[box type=”bio”] Learning Points for this Article: [/box]
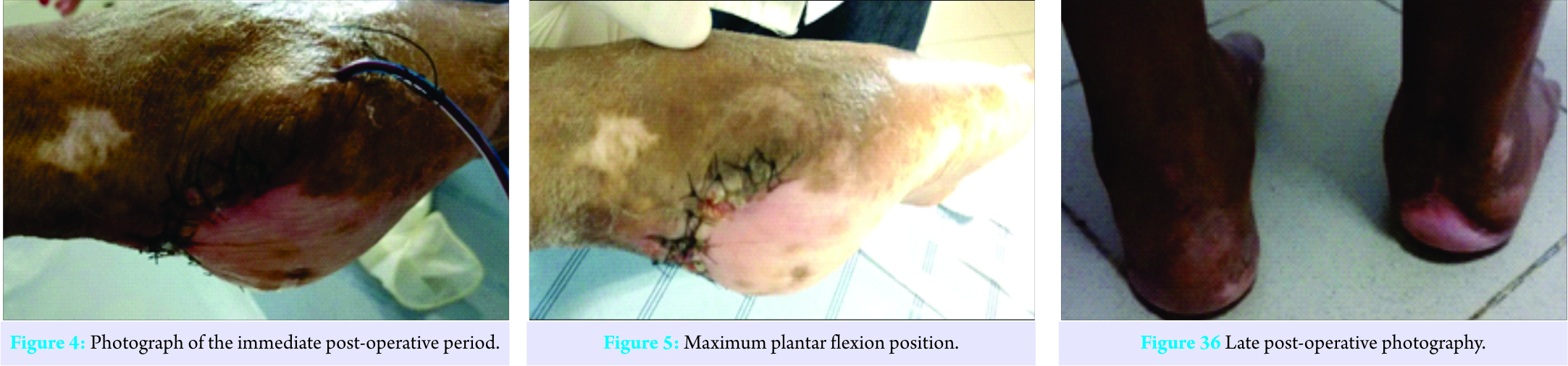
In subtotal calcanectomy surgeries, the position of the ankle in maximal plantar flexion allows the primary closure of the operative wound, without the need for flaps.
Case Report | Volume 7 | Issue 5 | JOCR Sep – Oct 2017 | Page 71-74 | Thiago Batista Faleiro, Alexandre Vasconcelos de Meirelles, Roberto Guimarães Rezende, Herberth Rodrigues Ferreira, Gildásio de Cerqueira Daltro, Renata da Silva Schulz. DOI: 10.13107/jocr.2250-0685.902
Authors: Thiago Batista Faleiro [1], Alexandre Vasconcelos de Meirelles [1], Roberto Guimarães Rezende [1], Herberth Rodrigues Ferreira [1], Gildásio de Cerqueira Daltro [2], Renata da Silva Schulz [3].
[1] Department of Orthopaedics, Brazilian Association of Medicine and Surgery of the Foot and Ankle, Saint Anthony Hospital, Sister Dulce Social Works, Salvador, Brazil.
[2] Department of Orthopaedics, Federal University of Bahia, Rua Doutor Augusto Viana, Canela, Salvador, Brazil,
[3] Jorge Amado University, Paralela, Salvador, Brazil.
Address of Correspondence
Dr. Thiago Batista Faleiro,
Brazilian Association of Medicine and Surgery of the Foot and Ankle,
Saint Anthony Hospital, Sister Dulce Social Works, Av. Bonfim 161, Salvador, Brazil.
E-mail: thiagofaleiro@yahoo.com.br
Abstract
Introduction: Introduction: Subtotal calcanectomy is a therapeutic option for the treatment of chronic ulcer associated with calcaneal osteomyelitis. Closure of the surgical wound can be difficult due to the lack of local cutaneous coverage. We present the first case of subtotal calcanectomy in which the ankle was positioned in plantar flexion allowing the primary closure of the surgical wound without the need for flap.
Case Report: We present a case of 62-year-old female patient with a foot ulcer associated with osteomyelitis. After an initial assessment, a subtotal calcanectomy with primary wound closure was performed. After healing of the surgical wound, the patient started rehabilitation with recovery of dorsiflexion and independent gait without support after 12 weeks.
Conclusion: The result shows that subtotal calcanectomy with the ankle in plantar flexion allows primary closure of the operative wound, without causing difficulty for rehabilitation.
Keywords: Orthopaedics, foot ulcer, osteomyelitis.
Introduction
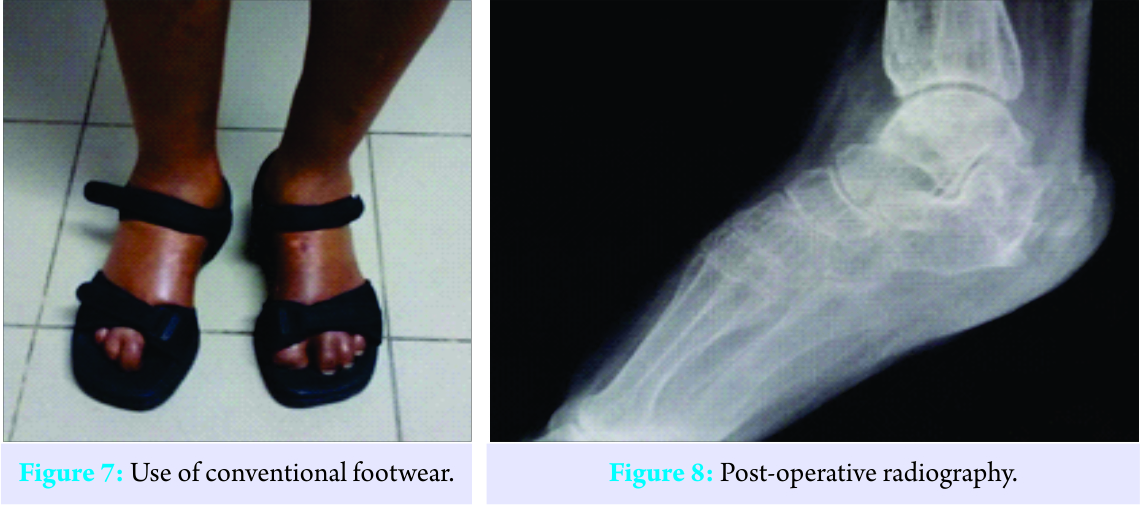
In the diabetic population, osteomyelitis represents one of the main complications of long-term ulcers. In the presence of long-standing ulceration, over 66% of the wounds will progress into the infection of the underlying bone [1]. The risk of amputation in acute diabetic infections is 4 times greater when associated with osteomyelitis than with isolated soft tissue infection. In addition, the presence of osteomyelitis requires a longer duration of antibiotic therapy and a longer duration of hospitalization, thus increasing hospitalization costs for these patients [2]. After amputation of lower limbs in the elderly, about 46% die within the 1st year after surgical intervention. Only 13.67% use prosthesis; while others use a wheelchair for mobility [3]. Thus, the providers are searching for therapeutic alternatives to prevent the need for amputation. We present the first case of subtotal calcanectomy in which the ankle was positioned in maximum plantar flexion allowing the primary closure of the surgical wound without the need for flap. The post-operative evolution shows that the absence of the Achilles tendon allows adequate rehabilitation and recovery of dorsiflexion with gait without support and use of conventional shoes.
Case Report
We present the case of 62-year-old female patient with a history of chronic heel ulcer associated with calcaneal osteomyelitis. She also had the diagnostic of systemic arterial hypertension and diabetes mellitus Type II for 17 years. The patient reported having been admitted to another hospital unit for the treatment of ischemic stroke, which was complicated by peripheral vascular complications and the need for amputation of the right hand, right hallux, and distal phalanx of the left hallux. She also presented with a pressure ulcer associated with the right calcaneal osteomyelitis due to being bedridden for a prolonged period. This was treated with debridement, tenotomy of the calcaneus tendon, and antibiotic therapy in the unit of origin. The culture result showed polymicrobial growth. She was discharged for outpatient follow-up and oral antibiotic therapy with ciprofloxacin and vancomycin. The infection persisted without ulcer healing, and after 14 months of follow-up, she was referred to the Foot and Ankle Surgery Service of Santo Antônio Hospital and was admitted in March 2016. In the initial evaluation, the patient used a wheelchair for mobility due to a posterior calcaneal ulcer with purulent secretion and exposure of necrotic bone tissue (Fig. 1).
She did not present neurological sequelae related to stroke but had bilateral plantar hypoesthesia, symmetrical filiform distal pulses, delayed capillary filling, and operative wounds of healed amputations (Fig. 2 and 3) and a score of 45 on the American Orthopaedic Foot and Ankle Society (AOFAS) scale. After the first consultation, hospital admission was indicated to improve the clinical status and subsequent surgical treatment. Several studies show that adequate glycemic control, nutritional status, and laboratory parameters improve the prognosis of surgery [4, 5, 6]. In April 2016, after 1 month hospitalization, subtotal calcanectomy was performed with excision of all necrotic tissue and primary closure of the wound with the use of a vacuum drain in the first 48 h postoperatively (Fig. 4). The ankle was held in a position of maximal plantar flexion until healing of the lesion to avoid tension on the operative wound (Fig. 5).
The culture result showed polymicrobial growth. The patient was hospitalized for 2 months to receive empirical venous antibiotic therapy with ceftriaxone metronidazole. Antibiotic resistance is at all-time high in all the parts of the world. The high economic burden in the health-care sector has become a burning issue, due to extended hospital stays, isolation wards, stringent infection control measures, and treatment failures [7]. Infections in diabetic feet are often polymicrobial and are related to high prevalence of multi-resistant pathogens [8]. Despite the bacterial resistance to ciprofloxacin and clindamycin initially observed, there was an excellent response to the therapeutic regimen proposed during hospital admission with normalization of the laboratory tests after 8 weeks. Complete healing of the wound occurred 10 weeks after surgery (Fig. 6), at which point it started motor rehabilitation. When the patient presented for evaluation, after 12 weeks of rehabilitation, she had independent gait without support, adaptation to conventional shoes (Fig. 6 and 7) the radiography showed no signs of osteomyelitis (Fig.8), and a score of 90 on the AOFAS scale.
Discussion
Diabetic foot wounds complicated by infection usually result in amputations, thus imposing a large socioeconomic burden on available health-care resources and increasing the morbidity and mortality of the patients affected [9]. The calcaneus is the second most common site for the formation of pressure ulcers, accounting for about 23.6% of all ulcers and most frequently leading to amputation of the lower extremities [10, 11]. Peripheral neuropathy associated with vasculopathy and infection transform the management of cutaneous lesions in patients with ulcer associated with calcaneus osteomyelitis and present a major therapeutic challenge. The use of reconstruction techniques involves the participation of a multidisciplinary team to achieve good clinical results [12]. In the case reported, the patient was followed up by the nursing team, nutrition, clinicians, and orthopaedic surgeons. The care of a multidisciplinary team is important because diabetes and neuropathy are factors of poor prognosis [13]. Priority was given to the indication of a rescue technique due to poor prognosis for adaptation to the prosthesis based on the presenting facts that the patient is elderly, diabetic, and has had previous amputation of the upper limb. Although the secondary wound closure is frequently adopted in patients with osteomyelitis, primary surgical closure has not been associated with a greater number of complications. The patients who received primary surgical closure had faster healing rates and a lower percentage of exudation, edema, and reinfection; factors that determine the delay in wound healing and affect the prognosis of the surgical outcome [14]. The position of the ankle in maximal plantar flexion allowed the primary closure without tension of the wound. There was no difficulty in the recovery of dorsiflexion due to previous tenotomy of the Achilles.
Conclusion
The main purpose of diabetic foot lifesaving approaches is to improve the overall health of the patient and to provide the patient with a stable, full-skinned, planificate, and independent gait member. A proactive surgical approach is often essential to achieve this goal. The good results achieved with the subtotal calcanectomy shown in the present case and the literature, show that this is a technique that should always be considered before an amputation for the treatment of calcaneal osteoarthritis.
Clinical Message
Although chronic osteomyelitis of the calcaneus associated with ulcer is a serious lesion, with poor prognosis, it is possible to perform foot preservation surgery with good results. The calcanectomy should be evaluated as an alternative to transtibial amputation in this group of patients.
References
1. Ramoutar CS, Tierney E, Frykberg R. Osteomyelitis and lower extremity amputations in the diabetic population. J Diabet Foot Complications 2014;2:4.
2. Malhotra R, Chan CS, Nather A. Osteomyelitis in the diabetic foot. Diabet Foot Ankle 2014;5.
3. Hershkovitz A, Dudkiewicz I, Brill S. Rehabilitation outcome of post-acute lower limb geriatric amputees. Disabil Rehabil 2013;35:221-7.
4. Tubili C. Nutritional status in diabetic patients with foot ulcers: Bioelectrical analysis in routine evaluation. Mediterr J Nutr Metab 2014;7:181-4.
5. Gau BR, Chen HY, Hung SY, Yang HM, Yeh JT, Huang CH, et al. The impact of nutritional status on treatment outcomes of patients with limb-threatening diabetic foot ulcers. J Diabetes Complications 2016;30:138-42.
6. Akiboye F, Rayman G. Management of hyperglycemia and diabetes in orthopedic surgery. Curr Diab Rep 2017;17:13.
7. Zaman SB, Hussain MA, Nye R, Mehta V, Mamun KT, Hossain N, et al. A review on antibiotic resistance: Alarm bells are ringing. Cureus 2017;9:e1403.
8. Perim MC, Jda CB, Celeste SR, Ede FO, Mendes RR, Mendes GO, et al. Bacteriological study of diabetic foot. Rev Soc Bras Med Trop 2015;48:546-54.
9. Fisher TK, Scimeca CL, Bharara M, Mills JL Sr, Armstrong DG. A step-wise approach for surgical management of diabetic foot infections. J Vasc Surg 2010;52:72S-75.
10. Evans KK, Attinger CE, Al-Attar A, Salgado C, Chu CK, Mardini S, et al. The importance of limb preservation in the diabetic population. J Diabetes Complications 2011;25:227-31.
11. Vangilder C, Macfarlane GD, Meyer S. Results of nine international pressure ulcer prevalence surveys: 1989-2005. Ostomy Wound Manage 2008;54:40-54.
12. Zgonis T, Stapleton JJ, Rodriguez R, Girard-Powell VA, Cromack DM. Plastic surgery reconstruction of the diabetic foot. Assoc Perioper Regist Nurse J 2008;87:951-70.
13. Merlet A, Cazanave C, Dauchy FA, Dutronc H, Casoli V, Chauveaux D, et al. Prognostic factors of calcaneal osteomyelitis. Scand J Infect Dis 2014;46:555-60.
14. Morales EG, Martınez JL, Sanchez JA, Matilla AC, Alvarez YG, Montesinos JV. Surgical complications associated with primary closure in patients with diabetic foot osteomyelitis. Diabet Foot Ankle 2012;3:10.
| How to Cite This Article: Thiago Batista Faleiro, Alexandre Vasconcelos de Meirelles, Roberto Guimarães Rezende, Herberth Rodrigues Ferreira, Gildásio de Cerqueira Daltro, Renata da Silva Schulz. Subtotal Calcanectomy for the Treatment of Chronic Ulcer Associated with Osteomyelitis: A Case Report . Journal of Orthopaedic Case Reports 2017 Sep-Oct;7(5):71-74 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com