocations of the left shoulder last 5 years with no instability on the right side. He had frequent episodes of tonic–clonic seizures 5 years back. During one episode, he dislocated his left shoulder for which he visited a local doctor who reduced it under sedation. He was diagnosed to be suffering from neurocysticercosis of the brain for which he was successfully treated. He did not have any episode of seizure later, but he continued to have repeated episodes of dislocation on his left side only. His left shoulder would dislocate during routine activities and even in sleep. Each episode was painful but he managed to reduce himself. On examination of his left shoulder, he had normal range of motion. His rotator cuff strength was adequate. Anterior drawer was Grade 2. He was found to be very apprehensive, with apprehension even in the midrange. This made us suspect glenoid bone loss and hence both magnetic resonance imaging (MRI) and three‑dimensional computed tomography (CT) scan of left shoulder were ordered. We did not suspect a coracoid fracture looking at the AP X‑ray of the left shoulder which he was carrying to the clinic. The Stryker notch view done for the Hill‑Sachs lesion showed a bony fragment (Fig. 1a). No signs of axillary or musculocutaneous nerve injuries were noted. The CT scan was performed for the left shoulder, however, as per protocol, data were obtained for the right shoulder to compare and assess the actual glenoid bone loss. The CT scan revealed bilateral coracoid fractures which were strikingly similar (Fig. 1b). The fractured fragment of the coracoid on the left side (Fig. 1c) was more displaced than the right side (Fig. 1d). The anterior glenoid bone loss in the left shoulder was found to be significant (>25%) with inverted pear shape (Fig. 1e). MRI of the left shoulder showed an anterior labrum tear with a Type II superior labral anterior‑posterior (SLAP) and a Hill‑Sachs lesion. The supraspinatus, infraspinatus, and the subscapularis tendons were intact. An open bony procedure including iliac crest bone graft was planned after a diagnostic arthroscopy keeping in mind that the latarjet procedure may not be possible due to the coracoid fracture. Preoperatively, the details of the possible bony procedure and biceps tenotomy were discussed in detail, and informed consent obtained from the patient. The patient was put in a beach chair position for the left shoulder surgery, followed by a diagnostic round to assess the bone loss which was found to be coinciding with the CT finding of more than 25% anterior glenoid bone loss. Biceps was tenotomized and the SLAP was debrided with a shaver. The deltopectoral approach was used. The conjoint tendon with the bony fragment of coracoid showed a retraction of about 6 cm from its original position. The musculocutaneous nerve was isolated and finger dissected to mobilize it. To our relief, the coracoid fragment was large enough with its cortical support intact to hold two screws which made it feasible to perform a latarjet procedure rather than doing an iliac crest bone graft. The coracoid fragment was predrilled and later fixed to the prepared bed of the anterior glenoid wall (Fig. 1f). This itself provided stability of the shoulder on abduction and external rotation by providing a bony block not requiring any further procedure for the Hill‑Sachs lesion. Two single loaded titanium anchors (2.8 mm) were used for the anterior labrum and capsule closure. This also made the graft extra‑articular as described by Burkhart et al. [9]. After the completion of the procedure, the joint showed good stability. The post‑operative period was uneventful and the patient was followed up at 2 weeks, 6 weeks, 3 months, 1‑year, and 3 years postoperatively. The range of movement gradually improved over the 3‑year follow‑up to 160° forward flexion, 40° extension, 170° abduction, 70° internal, and 85° external rotation at present (Figs. 2a and b) without any instability. The Oxford Instability Score and Rowe’s Instability Score at 3 years postoperatively measured 14 and 95, respectively [10, 11]. The radiographs and CT images obtained at the 3‑year follow‑up showed a well incorporated coracoid fragment with complete filling up of the preoperative anterior glenoid bone defect (Fig. 2c and d).
Discussion
To date fractures of the coracoid are infrequently recognized and reported. The reasons for missing this fracture in cases of patients with anterior dislocation have been the dominance of the symptoms of dislocation which mask the symptoms of coracoid fracture as rightly pointed by Garcia‑Elias and Salo in 1985 [12]. The fracture may come into notice if it impedes the reduction as reported by Wong‑Chung and Quinlan [2]. Many X‑ray views targeting the coracoid have been described; however, these are specific views which are not widely practiced [8]. Coracoid view described by Protass et al. in 1975 is based on 30‑350 angulation of the X‑ray tube with the patient supine [7]. Acromioclavicular dislocation was the most common lesion seen in the 60 cases of the total 67 cases. The classification of these fractures as described by Eyres et al. is practical and gives an insight into the pathomechanics of the fracture [13]. They classified these into five types. Types I, II, and III are avulsion fractures caused by the traction forces from the attached tendons and ligaments. Types IV and V are more severe injuries due to shear forces. The fractures described in this report are Type II avulsion fractures. To our knowledge, this is first such case report in the English literature where the avulsed fragment of the coracoid was fixed to the anterior glenoid addressing the anterior instability of the patient. The case we report was assessed for the bilateral condition to rule out fusion failure as reported by Kim et al. in 1999 [14]. Although the patient had no instability on the right side, patients with seizure episodes have shown, in the past, to possess higher frequency of bilateral involvement of the shoulders as reported by Buhler and Gerber in 2002 [15]. They did not report any case of coracoid fracture in a series of 26 cases with 17 anterior dislocations. They concluded that skeletal reconstruction is necessary to obtain good clinical stability especially in anterior dislocation which is difficult to treat.
Conclusion
In conclusion, bilateral coracoid fractures with anterior shoulder dislocation are rare injuries. Coracoid fractures are often missed on routine AP view of the shoulder unless a high degree of suspicion is maintained. Epileptic patients should undergo CT scan evaluation for glenoid bone loss, large Hill‑Sachs lesion and to rule out coracoid fractures to plan for bony stabilization procedure.
Clinical Message
In patient who has had coracoids fracture due to trauma or seizure, the broken fragment of coracoids even after 5 years can be used to augment defect in latarjet procedure rather than using for iliac crest bone graft which has less desirable result and more comorbidities.
References
1. Asbury S, Tennent TD. Avulsion fracture of the coracoid process: A case report. Injury 2005;36(4):567‑568.
2. Wong‑Chung J, Quinlan W. Fractured coracoid process preventing closed reduction of anterior dislocation of the shoulder. Injury 1989;20(5):296‑297.
3. Wong‑Pack WK, Bobechko PE, Becker EJ. Fractured coracoid with anterior shoulder dislocation. J Can Assoc Radiol 1980;31(4):278‑279.
4. Cottias P, le Bellec Y, Jeanrot C, Imbert P, Huten D, Masmejean EH. Fractured coracoid with anterior shoulder dislocation and greater tuberosity fracture – Report of a bilateral case. Acta Orthop Scand 2000;71(1):95‑97.
5. Taneja AK, Pecci Neto L, Skaf A. Bilateral anterior glenohumeral dislocation and coracoid processes fracture after seizure: Acute MRI findings of this rare association. Clin Imaging 2013;37(6):1131‑1134.
6. Benchetrit E, Friedman B. Fracture of the coracoid process associated with subglenoid dislocation of the shoulder. A case report. J Bone Joint Surg Am 1979;61(2):295‑296.
7. Protass JJ, Stampfli FV, Osmer JC. Coracoid process fracture diagnosis in acromioclavicular separation. Radiology 1975;116(1):61‑64.
8. Zilberman Z, Rejovitzky R. Fracture of the coracoid process of the scapula. Injury 1981;13(3):203‑206.
9. Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007;23(10):1033‑1041.
10. Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder stability: The development and validation of a questionnaire. J Bone Joint Surg Br 1999;81(3):420‑426.
11. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: A long‑term end‑result study. J Bone Joint Surg Am 1978;60(1):1‑16.
12. Garcia‑Elias M, Salo JM. Non‑union of a fractured coracoid process after dislocation of the shoulder. A case report. J Bone Joint Surg Br 1985;67(5):722‑723.
13. Eyres KS, Brooks A, Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br 1995;77(3):425‑428.
14. Kim SJ, Km JS, Kim HJ, Yu, HW. Bilateral unfused coracoid process. J Korean Med Sci 1998;13:563‑565.
15. Buhler M, Gerber C. Shoulder instability related to epileptic seizures. J Shoulder Elbow Surg 2002;11(4):339‑344.
| How to Cite This Article: Gupta PK, Acharya A, Mourya A. Bilateral Coracoid Avulsion Fractures with Unilateral Anterior Instability with Glenoid Bone Loss: Use of Avulsed Fragment for Reconstruction of Glenoid. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):81-84. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-644-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com