[box type=”bio”] What to Learn from this Article?[/box]
Ankle joint tuberculosis is a disorder that can be easily misdiagnosed.
Case Report | Volume 7 | Issue 1 | JOCR January – February 2017 | Page 87-90| Jeevan Pereira, S Anoop, George Joy Pettah. DOI: 10.13107/jocr.2250-0685.702
Authors: Jeevan Pereira[1], S Anoop[1], George Joy Pettah[1]
[1] Department of Orthopaedics, Yenepoya Medical College Hospital, Deralakatte, Mangalore, Karnataka, India.
Address of Correspondence
Dr. S. Anoop,
Department of Orthopaedics, Yenepoya Medical College Hospital, University Road, Deralakatte, Mangalore – 575 018, Karnataka,
India. Phone: +91-7204896925.
E-mail: anoopsuresh88@gmail.com
Abstract
Introduction: Tuberculosis (TB) of the ankle is an uncommon presentation of extrapulmonary infection. The early diagnosis of TB arthritis of the ankle is difficult because of the uncommon site, the ability of TB to mimic other disorders and, all too common, lack of awareness of about this infection in ankle joint.
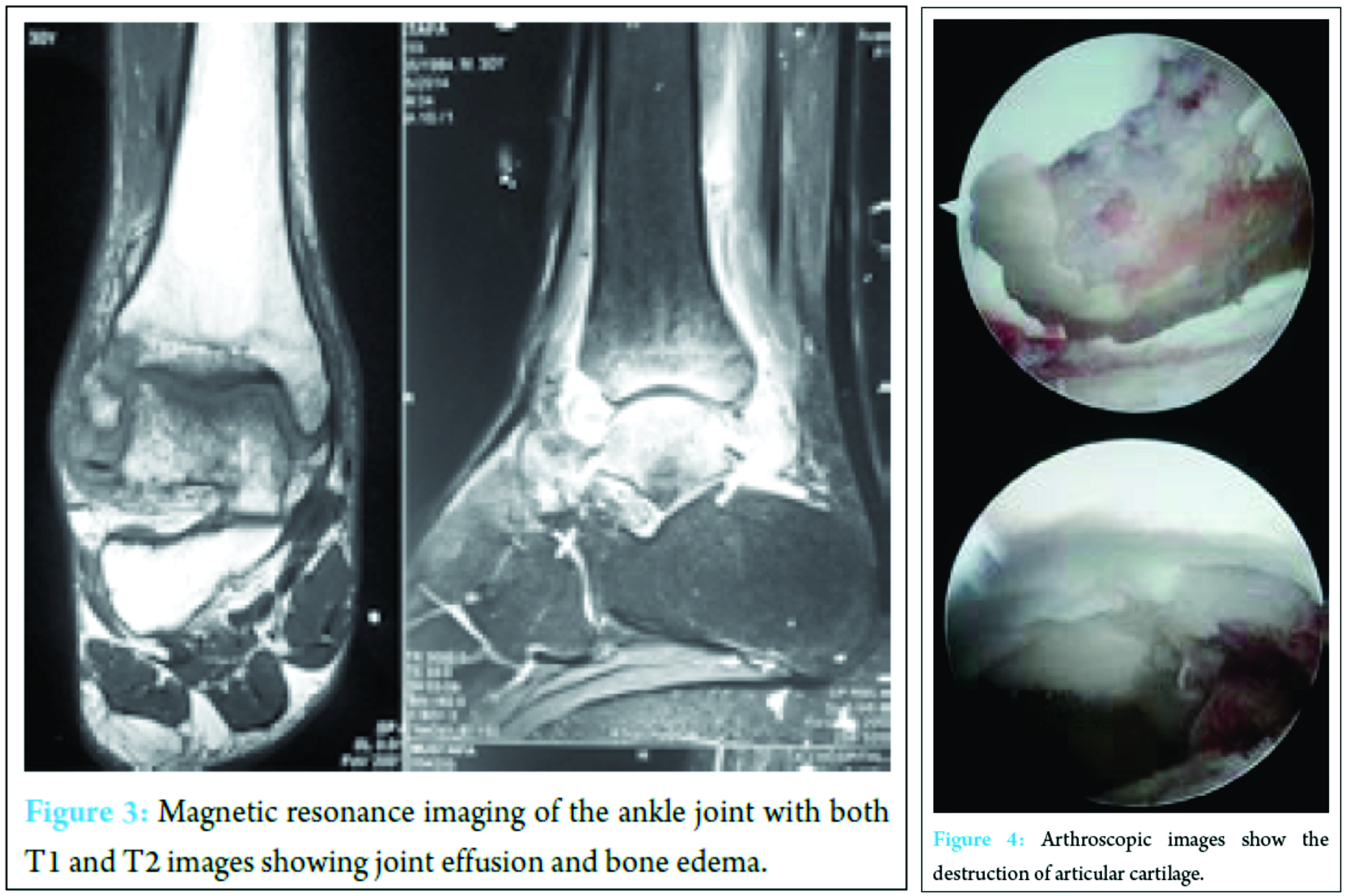
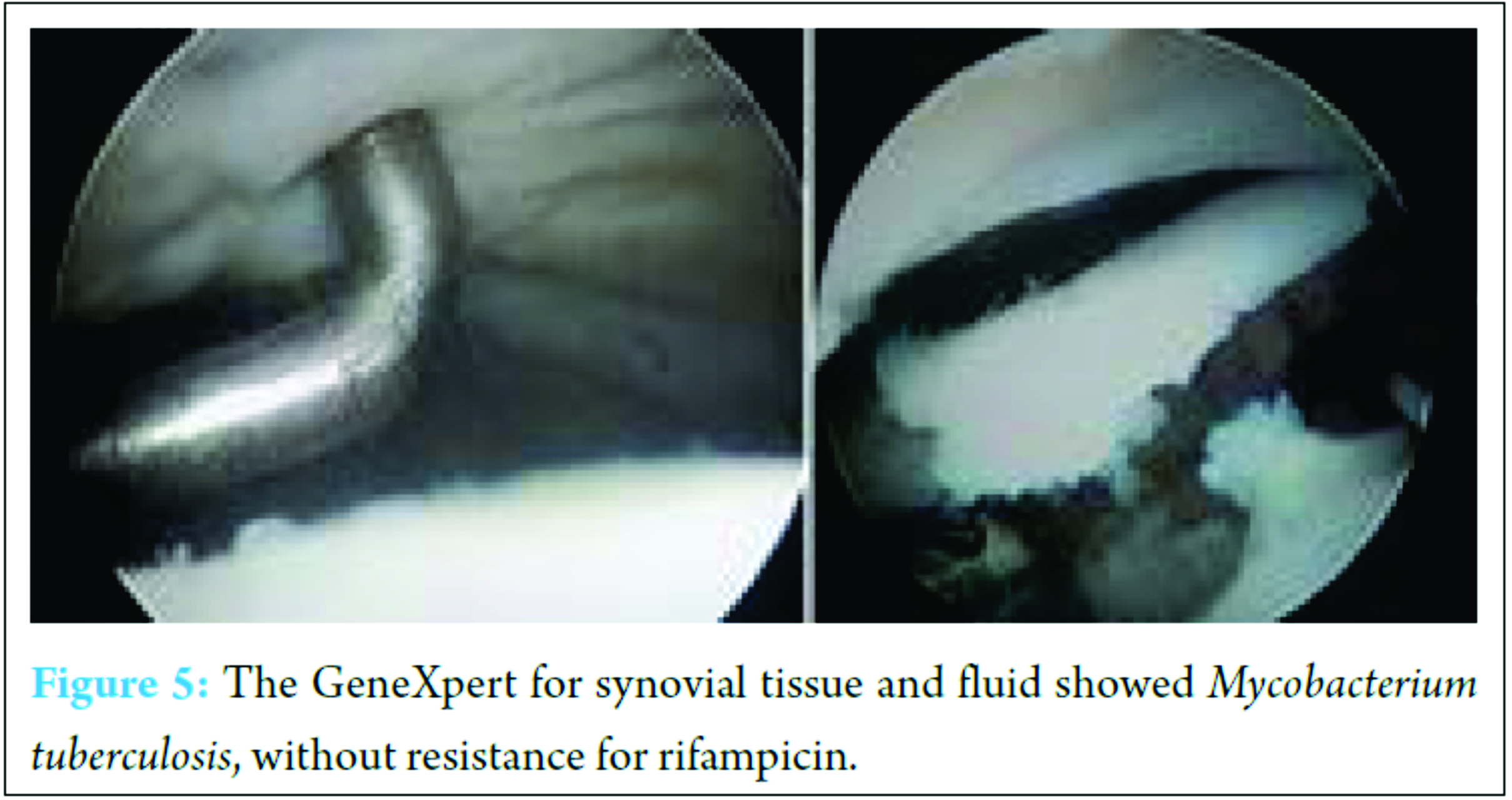
Case Report: A 30-year-old male presented with a 1-year history of right ankle pain and swelling. He denied any history of recent infection but had had recurrent ankle pain that had been treated accordingly. When he visited our outpatient clinic, he was afebrile. The patient, despite a period of conservative treatment, presented with a localized painful fullness of the ankle. Magnetic resonance imaging helps for the diagnosis with variable specificity, but TB arthritis was diagnosed through a diagnostic arthroscopic procedure, and anti-TB therapy eventually eradicated the infection.
Conclusion: It is highly recommended that early biopsy and synovial fluid for polymerase chain reaction GeneXpert be performed in suspicious cases to confirm and treat accordingly.
Keywords: Ankle joint, arthritis, tuberculosis, ankle arthroscopy.
Introduction
In India, pulmonary tuberculosis (TB) is the most common form of TB accounting for 75-90% of all types of TB. Extrapulmonary TB constitutes 10-25% of TB cases and accounts for more than 50% of all cases of TB in HIV+ patients [1]. In extrapulmonary of TB, involvement of musculoskeletal system was only 1-2% out of which major proportion of involvement was seen in the spine and weight bearing joints such as hip and knee [2]. The incidence of ankle and foot TB was found to be <5% of all osteoarticular TB and mimic a wide range of pathology; as a result, it will often misdiagnosed [3]. The microorganism usually spreads through the bloodstream to the synovium in TB arthritis. Monoarticular disease is the rule although polyarticular disease has also been reported [4]. The subsequent infection causes articular cartilage destruction, resulting in chronic joint morbidity. Ankle pain is a common presentation in the emergency department or outpatient clinic and is commonly associated with ankle swelling following trauma. Diagnosis of ankle pain is largely based on the clinical presentation. Because of repetitive ankle injury, the underlying problem may be overlooked by not only the patient himself but also by the doctor, which may result in the delayed diagnosis of the underlying disease. Here, we describe an uncommon case of TB arthritis involving the ankle joint.
Case Report
A 30-year-old male presented with a 1-year history of right ankle pain and swelling. He denied any history of recent infection but had had recurrent ankle pain that had been treated accordingly. When he visited our outpatient clinic, he was afebrile but had fullness of the right ankle when compared to the unaffected side (Fig. 1).There was no skin lesion, and the right ankle had almost a full range of motion except terminal restriction of dorsiflexion. Radiographs of the ankle showed apparently normal tibiotalar joint in comparison to the contralateral side (Fig. 2).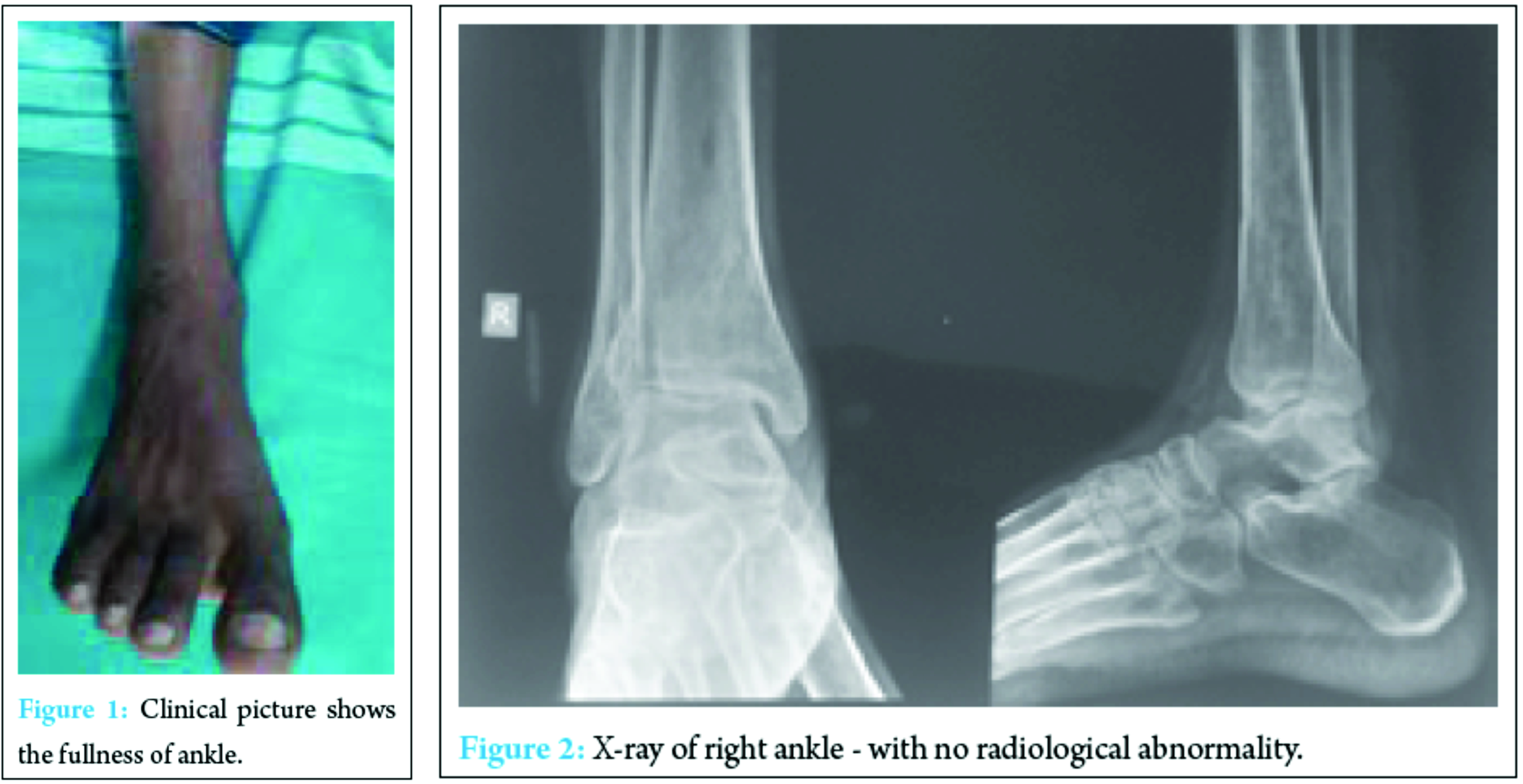
Discussion
TB still remains the most common infectious disease encountered in outdoor patient and has been a major cause of morbidity and disability. Osteoarticular TB represents 1-5% of all cases of TB disease and 10-18% of extrapulmonary involvement with the spine being the most commonly affected followed by major weight bearing joints. Four cases of ankle joint TB from Japan had similar clinical presentations as our patient [5]. Diagnosis of foot TB is difficult as it is detected in late stage. Most common symptoms include pain, swelling, and stiffness while swelling with fullness around malleoli and tendoachilis insertion, plantar flexion of ankle joint are the important signs of ankle-foot TB. There may be discharging sinus or nonhealing ulcer with secondary infection. Most commonly involved bones are calcaneum, talus, first metatarsal, and navicular. The midtarsal joint is the most commonly affected joint in this disease. Pulmonary involvement is uncommon and usually present in <50% of cases [6, 7]. X-ray is rarely diagnostic until late stage, computed tomography scan and MRI should be done on suspicion of ankle-foot TB as signs of bone destruction, and osteolysis can be seen but the diagnosis is confirmed only by histopathological examination of bone or soft tissue taken from the infected site [8]. Treatment is usually conservative with antitubercular treatment for 9-20 months with immobilization of affected joint by the cast. In our case, tubercular drugs were given for 12 months as recurrence is higher after shorter course [9, 10]. As results of conservative treatment are very good, surgical intervention (debridement and curettage, excision of sequestrated/destroyed bones and arthrodesis) is reserved only for failure of conservative therapy.
Conclusion
When a patient presents with a localized painful swelling of the ankle joint which increases on exertion, it should raise the suspicion for chronic inflammatory disease. In cases where TB is suspected, it is advisable for early biopsy and PCR-GeneXpert in addition to the routine investigation. TB of ankle is even rarer in comparison to foot; hence, simple PCR-GeneXpert will help in diagnosis and early treatment.
Clinical Message
Ankle TB is a disorder that can be easily misdiagnosed.
References
1. Tuli SM. Tuberculosis of the Skeletal System (Bones, Joints, Spine and Bursal Sheaths). 4th ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd.; 2010. p. 131-139.
2. Anand A, Sood LK. Isolated tuberculosis of talus without ankle and subtalar joint involvement. Med J Malaysia 2002;57(3):371-373.
3. World Health Organisation. Report on Global Tuberculosis Control. Geneva: World Health Organisation; 2008.
4. Linares LF, Valcarcel A, Mesa Del Castillo J, Saiz E, Bermudez A, Castellon P. Tuberculous arthritis with multiple joint involvement. J Rheumatol 1991;18(4):635-636.
5. Inoue S, Matsumoto S, Iwamatsu Y, Satomura M. Ankle tuberculosis: a report of four cases in a Japanese hospital. J Orthop Sci 2004;9(4):392-398.
6. Mariconda M, Cozzolino A, Attingenti P, Cozzolino F, Milano C. Osteoarticular tuberculosis in a developed country. J Infect 2007;54(4):375-380.
7. Hakimi M, Hashemi F, Mirzaie AZ, Pour AH, Kosari H. Tuberculous osteomyelitis of the long bones and joints. Indian J Pediatr 2008;75(5):505-508.
8. Shah BA, Splain S. Multifocal osteoarticular tuberculosis. Orthopedics 2005;28(3):329-332.
9. Dhillon MS, Aggarwal S, Prabhakar S, Bachhal V. Tuberculosis of the foot: An osteolytic variety. Indian J Orthop 2012;46(2):206-211.
| How to Cite This Article: Pereira J, Anoop S, Pettah GJ. A Case of Chronic Inflammation of the Ankle Joint with Subtle Signs of Inflammation: A Rare Presentation of Tuberculosis Ankle. Journal of Orthopaedic Case Reports 2017 Jan-Feb;7(1):87-90. Available from: https://www.jocr.co.in/wp/wp-content/uploads/25.-2250-0685.702.pdf |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com