[box type=”bio”] What to Learn from this Article?[/box]
Histopathology should be thoroughly reviewed as it helps determine the treatment plan and determine the type of prognosis required for the patient.
Case Report | Volume 7 | Issue 1 | JOCR January – February 2017 | Page 61-64 | Ruchika Ravi Agrawal, Jyoti Dilip Bhavthankar, Mandakini Subhash Mandale, Purva Prakash Patil. DOI: 10.13107/jocr.2250-0685.690
Authors: Ruchika Ravi Agrawal[1], Jyoti Dilip Bhavthankar[1], Mandakini Subhash Mandale[1], Purva Prakash Patil[1]
[1] Department of Oral Pathology, Government Dental College and Hospital, Aurangabad, Maharashtra, India.
Address of Correspondence
Dr. Ruchika Ravi Agrawal,
Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad – 431 001,
Maharashtra, India.
E-mail: ruchikaagrawal26@gmail.com
Abstract
Introduction: Osteosarcoma is a malignant mesenchymal tumor whose cancerous cells produce osteoid matrix. It is a common primary malignant bone tumor, representing 23% of total head and neck malignancies. Osteosarcomas of the jaws are rare lesions, representing only 4-7% of all osteosarcomas. This presentation discusses the clinical, radiographical, and histopathological features of a case of osteosarcoma of the mandible with unusual histopathological appearance.
Case Report: A 21-year-old male patient reported with a diffuse swelling of the right side of mandible with dull ache and increasing difficulties with eating and speech. Incisional biopsy done showed a histopathological picture of osteosarcoma and osteoblastoma. Hemimandibulectomy was done and the histopathology showed varying patterns of the lesion-like osteoblastoma-like osteosarcoma and osteoblastic variant of osteosarcoma. Focal areas in the lesion also showed fibrohistiocytic differentiation which may be mistaken for malignant fibrous histiocytoma. Hemangiopericytomatous appearance was also seen. Hence, it was necessary to differentiate between all the lesions as the treatment plan for all these lesions is different. Rarely, tumor may show a spectrum of histopathology as seen here in a case of osteosarcoma of the mandible.
Conclusion: The treatment plan and prognosis for each type of these lesions are different. Thus, thorough histopathological evaluation will help in accurate diagnosis, proper treatment planning, and prognosis of these lesions.
Keywords: Osteosarcoma, bone, mandible, histologically.
Introduction
Osteosarcoma, sometimes referred to as osteogenic sarcoma, is the most common primary bone tumor seen in adolescents and young adults [1]. Osteosarcomas of the jaws are rare and they are highly malignant neoplasms of the bone whose diagnoses are challenging [2]. There is a predilection of mandibular osteosarcomas in older patients (mean age: 34-36 years) [1]. It accounts for about 23% of all sarcomas [3]. About 4-6% osteosarcomas occur in the maxillofacial region [4]. The exact cause is unknown, but there are various predisposing factors that may cause osteosarcoma. These include rapid bone growth (increased incidence during adolescent growth spurt), person receiving radiation, genetic predisposition, bone dysplasias including Paget’s disease, fibrous dysplasia, enchondromatosis, hereditary multiple exostoses, and retinoblastoma [5]. The radiographic appearances of these tumors are radiolucent, radiopaque, or mixed. Radiographic appearance of sunburst pattern is classic for osteosarcoma but is not a sensitive or specific feature. Garrigton et al. mentioned that the roentgenographic evidence of symmetrically widened periodontal membrane space was a significant early finding in jaw osteosarcoma. The extent of tumor in both bone and soft tissue can be best appreciated using computed tomography (CT) or magnetic resonance imaging which shows the formation of irregular endosteal and extracortical bone as well as destroyed or obliterated cortex [5]. To confirm the diagnosis, biopsy is needed. These neoplasms often show a typical clinical behavior and varied radiological appearances. They present wide spectrum of histopathological features. Commonly seen variants are osteoblastic, chondroblastic, and fibroblastic, of which chondroblastic variant predominates. Few other variants may show fibrohistiocytic differentiation, which may be mistaken for malignant fibrous histiocytoma. Some osteosarcomas histologically resemble osteoblastomas. Hence, it is necessary to differentiate between all these lesions as the treatment plan for all these lesions is different. Rarely, tumor may show a spectrum of histopathology. Here, a case report of a 21-year-old male patient is described which showed varied histomorphologic pattern causing a diagnostic dilemma.
Case Report
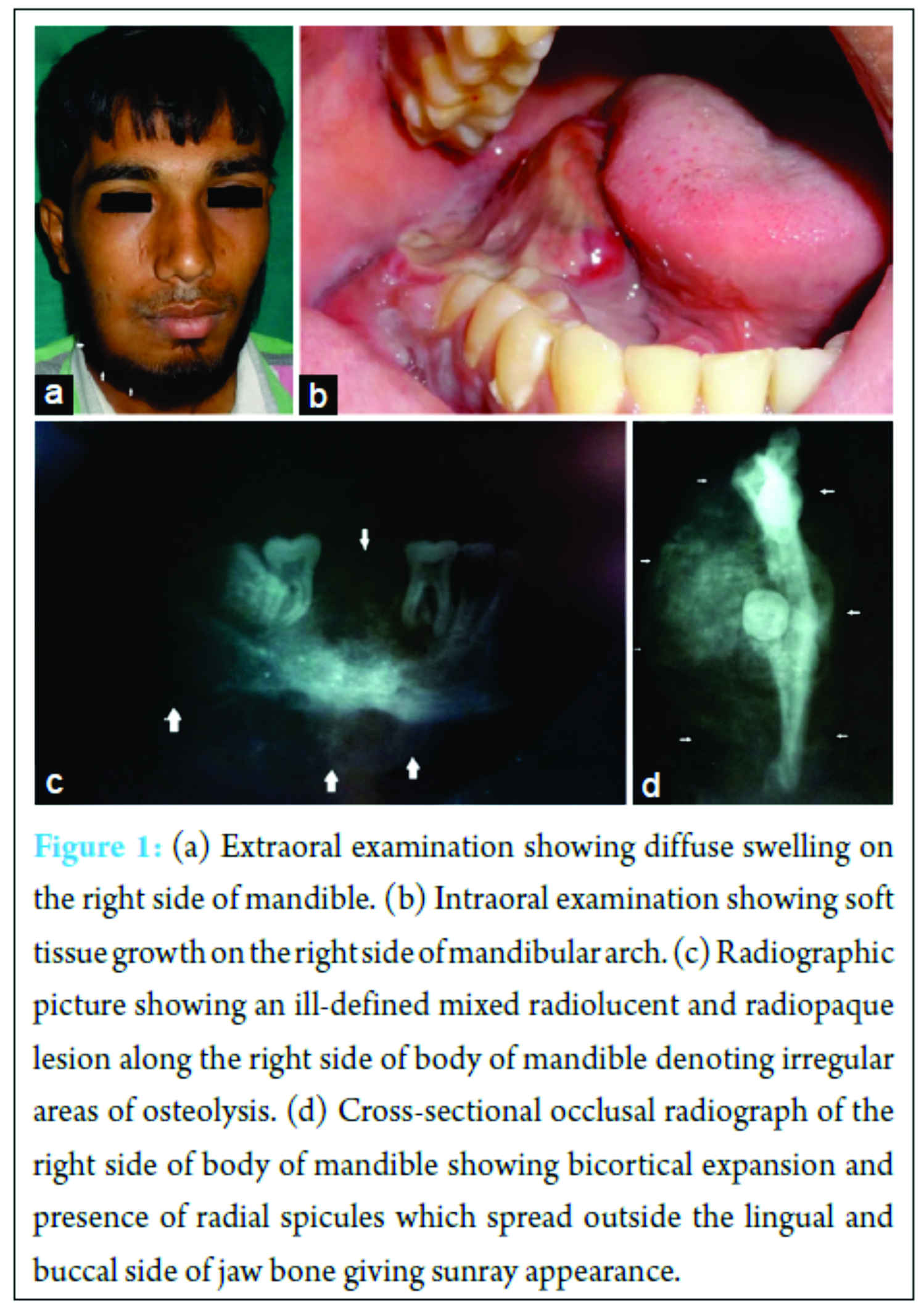
A 21-year-old male reported with a diffuse swelling and pain in the lower right posterior region of jaw for 4 months. Pain was dull and intermittent with increase in difficulty during eating and speech. The patient gave a history of extraction 1 month before for the same complaint, but there was no relief. After 2 months, growth appeared intraorally. Medical history was non-contributory. Extraoral examination revealed a diffuse swelling on the right side of mandible, extending anteroposteriorly from 1 cm behind angle of mouth to angle of mandible. Superoinferiorly, 2 cm below line drawn from angle of mouth to tragus of ear to 4 cm below lower border of mandible roughly measuring around 5 cm × 4 cm in size. Skin over swelling appeared normal on inspection and firm and tender on palpation. Right submandibular lymph node was palpable, enlarged, firm to hard, and fixed (Fig. 1a). Intraoral examination revealed a soft tissue growth along the right side of mandibular arch. It extended from first premolar to retromolar region causing obliteration of buccal and lingual vestibule. Overlying mucosa was red. Surface appeared smooth with areas of depression at places (Fig. 1b).
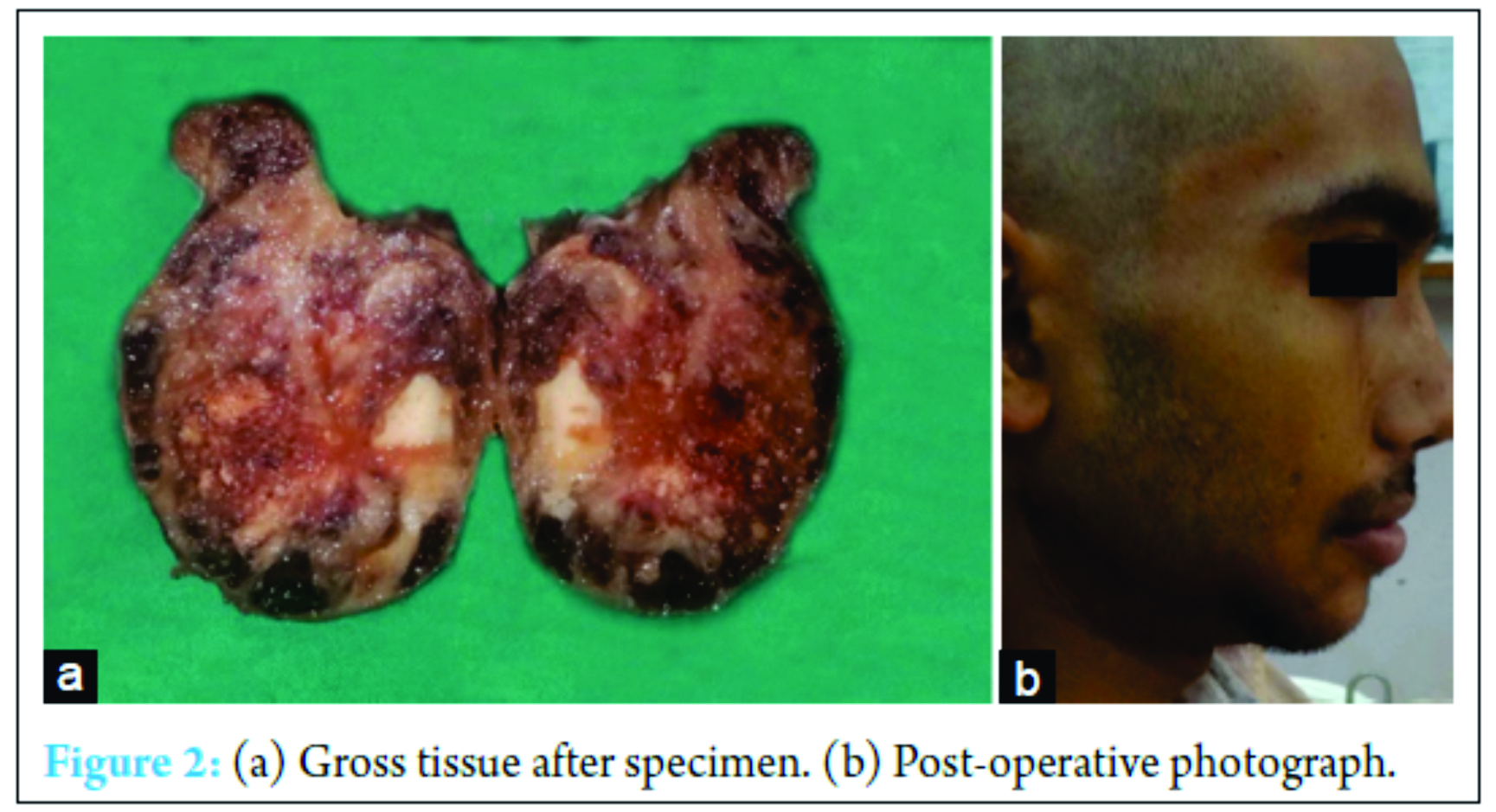
Radiographic evaluation included panoramic radiograph, occlusal radiograph, and cone beam CT. Panoramic radiograph revealed an ill-defined mixed radiolucent and radiopaque lesion along the right side of body of mandible denoting irregular areas of osteolysis (Fig. 1c). The cross-sectional occlusal radiograph of the right side of body of mandible showed bicortical expansion and presence of radial spicules which spread outside the lingual side of jaw bone giving sunray appearance (Fig. 1d). Aspiration was done which gave yellowish viscous blood tinged fluid. Based on clinical and radiological findings, the provisional diagnosis of malignancy of right side of the mandible, hemangioma, and osteosarcoma was given. The incisional biopsy revealed osteoid tissue with irregular trabeculae with osteoblasts which were large round to oval, epithelioid in appearance with hyperchromatic nucleus and prominent nucleoli and occasional atypical mitoses. Intertrabecular areas showed solid cellular stroma. As the biopsy was incisional, tumor border cannot be traced. Hence, the diagnosis was given as aggressive osteoblastoma/Osteoblastoma like osteosarcoma(Fig. 3b). Lesion was excised. Grossly, there was extensive soft tissue destruction with an associated soft tissue mass (Fig. 2a). The histopathology revealed abundance of osteoid and tumor bone without osteoblastic rimming suggestive of osteoblastic osteosarcoma (Fig. 3c). Other areas showed fibrous spindle cell areas where osteoid or tumor bone was scarce i.e. (fibroblastic/fibrohistiocytic type Fig. 3a). At focal places, vessels were numerous, dilated and proliferating giving a haemangiopericytomatous appearance (Fig. 3d) (Staghorn type appearance).
Discussion
Osteosarcoma arises from primitive bone forming mesenchymal cells and its histological hallmark is production of malignant osteoid tissue [5, 6, 7]. Other cell populations may also be present as these types of cells may also arise from pluripotent mesenchymal cells but any area of malignant bone in lesion establishes diagnosis as osteosarcoma [5]. There is no relationship between radiographic pattern and histological type of osteosarcoma [5]. Clinical characteristics of the case were in agreement with those of previous studies regarding age and chief clinical features. Histologically, osteosarcomas can be classified according to their cellular differentiation as osteoblastic, chondroblastic, and fibroblastic. In the osteoblastic type, atypical neoplastic osteoblast exhibits considerable variation in their shapes and sizes, showing large deeply staining nuclei which are arranged in a disorderly fashion. This type constitutes 60 % of the jaw lesions [2]. In the chondroblastic type, atypical chondroid areas composed of pleomorphic and atypical binucleate cells which had large hyperchromatic nuclei and prominent nucleoli are seen [2]. Fibroblastic type is rare [2]. The other histologic types include malignant fibrous histiocytoma-like osteosarcoma which shows spindle anaplastic cells [2, 8]. In large cell predominant osteosarcoma, large cells with prominent nucleoli are seen. Giant cell predominant osteosarcoma is characterized by anaplastic stromal cell producing streams of osteoid along with giant cells [2]. In small cell or round cell predominant type, osteoid producing small malignant cells and primitive bone tissue are the characteristic, whereas in telangiectatic osteosarcoma, anaplastic cells are present along with osteoid [2, 8]. Osteoblastoma-like osteosarcoma is also another type which is difficult to be differentiated from osteoblastoma [9-11]. Generally, one type of histologically predominant pattern is observed in osteosarcomas. This case revealed varied histologic pattern, i.e. osteoblastic, fibroblastic, hemangiopericytomatous, and osteoblastoma-like osteosarcoma varian,t but the presence of osteoid produced directly by the tumor cells clinched the diagnosis. No such case is reported in the literature with several histologic variants seen in one case of jaw osteosarcoma. As various histological variants are seen in the same patient representing the heterogeneity of the proliferating mesenchymal cells, the tumor may be more aggressive and with poor prognosis. Varying patterns may affect the aggressiveness and the prognosis of the lesion. Unlike long bone osteosarcomas, jaw osteosarcomas therapy of choice is radical surgical excision since it provides a 5-year survival rate of over 80%. Jaw osteosarcomas occur at higher mean ages; thus, the patients have less chances of developing metastases. Metastasis was rare and late occurring in only 18% of cases and local recurrence was still the leading cause of death. Generally, prognosis of jaw osteosarcomas is better than that of long bone osteosarcomas. This could be due to the histologically better differentiation of jaw osteosarcomas than that of long bone osteosarcomas. In the present case, the patient had a radical surgical resection of the right mandible along with margin of normal surrounding tissue, followed by radiotherapy. As various histological patterns are seen, the tumor may be more aggressive and with poor prognosis. Moreover, as the patients are younger, chances of developing metastasis may be present. Thus, proper follow-up of patient is required in such cases.
Conclusion
Osteosarcoma is an uncommon condition with an unusual presentation showing various histopathological patterns. This creates problems in correct diagnosis. Clinical appearance and radiology do not help in identification of the histopathological variant of osteosarcoma. Hence, histopathological examination of the fragments from all parts must always be done as the type of osteosarcoma may affect the treatment and the prognosis. In the present case, patient has no complaints to date (2 years post-surgically) (Fig. 2b). Follow-up intervals were every 6 weeks to 3 months in years 1 and 2; later, patient will be followed every 2-4 months in years 3 and 4, every 6 months in years 5-10, and every 6-12 months thereafter. Each visit will include a history and physical examination and a chest X-ray. X-rays of the primary tumor site are recommended every 4 months until the end of year 4. Late metastases may occur >10 years after diagnosis, and there is no universally accepted stopping point for tumor surveillance.
Clinical Message
Appropriate diagnosis of the variants of osteosarcoma and its differentiation from the other conditions is necessary as varying histologic patterns may affect the aggressiveness of the disease. This affects the treatment plan and thus the prognosis of the condition. Thus, the detailed knowledge of histology helps in suitable treatment and prognosis.
References
1. Kalburge JV, Sahuji SK, Kalburge V, Kini Y. Osteosarcoma of mandible. J Clin Diagn Res 2012;6(9):1597-1599.
2. Bojan A, Christy W, Chanmougananda S, Ashokan K. Osteosarcoma of mandible: A case report and review of literature. J Clin Diagn Res 2012;6(4):753-757. Available from: http://www.jcdr.net/articles/PDF/2182/58%20-%204207.pdf.
3. Nthumba PM. Osteosarcoma of the jaws: a review of literature and a case report on synchronous multicentric osteosarcomas. World J Surg Oncol 2012;10:240.
4. Vasudeo K. Chondroblastic osteosarcoma of jaw bone. J Case Rep 2013;3(2):480-484. Available from: http: //www.casereports.in/articles/3/ 2/Chondroblastic-Osteosarcoma-of-Jaw-Bone.html.
5. Khorate M, Goel S, Singh M, Ahmed J. Osteosarcoma of mandible: A case report and review of literature. J Cancer Sci Ther 2010;2(4):122-125.
6. Available from: http://www.omicsonline.org/osteosarcoma-of-mandible-a-case-report-and-review-of-literature-1948-5956.1000036.php?aid=220.
7. Yesilova E, Akgunlu F, Dolanmaz D, Yasar F, Sener S. Osteosarcoma: A case report. Eur J Dent 2007;1:60-63. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2612954.
8. Kumar NL, Rosenberg AE, Raskin KA. Osteoblastoma-like osteosarcoma of the cuboid: A case report. J Orthop Surg Res 2010;5:52.
9. Kumar H, Buch AC, Sawlani VM, Chandanwale SS. Diaphyseal osteosarcoma with varying histomorphologic patterns. Adv Biomed Res 2014;3:33.
10. Lucas D. Osteoblastoma. Arch Pathol Lab Med 2010;1460-1466. Available from: http://www.archivesofpathology.org/doi/10.1043/2010-0201-CR.1?url_ver=Z39.88-2003&rfr_id=ori: rid:crossref.org&rfr_dat=cr_pub%3dpubmed.
11. Bertoni F, Unni K, Mcleod R, Dahlin D. Osteosarcoma resembling osteoblastoma. Cancer 1985;55:416-55426. Available from: http://www.onlinelibrary.wiley.com/doi/10.1002/1097-0142 (19850115)55:2%3C416:AID-CNCR2820550221%3E3.0.CO;2-5/pdf.
| How to Cite This Article: Agrawal RR, Bhavthankar JD, Mandale MS, Patil PP. Osteosarcoma of Jaw with Varying Histomorphologic Patterns: Case Report. Journal of Orthopaedic Case Reports 2017 Jan-Feb;7(1):61-64. Available from: https://www.jocr.co.in/wp/wp-content/uploads/19.-2250-0685.690.pdf |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com