[box type=”bio”] Learning Points for this Article: [/box]
A novel technique of articular reconstruction in periarticular Giant Cell Tumor using threaded K wires which is economical and widely available.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 68-71| Padmanabh H Vora, Rameez Musa, Neel M Bhavsar, Darshan Shah. DOI: 10.13107/jocr.2250-0685.858
Authors: Padmanabh H Vora[1], Rameez Musa[1], Neel M Bhavsar[1], Darshan Shah[1]
[1] Department of Orthopaedics, Smt. N.H.L. Municipal Medical College, Ahmedabad. India.
Address of Correspondence
Dr. Neel M Bhavsar,
Department of Orthopaedics,
Smt. N.H.L. Municipal Medical College & V.S. General Hospital, Kocharab, Ellisbridge, Paldi, Ahmedabad – 380006. India.
E-mail: drnmbortho@gmail.com
Abstract
Introduction: Giant Cell Tumor(GCT) is one of an infrequently encountered tumor by orthopaedic surgeons in clinical practice. It is described as ‘locally malignant’ tumor found in epimetaphyseal region of long bones, peculiarly around knee. We present a case of a solitary, benign Campanacci Grade 2 GCT in right lateral femoral condyle in 38 year old female and our treatment.
Case Report: A 38 year old female presented to our outpatient department with chief complaint of constant, moderate pain in right knee increasing in duration since 3 months. No history of precedent trauma. Radiological imaging with radiographs showed suspicious lytic lesion in lateral femoral condyle. MRI scan was done.On biopsy, histopathological evaluation showed presence of characteristic multinucleated giant-cells. After confirmation, tumor en bloc resection was done, followed by chemical cauterization with 5 % phenol. Articular margins were realigned under direct vision and fixed with 1.8 mm threaded K wires. PMMA cementing in bone defect was done after achieving adequate hemostasis. At two years follow-up, patient had good result in terms of pain, knee range of motion and weight bearing.
Conclusion: Combination treatment of radical curettage, phenol irrigation, electrocautery and cementation is effective in preventing local recurrence. This can replace en bloc resection with a wide margin. Using subchondral threaded Kirschner wires to maintain articular margins is cheap alternative to costly implants in economically underprivileged patients.
Keywords: Giant cell tumor, articular reconstruction, lateral femoral condyle tumor, PMMA Cementation.
Introduction
Giant Cell Tumor (GCT) is a relatively uncommon tumor. It was first described by Cooper and Travers in 1818 [ 1]. GCT was described in depth by Jaffe and Lichenstein, including its pathological appearance, grading, etiology and variants [2]. Although categorized into benign lesions, GCT are are locally aggressive and notorious for higher recurrence(about 50%) following simple curettage. However, currently recurrence rates have decreased to 10-15 % in most published series due to use of better techniques, adjuvants and increased understanding [3]. GCT comprises of 5 % of all neoplasms that occur in bone with slight female preponderance, mostly occurring in patients with closed physes i.e. age group 20-40 years [4, 21]. Radiologically, GCT is visualized in conventional radiographs as a well-defined lytic lesion with often nonsclerotic margin, eccentric in location, extending often to subchondral bone. Magnetic Resonance Imaging(MRI) is largely used to define extent of tumor in bone to plan resection and to visualise soft tissue envelope. Campanacci graded all primary and recurrent tumours based on their radiological appearance [21].
Grade – I tumor has a well-marginated border of a thin rim of mature bone, and the cortex is intact or slightly thinned but not deformed.
Grade – II tumor has relatively well defined margins but no radiopaque rim; the combined cortex and rim of reactive bone is rather thin and moderately expanded but still present.
Grade – III designates a tumor with fuzzy borders, suggesting a rapid and possibly permeative growth; the tumor bulges into the soft tissues, but the soft-tissue mass does not follow the contour of the bone and is not limited by an apparent shell of reactive bone.
Microscopically, GCT comprises of many multinucleated giant cells in a conglomeration of mononuclear stromal cells. Spindle cells, foamy macrophages and reactive bone formation is also seen alongwith stroma. Treatment of GCT revolves around adequate resection of lesion. This could be done either by intralesional curettage and adjuvant usage at the cost of having recurrence or by doing wide resection of lesion with use of prosthesis and allografts at the cost of having biological disintegration. Various studies have demonstrated promising results by usage of PMMA cementation for defect after curettage [6,15,16,17].
Case Report
A 38 year old female, housewife, came to our outpatient department with chief complaints of pain and swelling over right knee since 6 months. Pain was mild and activity related to start with and progressed to moderate and continuous. There was no history of precedent trauma, no history of fever, weight loss and anorexia. Patient had not solicited any treatment for this. On examination, there was diffuse bony swelling with crunchy ‘feel’ over right femoral condyles more localized to left side, extending to popliteal fossa. Overlying skin and muscles were free and mobile. Patient was unable to squat and walk painfree with knee ROM halted to 50 degree flexion but no fixed flexion deformity and full terminal extension possible.
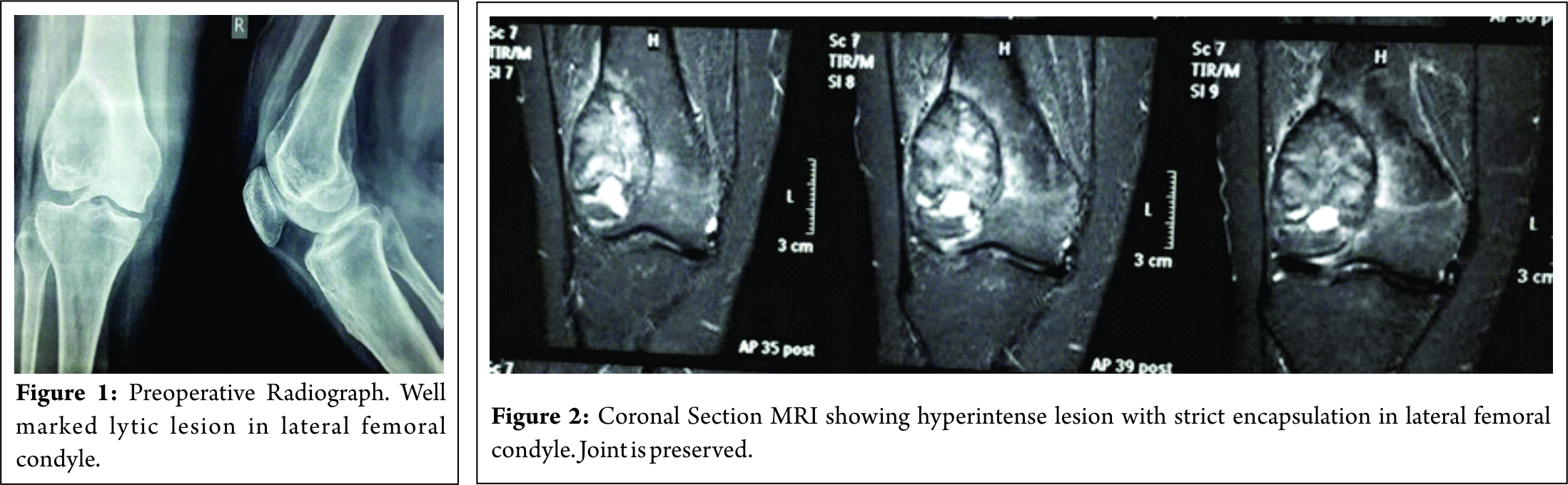
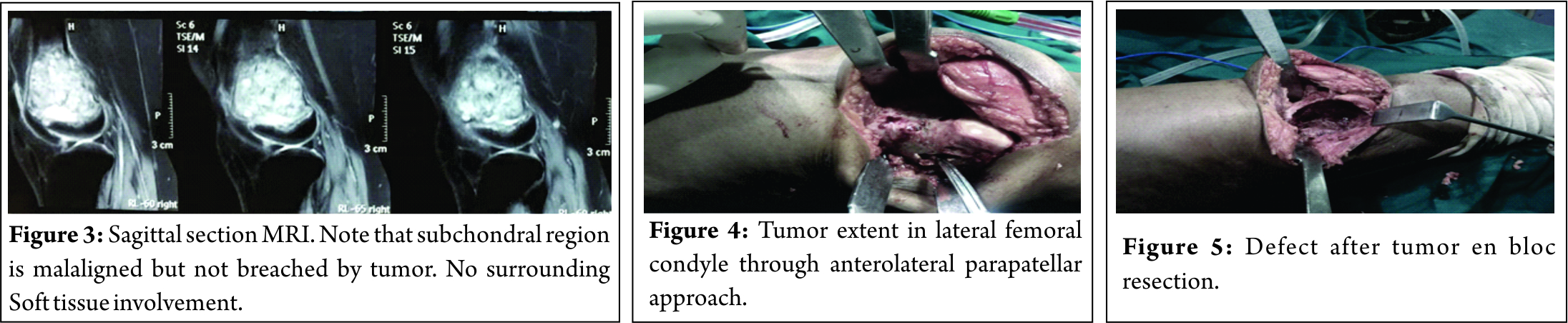
On plain radiographs, a distinct expansile radiolytic lesion was found in lateral femoral condyle, with articular step off , but no cortical breach on medial, lateral or posterior side, with thinned out nonsclerotic margin, graded as Campanacci Grade 2 (Fig. 3). MRI was done, which reaffirmed heterogeneous hyperintense lesion measuring 55×41 mm in epimetaphyseal region of lateral femoral condyle, with no soft tissue involvement(Fig. 1&2). A confirmatory biopsy was taken with all precautions for future procedure. Biopsy track was marked so as to include in approach during resection.
On confirmation of GCT in biopsy, a marginal resection and curettage with articular reconstruction and PMMA cementing for skeletal support was planned.
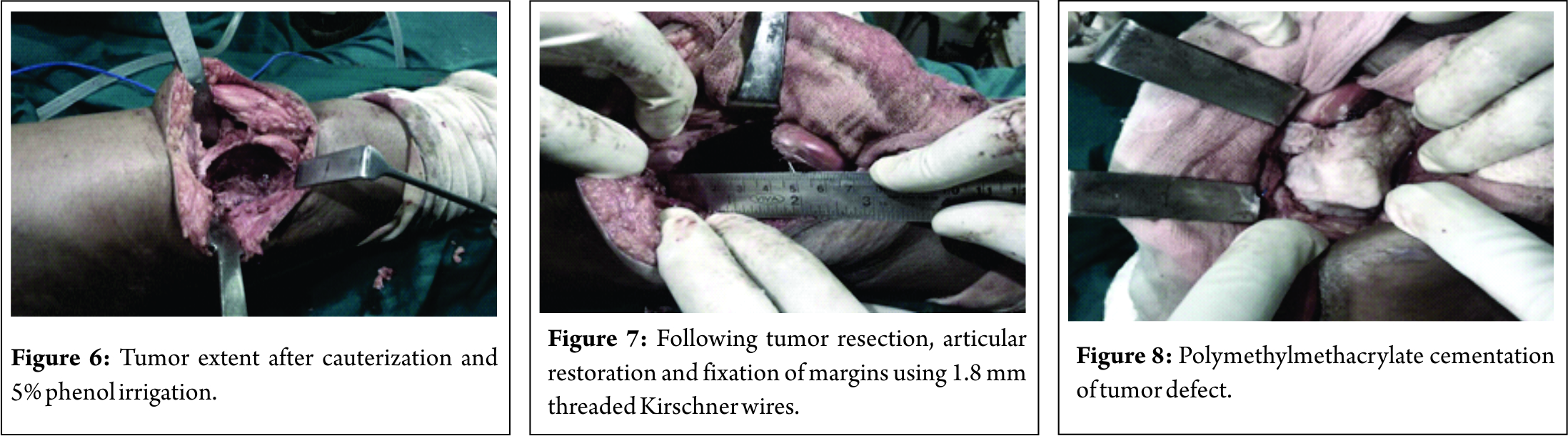
Under spinal anesthesia, with tourniquet, an anterolateral parapatellar approach was taken, with view of future need of knee arthroplasty. After adequate visualisation of tumor extent and articular margin, marking was done for wide resection (Fig. 5&6). Surgical mops were placed before opening the marrow, to avoid surrounding tissue contamination. Cortical breakout of lateral femoral wall occurred midway and curettage was done till the extent of viable bleeding bone. Cauterization of margins was carried out followed by denaturation of margins using 5 % Phenol soaked mop(Figure 6&7). Articular margin of lateral knee joint was reconstructed after elevation of subchondral bone and fixation using 1.8 mm threaded K wires (Fig. 8).
Bone defect was again curetted and prepared for cementing. PMMA cement, dual dose, was prepared using vacuum mixing technique, and the bone defect was filled with PMMA cement(Fig. 9). Threaded K wires were cut short, with ends for future retrieval. Closure was done in layers after tourniquet release and adequate hemostasis control.
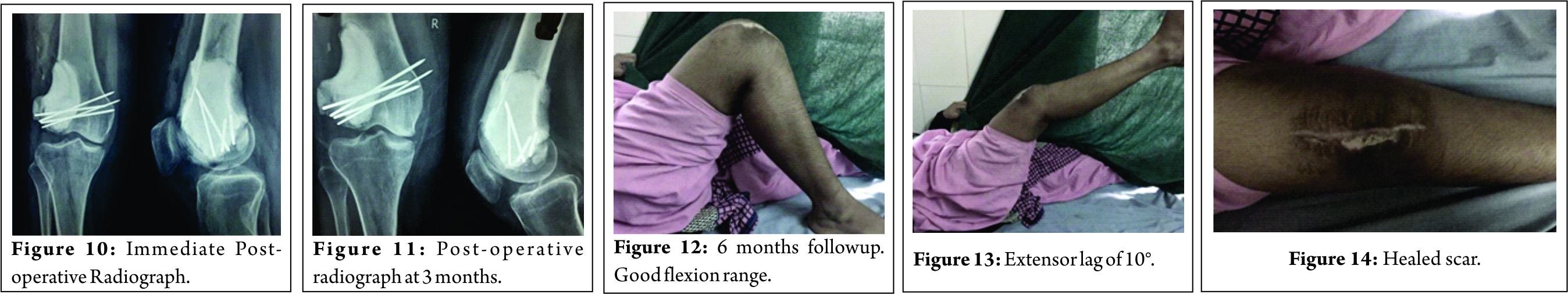
Patient was advised immediate ROM exercises on postoperative day 1 and allowed Full weight bearing with support. Patient could gain 90 degree flexion of knee with 10 degree terminal extension lag and Straight leg Raise possible (Fig. 10-13).
After 3 months, Postoperative radiology was done to see status of distal femur(Fig. 14). Chest xrays were taken every 3 months. Patient was followed for 2 years and has shown no signs of recurrence, cement subsidence or K wire loosening (Figure 15-17).
Discussion
Giant cell tumors involving lateral femoral condyle have been treated variedly by different proponents. Most of proponents now agree on not violating articular cartilage of lateral femoral condyle. There are high chances of pathological fracture as this is a major weight bearing area. Available methods for providing mechanical support after adequate curettage are :
Use of bone allograft[5].
Methylmethacrylate cementation[6].
Tumor endoprosthesis[7].
Intercalary reconstruction using vascularized fibula graft [8].
Resection arthrodesis using intramedullary nail [9].
D’aubigne procedure of pedicled patellar transplantation [10].
Osteoarticular allografts and tumor endoprosthesis are in vogue for large defect after resection of tumor. Although providing a good functional outcome and less recurrence with modern techniques, these modalities do face higher cost, wound complications, infection and non-union rates requiring revision [5,7]. In our country, with limited resources and at times cost inhibition, this modalities seem out-of-reach for quite a number of patients, although they are treated in tertiary center. Resection arthrodesis over dual grafts or intramedullary nail offers excellent outcome in terms of lower recurrence rates and stable/painless knee. However, with this there is definite compromise over daily activities and disability due to knee arthrodesis [9, 11]. Radical resection as compared to intralesional curettage offers very low recurrence rate but at cost of greater bone loss and associated morbidity [11]. Both intercalary reconstruction using vascularized graft and D’aubigne procedure are technically difficult procedures which have offered variable results in different case series [8, 10, 12, 13].
Methylmethacrylate cementation.
The method of cementation using acrylic cement in post-tumor resection defect was first described in 1969 by Vidal et al in their French article [14].
Advantages offered by cementation include
Immediate stability [15].
Lower morbidity as compared to other modalities[15].
Heat penetration upto 3 mm of tumor margin and tumor lytic properties[16].
Mixture with methotrexate can provide augmented tumorolysis[6, 17].
Easier detection of recurrence compared to bone grafting by absence of sclerotic rim at bone-cement interface [18].
Major disadvantage of cementation is of local recurrence. Various studies implicate local recurrence rate ranging from 0.5% to 29% [15, 19, 20].
We describe here a novel approach of using threaded K wires to hold subchondral and articular reconstruction before cementation of bone defect. Curettage followed by meticulous adjuvant treatment can preserve joint function and prevent associated morbidities. When there is no local recurrence(> 2 years) then cement could be replaced by bone grafting. Threaded K wires(1.8 mm) offer good purchase in subchondral bone and maintain the articular scaffold against collapse under weight bearing. A long term follow-up is necessary to provide definite judgment.
Conclusion
Combination treatment of radical curettage, phenol irrigation, electrocautery and cementation is effective in preventing local recurrence. This can replace en bloc resection with a wide margin. Using subchondral threaded K wires to maintain articular margins is cheap alternative to costly implants in economically underprivileged patients.
Clinicla Message
Over the years, the management-associated challenges for GCT have intrigued surgeons to formulate an affordable and effective solution. With a patient-oriented approach, the ultimate aim of this strife should be to attain a balance between optimum resection and preservation of biology in constant alignment with the patient’s well-being.
References
1. Cooper AS, Travers B. Surgical essays. London, England: Cox Longman & Co, 1818; 178–179.1. Cooper AS, Travers B. Surgical essays. London, England: Cox Longman & Co, 1818; 178–179.
2. Jaffe HL, Lichtenstein L, Portis RB. Giant cell tumor of the bone: Its pathological appearance, grading, supposed variant and treatment. Arch Pathol. 1940;30:993–1031.
3. Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Giant cell tumor of bone: risk factors for recurrence. Clin Orthop Relat Res. 2011;469(2):591-9.
4. Hoch B, Inwards C, Sundaram M, Rosenberg AE. Multicentric giant cell tumor of bone. Clinicopathologic analysis of thirty cases. J Bone Joint Surg Am. 2006;88(9):1998-2008.
5. Bianchi G, Staals EL, Donati D, Mercuri M. The use of unicondylar osteoarticular allografts in reconstructions around the knee. Knee. 2009;16(1):1-5.
6. Moon, M. S., Kim, S. S., Moon, J. L., Kim, S. S., & Moon, H. (2013). Treating giant cell tumours with curettage, electrocautery, burring, phenol irrigation, and cementation. Journal of Orthopaedic Surgery, 21(2), 209-212.
7. Natarajan MV, Prabhakar R, Mohamed SM, Shashidhar R. Management of juxta articular giant cell tumors around the knee by custom mega prosthetic arthroplasty. Indian J Orthop. 2007;41(2):134-8.
8. Muramatsu, K., Ihara, K., Shigetomi, M., & Kawai, S. (2004). Femoral reconstruction by single, folded or double free vascularised fibular grafts. British journal of plastic surgery, 57(6), 550-555.
9. Enneking, W. F., & Shirley, P. D. (1977). Resection-arthrodesis for malignant and potentially malignant lesions about the knee using an intramedullary rod and local bone grafts. J Bone Joint Surg Am, 59(2), 223-236.
10. R. Merle D’aubigne (1973) Reconstruction of the Knee by Pedicled Patellar Transplant, Acta Orthopaedica Scandinavica, 44:4-5, 550-559.
11. Campanacci, M., & Costa, P. (1979). Total resection of distal femur or proximal tibia for bone tumours. Autogenous bone grafts and arthrodesis in twenty-six cases. Bone & Joint Journal, 61(4), 455-463.
12. Hsu, R. W., Wood, M. B., Sim, F. H., & Chao, E. Y. (1997). Free vascularised fibular grafting for reconstruction after tumour resection. J Bone Joint Surg Br, 79(1), 36-42.
13. Ceruso, M., Falcone, C., Innocenti, M., Delcroix, L., Capanna, R., & Manfrini, M. (2001). Skeletal reconstruction with a free vascularized fibula graft associated to bone allograft after resection of malignant bone tumor of limbs. Handchirurgie· Mikrochirurgie· Plastische Chirurgie, 33(04), 277-282.
14. Vidal J, Mimran R, Allieu Y, Jamme M, Goalard G. Plastie de comblement par metacrylate de methyl traitement de certaines tumeurs osseuses benigenes. Montepellier chir 1969;15:389-97.
15. Saikia KC, Bhattacharyya TD, Bhuyan SK, Bordoloi B, Durgia B, Ahmed F. Local recurrences after curettage and cementing in long bone giant cell tumor. Indian J Orthop. 2011;45(2):168-73.
16. Nelson DA, Barker ME, Hamlin BH. Thermal effects of acrylic bone cementation at tumor bone sites. Int J Hyperther 1997;13:287-306.
17. Wang HC, Chien SH, Lin GT. Management of grade III giant cell tumors of bones. J Surg Oncol 2005;92:46–51.
18. Remedios D, Saifuddin A, Pringle G. Radiological and clinical recurrence of GCT of bone after the use of cement. J Bone Joint Surg 1997;79:630-2.
19. Peterson BM, Ryldholm A, Berlin O, Gunterberg B. Curettage and acrylic cementation in surgical treatment of giant cell bone tumours. In: Enneking WF, editor. limb salvage in musculoskeletal oncology. New York: Churchill livingstone; 1987. p. 476.
20. Gitelis S. Mallin BA, Paisecki P, TurnerF. Intralesional Excision compared with en bloc resection for giant cell tumours of bone. J Bone Joint Surg 1993;75:1648-55.
21. Sobti A, Agrawal P, Agarwala S, Agarwal M. Giant Cell Tumor of Bone – An Overview. Archives of Bone and Joint Surgery. 2016;4(1):2-9.
 |
 |
 |
 |
| Dr. Padmanabh H Vora | Dr. Rameez Musa | Dr. Neel M Bhavsar | Dr. Darshan Shah |
| How to Cite This Article: Vora1 P H, Musa R, Bhavsar N M, Shah D. Articular Reconstruction using Subchondral Cementation and Threaded K wires in Giant Cell Tumor : A Novel Technique. Journal of Orthopaedic Case Reports 2017 Jul-Aug;7(4):68-71 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com