[box type=”bio”] What to Learn from this Article?[/box]
Deep vein thrombosis of lower limbs is a serious medical condition, but elective procedures can be attempted safely after inserting inferior vena cava filter.
Case Report | Volume 7 | Issue 1 | JOCR January – February 2017 | Page 16-19 | Saurabh Agarwal, Ashish Rana, Gaurav Gupta, Deepak Raghav, Rajeev K Sharma. DOI: 10.13107/jocr.2250-0685.668
Authors: Saurabh Agarwal[1], Ashish Rana[1], Gaurav Gupta[1], Deepak Raghav[1], Rajeev K Sharma[1]
[1] Department of Orthopaedics, Indraprastha Apollo Hospital, New Delhi, India.
Address of Correspondence
Dr. Saurabh Agarwal,
Department of Orthopaedic, Indraprastha Apollo Hospital, New Delhi -110 076, India.
E-mail: saurabh.24090@gmail.com
Abstract
Introduction: Deep vein thrombosis (DVT) following total knee arthroplasty (TKA) and its associated complication, pulmonary thromboembolism (PTE) remains a challenge for orthopedic surgeons. There are wide ranges of predisposing factors which are both patient specific as well as procedure associated, responsible for DVT. PTE is a well-known fatal complication of DVT which may be life-threatening. Medical management and early mobilization are necessary for the management of DVT. Fatal PTE can be prevented by implantation of inferior vena cava (IVC) filter in at risk patients.
Case Report: We are presenting a rare case report of 75-year-old female with severe osteoarthritis of the left knee with DVT of the left lower limb in which TKA was done in a prediagnosed case of DVT. IVC filter placement was done before TKA for prevention of fatal PTE, and medical management was done for DVT.
Conclusion: Prevention of fatal thromboembolism is of prime importance in the management of DVT. This can be achieved by implanting IVC filter. TKA is necessary for early pain free mobilization of the patient, which prevents progression of DVT and early recovery. IVC filter placement prevents fatal thromboembolism. Hence, treatment of both osteoarthritis of knee by TKA and DVT can be done simultaneously.
Keywords: Deep vein thrombosis, total knee arthroplasty, acute thromboembolism, osteoarthritis, inferior vena cava filter.
Introduction
Pulmonary thromboembolism (PTE) is one of the most serious complications of long recumbency in hospitalized patients. Etiology of deep vein thrombosis (DVT) has been explained by Virchow’s triad which stated that thrombosis is related to vessel wall changes, blood flow and coagulability [1]. Venostasis and tissue hypoxia with resultant endothelial changes are the major cause of DVT after total knee arthroplasty (TKA). Prolonged immobilization due to severe osteoarthritis of knee is itself a contributing factor for the development of DVT [2]. The classical sign and symptoms of DVT include pain in calf at rest and on foot dorsiflexion, pitting edema above the medial malleolus and palpable difference in temperature between the legs. Some patients may develop PTE without showing any clinical signs of DVT, so other tests are necessary for diagnosis of DVT [3]. Most routinely done investigation is venous Doppler, which is nonexpensive, noninvasive and readily available. Venous Doppler shows sensitivity of 89% and specificity of 100% [4]. We are presenting a case report of a patient in which TKA was done in a diagnosed case of DVT. We assessed both the patient specific predisposing factors and procedure-associated risk factors [5] of DVT in this patient. This is a rare case report as TKA in a diagnosed case of DVT had not been published in written literature.
Case Report
A total of 75-year-old obese female with body mass index (BMI) of 36.5 (obese Class II; according to WHO classification), came with complaint of pain in both knees (left >> right) with difficulty in walking for last 10 years with swelling on left leg for last 1 week. She had severe pain in the left knee which badly affected her activities of daily living. She was a known case of hypertension for last 8 years and hypothyroidism for last 20 years. She was recently diagnosed with diabetes mellitus. X-rays of the left knee (Fig. 1) showed advanced osteoarthritis, and she was advised for left TKA.On physical examination, the patient had swelling and mild tenderness over the left leg without apparent signs of venous thrombosis. Distal pulses of the left leg were feeble and Homan’s Sign was negative. Doppler ultrasound of the lower extremity was done which showed acute thrombosis involving femoral and popliteal vein in the left leg (Fig. 2).
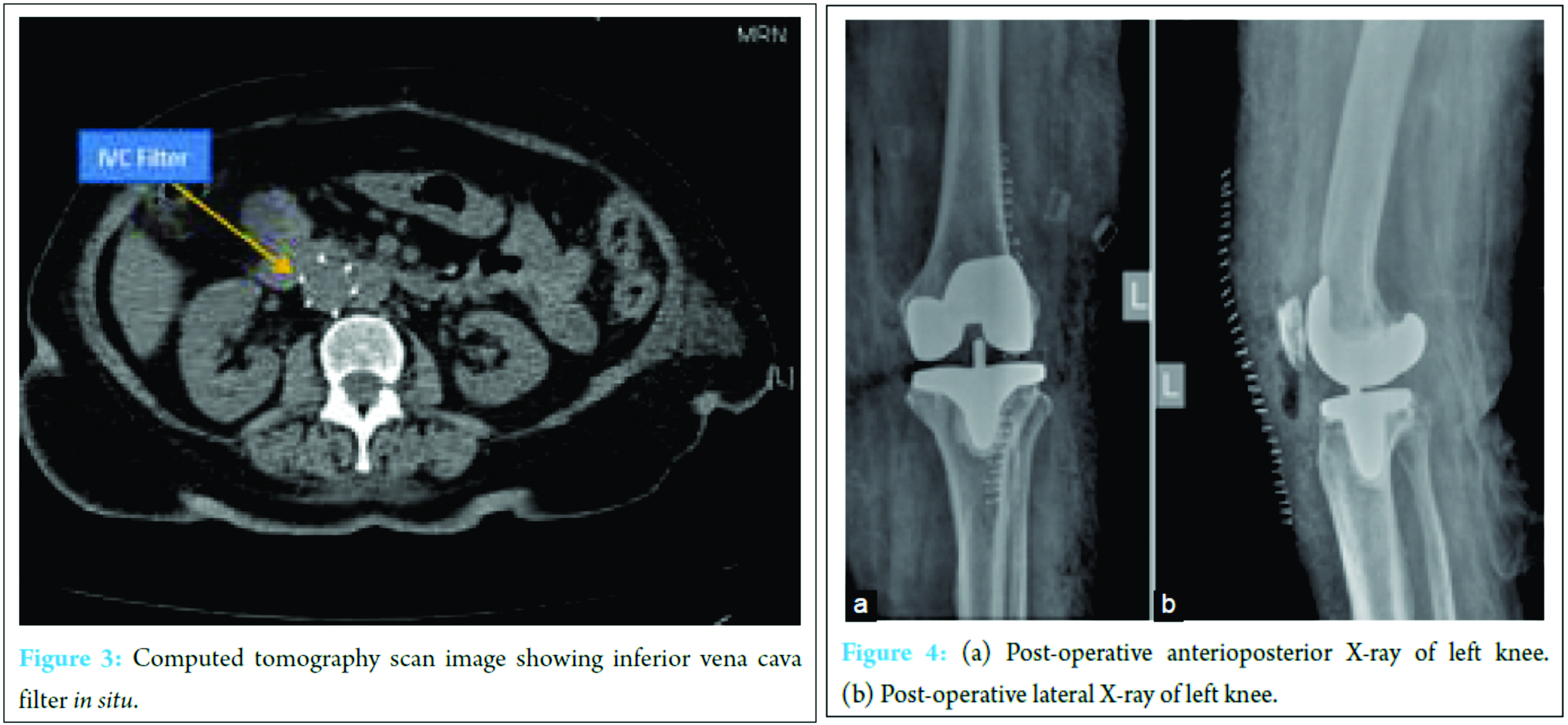
The patient was subsequently evaluated by a senior vascular surgeon. She was advised treatment for DVT and to wait for at least 3 months before TKA. However, the patient was so disabled by the knee pain that she insisted on scheduling the surgery as early as possible. Published literature did not show any case report in which TKA was done in a diagnosed case of DVT. Although a number of surgical procedures had been done in last in patients with DVT [6, 7, 8]. In all such patients, inferior vena cava (IVC) filter was implanted to prevent serious complications of DVT due to thromboembolism, during and after surgery. The goal of IVC filter was to prevent fatal PTE. Therefore informed consent was taken, explaining to the patient, all the pros and cons of the surgery. Retrievable IVC filter (OPTEASE® Retrievable Vena Cava Filter, Cordis Corporation) was implanted through right femoral vein under fluoroscopy guidance one day before the surgery (Fig. 3). The patient was given enoxaparin sodium injection 40 mg (Clexane, Sanofi) 12 h before surgery.
TKA using PS 150 (Depuy Orthopaedics, Inc. USA) on the left side was done (Fig. 4a and b) under general anesthesia. The patient was not given regional anesthesia in the form of spinal or epidural anesthesia to prevent from intradural bleeding which may cause subdural hematoma leading to neurological deficit. Tourniquet was applied only at the time of cementing of implants. Wound was closed in multiple layers and suction drain was not used. Postoperatively the patient was put on therapeutic dose of DVT management. Injection enoxaparin 30 mg twice a day, subcutaneously was given for 6 days and then she was put on tablet rivaroxaban (Xarelto, Bayers) [9] 15 mg twice a day for 3 weeks [10] and then on 20 mg once a day for 3 months. DVT Foot Pump was applied immediately after surgery in the recovery room. DVT Stockings were applied on 2nd post-operative day after change of dressings. Physiotherapy and walker aided mobilization was started on 1st post-operative day. Patient developed swelling over the knee with multiple ecchymotic patches. The surgical wound heals well at 2 week time. The pain and swelling over the lower limb had subsided over the period of 3-month. The patient is now 1 year post-operative follow-up and is doing well.
Discussion
Risk factors of DVT are prolonged bed rest or inactivity, obesity, smoking, and chronic venous diseases like varicose vein and vasculitis [2]. TKA is also itself a risk factor for the development of DVT. Sometimes even asymptomatic DVT can lead to lethal complication such as PTE [3, 11]. However, it is not necessary that all DVT will give rise to pulmonary embolism [12]. Our patient had many predisposing factors which increase the risk of DVT including old age, obesity (high BMI 36.5), diabetes mellitus, hypertension, and hypothyroidism. She was unable to walk unaided and had difficulties in doing activities of daily living, because of severe osteoarthritis of the left knee, thus leading a sedentary life. Early mobilization of patient was necessary to prevent progression of DVT after surgery. Major concern was prevention of fatal PTE, because calf thrombi may dislodge and can produce fatal PTE [11]. In consultation with vascular surgeon, IVC filter was implanted to prevent any complication of DVT due to thromboembolism, during and after surgery. The goal of IVC filter was to prevent fatal PTE. After surgery, aggressive post-operative rehabilitation program and therapeutic management of DVT was started. IVC filters have shown to be effective in the prevention of pulmonary embolism [13]. Absolute indications for IVC filter implantation is failure or contraindication to anticoagulation. Prophylactic implantation of IVC filter has also been advocated in patients with a high risk of thromboembolic disease [14]. This group includes patients who need to undergo surgery with concomitant high risk of development of PTE. Temporary placement of retrievable IVC filter is a reasonable choice for these patients. Implantation of IVC filter is not without complications. It can act as a nidus for thrombus formation. Migration of filter and IVC perforation may also occur. In our patient OPTEASE®, Retrievable Vena Cava Filter was used. It is safe and effective in the prevention of PTE. There is a scarcity of literature about the prophylactic use of IVC filters in orthopedic surgery, and there was no reported case of TKA successfully done in a patient of DVT. Muratani et al. used IVC filter for the management of DVT in the trimalleolar fracture fixation intraoperatively [6]. Rosenthal et al. managed cases of polytrauma which were at high risk for development of thromboembolism by putting temporary IVC filter [7]. In these subsets of patients, chemical prophylaxis cannot be started due to the possibility of bleeding from the fracture sites. Seto et al. also used IVC filter intraoperatively, during hysterectomy for uterine leiomyoma to prevent PTE in a diagnosed DVT patient [8]. According to American Academy of Orthopaedic Surgeons guideline for DVT prophylaxis, IVC filter in elective knee or hip arthroplasty may be considered in such situations where chemoprophylaxis is contraindicated and/or known case of DVT [15].
Conclusion
Prolonged immobilization due to severe osteoarthritis of knees is a contributing factor for the development of DVT [2]. In the management of DVT, prevention of fatal thromboembolism is of prime importance. This can be achieved by implanting IVC filter. Hence, treatment of both osteoarthritis of knee by TKA and DVT can be done simultaneously. TKA is necessary for the early pain free mobilization of the patient, which prevents progression of DVT and IVC filter placement is necessary to prevent fatal episode of thromboembolism.
Clinical Message
Pulmonary embolism is a devastating complication post DVT which can be prevented by implantation of IVC filters. Elective surgeries like TKA can be attempted in patients of osteoarthritis of knee with DVT, after implantation of IVC filters and taking necessary precautions.
References
1. Available from: http://www.virchow’s triad? – free online library. [Last retrieved on 2009 Feb 10].
2. Coiteux I, Mazzolai L. Deep vein thrombosis: epidemiology, risk factors and natural history. Praxis (Bern 1994) 2006;95(12):455-459.
3. Lambie JM, Mahaffy RG, Barber DC, Karmody AM, Scott MM, Matheson NA. Diagnostic accuracy in venous thrombosis. Br Med J 1970;2(5702):142-143.
4. Markel A, Weich Y, Gaitini D. Doppler ultrasound in the diagnosis of venous thrombosis. Angiology 1995;46(1):65-73.
5. Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004;126 3 Suppl:338S-400S.
6. Muratani T, Tsunemi K, Yazu M, Ishizu T. Case of trimalleolar ankle fracture managed by placement of a temporary inferior vena cava filter by an anesthesiologist. Masui 2014;63(8):682-685.
7. Rosenthal D, Wellons ED, Levitt AB, Shuler FW, O’Conner RE, Henderson VJ. Role of prophylactic temporary inferior vena cava filters placed at the ICU bedside under intravascular ultrasound guidance in patients with multiple trauma. J Vasc Surg 2004;40(5):958-964.
8. Seto A, Fukuyama H, Niijima K, Takenaka I, Kadoya T. Anesthetic management of a patient with deep venous thrombosis using temporary inferior vena cava filter. Masui 2000;49(3):302-304.
9. Available from: http://www.xareltohcp.com/dosing-and-administration/ dvt-pe.
10. Kearon C, Akl EA. Duration of anticoagulant therapy for deep vein thrombosis and pulmonary embolism. Blood 2014;123(12):1794-1801.
11. Giachino A. Relationship between deep-vein thrombosis in the calf and fatal pulmonary embolism. Can J Surg 1988;31(2):129-130.
12. Hanel KC, Abbott WM, Reidy NC, Fulchino D, Miller A, Brewster DC, et al. The role of two noninvasive tests in deep venous thrombosis. Ann Surg 1981;194(6):725-730.
13. Athanasoulis CA, Kaufman JA, Halpern EF, Waltman AC, Geller SC, Fan CM. Inferior vena caval filters: review of a 26-year single-center clinical experience. Radiology 2000;216(1):54-66.
14. Kinney TB. Update on inferior vena cava filters. J Vasc Interv Radiol 2003;14(4):425-440.
15. Available from: http://www.aaos.org/research/guidelines/VTE/VTE_summary_of_recs.pdf.
| How to Cite This Article: Saurabh Agarwal, Ashish Rana, Gaurav Gupta, Deepak Raghav, Rajeev K Sharma. Total Knee Arthroplasty in a Diagnosed Case of Deep Vein Thrombosis – Our Experience and Review of Literature. Journal of Orthopaedic Case Reports 2017 Jan-Feb ;7(1):16-19. Available from: https://www.jocr.co.in/wp/wp-content/uploads/8.-2250-0685.668.pdf |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com