[box type=”bio”] Learning Points for this Article [/box]
Compression screw fixation has been the workhorse implant for medial malleolar nonunions; however, tension band wiring may be a better technique for such nonunions, as seen in this rare case of isolated, medial malleolus gap nonunion.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 72-75| Rakesh John, Mandeep Singh Dhillon, Ankit Khurana, Sameer Aggarwal, Prasoon Kumar. DOI: 10.13107/jocr.2250-0685.860
Authors: Rakesh John[1], Mandeep Singh Dhillon[1], Ankit Khurana[2], Sameer Aggarwal[1], Prasoon Kumar[1]
[1] Department of Orthopedics, Post Graduate Institute of Medical Education & Research (PGIMER), Sector 12,Chandigarh. India 160012.
[2] Department of Orthopaedics, All India Institute of Medical Sciences (AIIMS), Ansari Nagar, New Delhi. India.
Address of Correspondence
Professor. Mandeep Singh Dhillon,
Department of Orthopedics, Post Graduate Institute of Medical Education & Research (PGIMER), Sector 12, Chandigarh, India 160012.
E-mail: drdhillon@gmail.com
Abstract
Introduction: Isolated, neglected medial malleolus nonunion cases are a rare entity in orthopedic literature. All studies (except one) have described the use of compression screws (with or without plates) for medial malleolar nonunion management. In acute fractures, tension band wiring (TBW) has shown excellent results both in biomechanical and in clinical studies. On the contrary, it has seldom been used in nonunion or in neglected cases.
Case Report: We describe a 6-month-old neglected medial malleolus gap nonunion case who presented with progressive pain and limp. TBW with a monoblock, inlay, tricortical, and iliac crest bone graft for the defect was performed. The fracture united within 12 weeks and patient went back to his normal work routine; on the latest follow-up at 3 years, the patient was asymptomatic with no clinicoradiologic signs of secondary osteoarthritis of the ankle joint.
Conclusion: TBW may be better than screw fixation in the management of medial malleolus nonunion as it is technically straightforward and cost-effective, can provide equal or more compression than a screw; it does not damage the sandwiched inlay bone graft, and the amount of compression is surgeon-controlled. It is also more suitable for fractures with small distal fragments and/or osteoporosis.
Keywords: Nonunion, medial malleolus, tension band wiring, neglected.
Introduction
A fracture of the medial malleolus seldom fails to unite; nonunion is rare, but disabling complication encountered with bimalleolar ankle fractures, and little in the literature dictates principles of management [1, 2]. After encountering one such case, we reviewed the literature for isolated medial malleolus nonunion epidemiology and treatment methods. The literature review revealed that open reduction, internal fixation (ORIF) with self-tapping, compression screws with adjuvant bone graft is the preferred method of surgical fixation [3]. We describe a modification of the standard protocol, where we used tension band wiring (TBW) with a monoblock, inlay graft and achieved a satisfactory clinical outcome.
Case Report
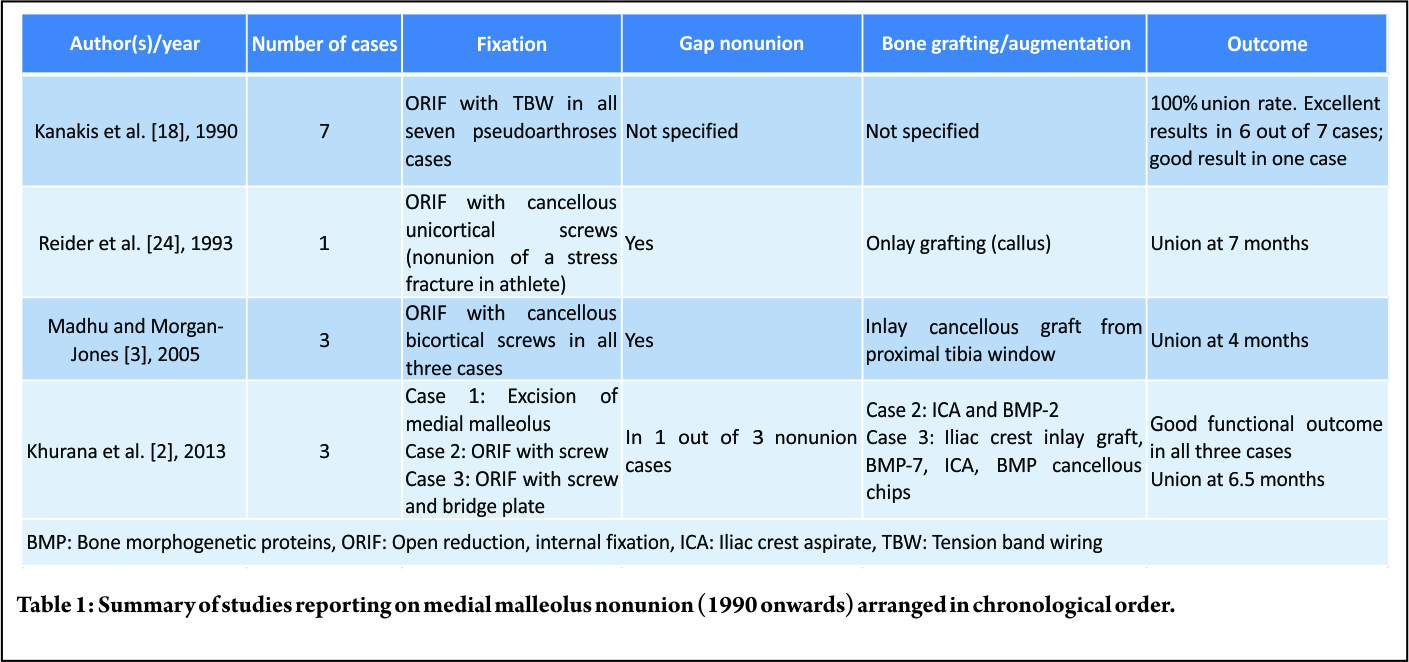
A 28-year-old male, manual laborer by occupation, presented to us with complaints of gradually progressive pain in the right ankle, on standing and walking, over the medial malleolar region with an associated antalgic gait. 6 months previously, he was involved in a road traffic accident when he was struck from behind by a bike while walking on the roadside. Following the impact, his right ankle struck the pavement with direct impact to the medial malleolus; the patient developed pain and swelling in the right ankle for which he consulted a quack in his locality who prescribed him rest and some home remedies and made him walk after 10 days. Initially the patient neglected the pain and carried on his activities; however, the pain had become unbearable in the previous 2 weeks, and the patient was unable to walk without the help of a cane. His ankle range of motion (ROM) was significantly decreased compared to the uninjured limb (0-0-30 vs. 15-0-45). Radiographs and computed tomography scans at presentation revealed an atrophic, gap nonunion of the medial malleolus without any associated lateral injury (Fig. 1a and b). The fracture pattern was most probably a pronation-abduction or pronation-external rotation type of injury (both Stage 1) according to the Lauge-Hansen classification. The patient was non-diabetic, non-smoker, was not on any long-term medications and did not suffer from any chronic disease.
Surgical Technique
We modified the treatment method keeping in mind the need for defect reconstruction as well as the small size of the displaced fragment. The medial malleolus was exposed through the standard medial approach; the nonunion site was freshened and adequately debrided. A significant defect was noted after freshening which was filled with a monoblock, tricortical iliac crest graft (inlay grafting); the fracture was reduced using a small Weber’s reduction clamp, and it was checked that the graft was not protruding into the joint clinically and radiologically. Two parallel 2-mm Kirschner wires were passed across the fracture site through the tricortical iliac crest block for provisional fixation; TBW with an 18 French stainless steel wire was performed using the standard technique (Fig. 2a and b).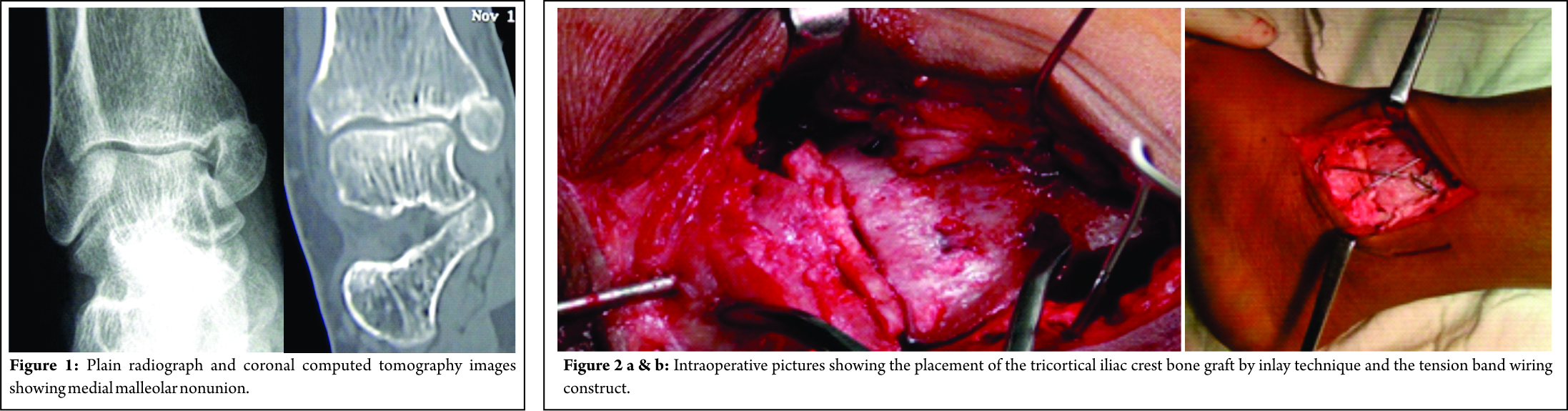
Discussion
Nonunion of bimalleolar ankle fractures was not uncommon in the earlier days when these fractures used to be managed nonoperatively; historically, the incidence ranged between 5% and 30% [4, 5, 6, 7]. Mendelsohn [7] reported a 4.3% incidence of nonunion in his case series of 253 ankle fractures (12/257 cases). Among the 12 nonunion cases in his series, he noted only two cases of isolated medial malleolus nonunions, which were eventually managed nonoperatively, as there was no significant tibiotalar displacement and the patients were relatively asymptomatic [7].
After the advent of the arbeitsgemeinschaft fur osteosynthesefragen (AO) philosophy and the increased indications of ORIF in bimalleolar fractures, the incidence of nonunion of bimalleolar ankle fractures has reduced significantly; most authors state that nonunion is currently a rare complication of bimalleolar ankle fractures [1, 2, 8, 9]. Rotational bimalleolar ankle fractures (supination-external rotation Type IV) are more prone for nonunion, especially when treated by nonoperative methods [10]. Local and systemic reasons which predispose a fracture to nonunion are generally well understood. Systemic factors include diabetes mellitus, smoking, alcohol use, obesity, advanced age, and radiation therapy [1, 2, 9]. Fracture-specific causes are excessive motion at the fracture site, compromised vascularity, diastasis at fracture site, and infection [11]. Some specific reasons for medial malleolus nonunion which has been described in the literature include soft tissue interposition (especially by the tendon of the tibialis posterior or deltoid ligament), paltry vascular supply to the fractured fragment, inadequate reduction/fixation, poor osteogenic activity, and the effect of synovial fluid on the fracture hematoma [12, 13, 14]. Not all medial malleolus nonunion necessitate surgical fixation. Stable, fibrous nonunions without any tibiotalar displacement can still be treated nonoperatively [4, 5, 6, 7, 14]. Indications for surgical fixation of medial malleolus nonunion include significant pain and a consequential antalgic gait, tibialis posterior tenosynovitis, and/or ankle instability [4]. Not all medial malleolus nonunion necessitate surgical fixation. Stable, fibrous nonunions without any tibiotalar displacement can still be treated nonoperatively [4, 5, 6, 7, 14]. Indications for surgical fixation of medial malleolus nonunion include significant pain and a consequential antalgic gait, tibialis posterior tenosynovitis, and/or ankle instability [4]. For atrophic type of nonunions some form of osteogenic stimulation in the form of bone graft or other adjuncts like bone morphogenetic proteins (BMPs), is necessary apart from anatomic reduction and rigid, stable fixation [3, 15, 16]. Screw fixation is the most commonly employed technique to fix symptomatic medial malleolar nonunion. Khurana et al. [2] reported three cases of medial malleolus nonunion in their mixed cohort study of 15 bimalleolar nonunions (two of these cases were treated nonoperatively in the acute stage, and the other case went into nonunion after ORIF). Their study sought to evaluate the outcomes following operative treatment of bimalleolar fracture nonunions. One patient underwent ORIF with screw and augmentation by BMP-2 and iliac crest aspirate (ICA). In the second patient, a plate was used along with screws and augmentation with iliac crest bone graft, ICA, BMP-7 and BMP cancellous chips (a plate was used in this case to bridge the gap between fracture ends). In the third subject, the medial malleolar fragment was excised (reason not specified). They reported union in both cases which underwent ORIF and good functional outcomes in all three nonunion cases [2]. Madhu and Morgan-Jones [3] reported a modified screw fixation technique for medial malleolus nonunion in their case series of three bimalleolar nonunions (out of which two were initially treated by ORIF, and one patient was treated nonoperatively); the modification proposed was use of a cancellous screw with bicortical purchase of tibia instead of unicortical purchase. The defect in the medial malleolus nonunion site was bridged using cancellous bone graft obtained from a distal metaphyseal tibial window proximal to the nonunion site. They proposed that anatomical reduction, stable internal fixation and compression at fracture site with bone grafting was the ideal treatment for atrophic type of medial malleolus nonunion; they favored the use of self-tapping, cancellous screws as the ideal implant to provide compression at the fracture site [3]. Historically, TBW has been recommended by the AO/ASIF group for avulsion fractures of the medial malleolus with a distal fragment too small for screw fixation, or for osteoporotic bones where screw purchase is doubtful [17]. They also noted that TBW may need considerable exposure for implant removal if needed [17]. However, it has increasingly been recognized that TBW can be used for fractures with large fragments too, with excellent union rates and good functional outcomes [18].
Several biomechanical and clinical studies have proven that TBW provides a stronger construct than screw fixation constructs [19, 20, 21]. Ostrum and Litsky [19] conducted a clinical, prospective study of 31 medial malleolar fractures fixed by TBW along with an ex vivo biomechanical, cadaveric study on 6 fresh cadaver legs comparing the strengths of TBW and screw fixation constructs. They observed that the TBW construct was 4 times stiffer than a screw construct against pronation forces (P < 0.05); additionally, screw fixation produced a maximum of 35% return of intact tibial stiffness whereas TBW equaled or exceeded the intact tibial stiffness values (range: 22-141%). This demonstrated that a TBW construct provides greater compression (which is surgeon-controlled) than a screw construct. In the clinical part of the study, they observed a 100% union rate and good functional outcomes, with only two patients undergoing implant removal for hardware prominence [19]. Johnson and Fallat [20] conducted a comparative cadaveric study comparing biomechanical strengths of TBW and screw constructs. They observed that cancellous screws demonstrated only 47.16% of the strength of a TBW construct at clinical failure. The authors have recommended TBW as the method of choice for all medial malleolus avulsion fractures due to its superior strength [20]. Kanakis et al. [18] treated seven cases of medial malleolus nonunion by TBW in a case series of 104 medial malleolar fractures (all treated by ORIF with TBW). All seven pseudoarthroses united and patients returned to their work within 3 months of surgery. On long-term follow-up (mean 3.5 years), 6 of the 7 patients were classified as having “excellent” results on objective clinical assessment; the remaining one patient had a “good” result as some medial diastasis was observed in the ankle joint. It has not been specified if the authors noted any gap/defect at the pseudoarthroses site or whether bone graft/adjuncts were used. The authors have recommended TBW as the best technique for medial malleolus nonunion irrespective of the size of the malleolar fragment [18]. Apart from the biomechanical advantages listed above, TBW also provides flexibility; it is a technically straightforward method and is cost-effective, especially in the underdeveloped countries [18, 19, 22, 23].
Conclusion
Isolated medial malleolus nonunion is a rare entity in foot and ankle surgery; TBW, as shown in the current case, can be an effective treatment modality. The rarity of the problem, as evidenced by the limited literature, does not permit any evidence-based recommendation. However, points in favor of this procedure are ease of use, controlled compression, no damage to the sandwiched inlay bone graft, better suitability for fractures with small distal fragments and osteoporotic fractures.
Clinical Message
Tension band wiring may be better than screw fixation in the management of medial malleolus nonunion as it is technically straightforward, cost-effective, can provide equal or more surgeon controlled compression than a screw; it does not damage the sandwiched inlay bone grafting. It is especially suitable for fractures with small distal fragments and/or osteoporosis.
References
1. Capogna BM, Egol KA. Treatment of nonunions after malleolar fractures. Foot Ankle Clin 2016;21:49-62.1. Capogna BM, Egol KA. Treatment of nonunions after malleolar fractures. Foot Ankle Clin 2016;21:49-62.
2. Khurana S, Karia R, Egol KA. Operative treatment of non-union following distal fibula and medial malleolar ankle fractures. Foot Ankle Int 2013;34(3):365-371.
3. Madhu T, Morgan-Jones R. A modified operative technique for enhanced compression of medial malleolar non-union. Injury Extra 2005;36:520-525.
4. Banks SW. The treatment of non-union of fractures of the medial malleolus. J Bone Joint Surg Am 1949;31A(3):658-662.
5. Laurent LE. Pseudarthrosis of the internal malleolus. Ann Chir Gynaecol Fenn 1956;45(1):48-55.
6. Mindell ER, Rogers WJ 3rd. Refracture of ununited medial malleolus. Clin Orthop 1958;11:233-236.
7. Mendelsohn HA. Nonunion of malleolar fractures of the ankle. Clin Orthop Relat Res 1965;42:103-118.
8. Walsh EF, DiGiovanni C. Fibular nonunion after closed rotational ankle fracture. Foot Ankle Int 2004;25(7):488-495.
9. Dodson NB, Ross AJ, Mendicino RW, Catanzariti AR. Factors affecting healing of ankle fractures. J Foot Ankle Surg 2013;52(1):2-5.
10. Donken CC, van Laarhoven CJ, Edwards MJ, Verhofstad MH. Misdiagnosis of OTA Type B (Weber B) ankle fractures leading to nonunion. J Foot Ankle Surg 2011;50(4):430-433.
11. Weber BG, Cech O. Pseudarthrosis: Pathophysiology, Biomechanics, Therapy and Results. New York: Grune and Stratton; 1980.
12. Muller GM. Fractures of internal malleolus. Br Med J 1945;2(4418):320.
13. Watson-Jones SR. Fractures and Joint Injuries. 4th ed., Vol. 2. Baltimore: William and Wilkins; 1957.
14. Kristensen B. A report on results of treatment A.M. Lauge-Hansen of malleolar fractures (Danish). Nord Med 1948;37:277.
15. Burchardt H. The biology of bone graft repair. Clin Orthop Relat Res 1983;174:28-42.
16. Reckling FW, Waters CH 3rd. Treatment of non-unions of fractures of the tibial diaphysis by posterolateral cortical cancellous bone-grafting. J Bone Joint Surg Am 1980;62(6):936-941.
17. Muller ME, Allgower M, Schneider R, Willenegger H. Screws and plates and their application. In: Manual of Internal Fixation. 3rd ed. Ch. 3. New York: Springer-Verlag; 1991. p. 226-228.
18. Kanakis TE, Papadakis E, Orfanos A, Andreadakis A, Xylouris E. Figure eight tension band in the treatment of fractures and pseudarthroses of the medial malleolus. Injury 1990;21(6):393-397.
19. Ostrum RF, Litsky AS. Tension band fixation of medial malleolus fractures. J Orthop Trauma 1992;6(4):464-468.
20. Johnson BA, Fallat LM. Comparison of tension band wire and cancellous bone screw fixation for medial malleolar fractures. J Foot Ankle Surg 1997;36(4):284-289.
21. Shimamura Y, Kaneko K, Kume K, Maeda M, Iwase H. The initial safe range of motion of the ankle joint after three methods of internal fixation of simulated fractures of the medial malleolus. Clin Biomech (Bristol, Avon) 2006;21(6):617-622.
22. Mohammed AA, Abbas KA, Mawlood AS. A comparative study in fixation methods of medial malleolus fractures between tension band wiring and screw fixation. Springer Plus 2016;5:530.
23. Georgiadis GM, White DB. Modified tension band wiring of medial malleolar ankle fractures. Foot Ankle Int 1995;16(2):64-68.
24. Reider B, Falconiero R, Yurkofsky J. Nonunion of a medial malleolus stress fracture. A case report. Am J Sports Med 1993;21(3):478-481.
 |
 |
 |
 |
 |
| Dr. Rakesh John | Prof. Mandeep Singh Dhillon | Dr. Ankit Khurana | Prof. Sameer Aggarwal | Dr. Prasoon Kumar |
| How to Cite This Article: John R, Dhillon M S, Khurana A, Aggarwal S, Kumar P. Tension Band Wiring Is As Effective As A Compression Screw In A Neglected, Medial Maleolus Non-Union: A Case-Based Discussion & Literature Review. Journal of Orthopaedic Case Reports 2017 Jul-Aug;7(4):72-75 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com