[box type=”bio”] Learning Points for this Article: [/box]
Compression plating is considered the gold standard for humeral shaft fractures and non-union secondary to failed interlocking nailing is a challenging situation. Avoiding unnecessary surgical procedures and performing meticulous soft tissue dissection are some of the factors which reduce the incidence of humeral non-union.
Case Report | Volume 7 | Issue 5 | JOCR Sep – Oct 2017 | Page 80-83 | Jagdeep Singh, Anoop Kalia, Kavin Khatri, Anshul Dahuja. DOI: 10.13107/jocr.2250-0685.906
Authors: Jagdeep Singh [1], Anoop Kalia [1], Kavin Khatri [1], Anshul Dahuja [1].
[1] Department of Orthopaedics, Guru Gobind Singh Medical, College and Hospital, Faridkot, Punjab, India.
Address of Correspondence
Dr. Kavin Khatri,
Department of Orthopaedics, Guru Gobind Singh
Medical College and Hospital, Faridkot, Punjab, India.
E-mail: kavinkhatri84@gmail.com
Abstract
Introduction: Humerus non-union is a challenging situation for the surgeon and devastating and morbid situation for the patient. Surgical approach to the humerus is demanding because of the complex neurovascular anatomy and especially when previous surgeries have been attempted.
Case Report: We report a case of a young adult male who sustained a compound fracture of humerus shaft treated with intramedullary nailing followed by subsequent bone grafting and eventually landed up in non-union and was treated at our center by locking compression plate application with nail in situ with iliac crest autogenous bone graft followed by shoulder spica application.
Conclusion: Although humerus nailing is a valid therapeutic option for humeral shaft fractures, compression plating is considered the gold standard and non-union secondary to failed interlocking nailing is a challenging situation.
Keywords: Non-union, compression plating, interlocking nailing.
Introduction
Humerus shaft fractures have excellent healing ability due to rich blood supply provided by soft tissue and muscular envelopes. More than 90% union rates have been reported with non-operative management [1]. Angulatory, rotatory, and axial deformities are compensated by wide range of motion at shoulder and elbow joints. 20° of anterior angulation, 30° of varus, and 3 cm of bayonet apposition are well acceptable [2]. The incidence of non-union after operative treatment of humeral shaft fractures has been reported to be ranging between 2.5% and 13% [3, 4, 5, 6]. It has been reported that non-union after nailing has higher rates as compared to plate osteosynthesis mainly due to excessive motion or distraction at fracture site [7]. Humerus non-union is defined as a fracture which shows no signs of healing 24 weeks after injury [8].
Case Report
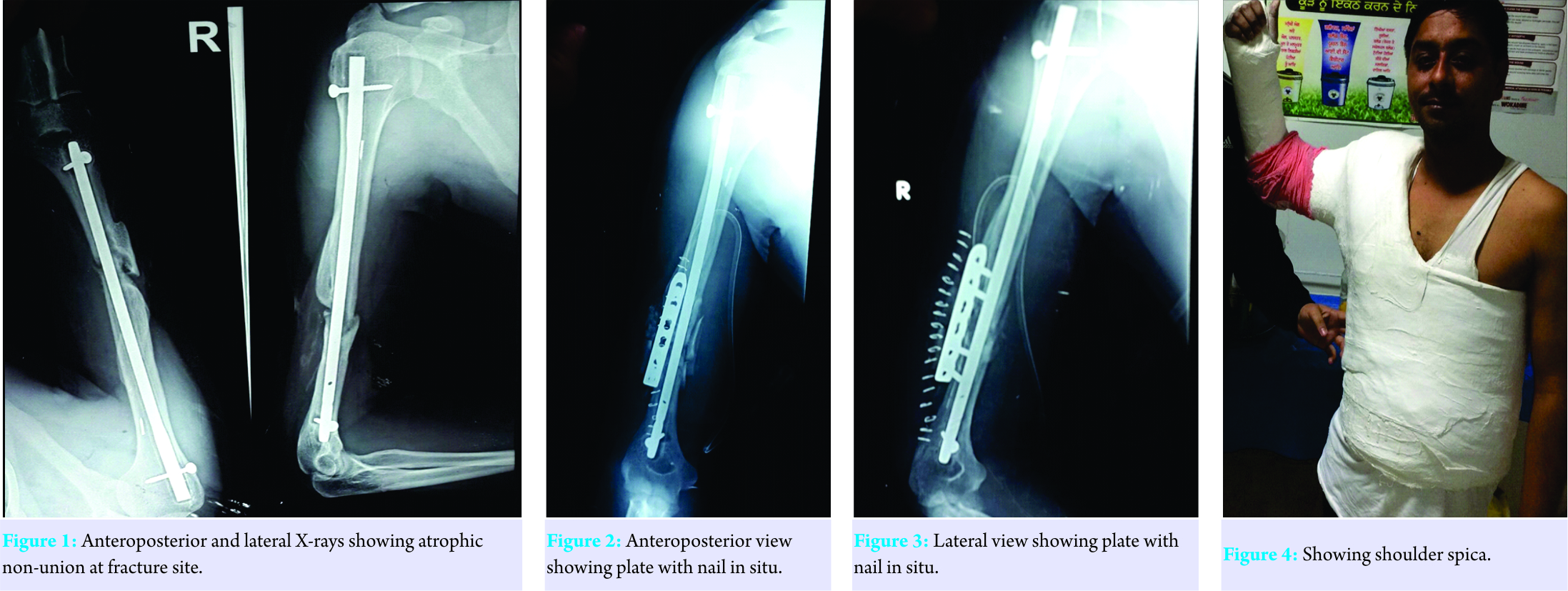
A 35-year-old young adult male presented to our department with pain over lower one-third of the right arm. Detail history taking revealed that the patient was a chronic smoker and alcoholic who sustained a compound fracture of the right shaft humerus 1 year back for which he underwent interlocking nailing at some private center. He further told us that the operating surgeon did iliac crest bone grafting 6 months after the initial surgery when no signs of union were evident. However, in spite of that, no signs of union were seen and he had persistent pain at fracture site when he used to perform household activities. He again went to the operating surgeon who referred the patient to our center. We got the anteroposterior and lateral X-rays done which revealed atrophic non-union at fracture site with one locking hole proximally and one distally (Fig. 1).
The nail seemed to be of appropriate diameter well seated in the medullary canal and removal of nail would have caused more damage to the rotator cuff. The patient was in a lot of mental trauma after the failed previous two surgeries, so he was counseled properly, and the decision was made to apply a locking compression plate (LCP) with nail in situ with iliac crest autogenous bone grafting. The patient being a chronic smoker and alcoholic was told that both smoking and alcohol cessations were mandatory before any definitive procedure and he agreed to that. After the preanesthetic checkup clearance, the patient was taken up in the theater; fracture site was opened posteriorly using triceps-splitting approach. As expected, there was rotational instability at the fracture site and no signs of callus formation were seen. The fracture margins were freshened till bleeding bone was visualized, fibrous tissue cleared, and locking compression with two monocortical holes on each side was applied along with bone graft harvested from iliac crest. Immediate post-operative anteroposterior and lateral radiograph were obtained (Fig. 2 and 3). After the stitches were removed and wound healed satisfactory, the patient was given shoulder spica to further ensure immobilization (Fig. 4). Shoulder spica was removed after 1 month and aggressive physiotherapy was started. Follow-up at the end of 6 months showed solid union at fracture site (Fig. 5) and excellent range of motion (Fig. 6a and b).
Discussion
Open reduction and plate osteosynthesis as well as closed intramedullary (IM) nailing can be done for humerus shaft fractures and both methods have their advantages and disadvantages. Osteosynthesis with plating allows direct visualization of radial nerve, causes minimal shoulder and elbow dysfunction, and also the construct is more stable and is associated with more union rates while non-union, malunion, radial nerve injury, and hardware failure are some of the disadvantages [7]. Closed IM nailing of humerus has various advantages as the procedure is less time consuming, low incidence of radial nerve palsy, and preservation of soft tissue envelope while the complications being shoulder stiffness and high rates of non-union. Non-union after interlock nailing of humerus is attributed to many factors including distraction at fracture site, excessive mobility at fracture site, disruption of nutrient artery during nailing, excessive comminution, infection, compound injuries, as well as inadequate surgical technique. Humerus diaphyseal non-unions can be treated with various internal and external fixation methods [9, 10, 11, 12]. Humerus non-union after failed IM nailing is a challenging situation and non-union rates range between 0% and 50% after IM nailing of humerus [13, 14, 15, 16]. On review of literature, it was found that authors have reported that the results of surgery in diaphyseal humerus non-unions are worse in patients previously treated with IM nailing than the patients managed conservatively or treated with compression plates [17, 18]. Exchange nailing to manage humerus non-union treated previously with IM nail has not been found to be effective [19]. One of the authors compared exchange nailing and compression plating in patients with humerus non-unions after failed locked IM nails. Compression plating achieved union in 9 out of 9 patients while exchange nailing achieved union in only 4 out of 10 patients [17]. Bone loss at non-union site, cortical thinning due to windshield wiper effect [19], and absence of cyclical loading in humerus [17] are some of the reasons why exchange nailing in non-union secondary to failed IM nailing is not a valid option in humerus. Authors have reported the use of plates with humerus nail in situ to manage the non-union secondary to IM nailing achieving union in all the 6 cases [18]. The amount of medullary canal occupied by the nail to determine the length of the plate and the type of screws to be used and the type of non-union to determine whether there is bone defect are some of the things to be stressed on by the operating surgeon if he decides to keep the nail in situ and perform supplemental plate fixation. When plates are used with nail in situ, they compress the nail against the bone improving the bone–nail interface and improved rotational stability at fracture site. Besides, surgical factors patient-related factors also account for humeral non-unions as in our case. Smoking [10] and alcohol [4] have both been implicated as risk factor for humeral non-unions.
Conclusion
Humeral shaft fractures can be managed conservatively, but when the decision to operate has been made, then the surgeon must be familiar with pros and cons of each type of operative intervention. Avoiding unnecessary surgical procedures and performing meticulous soft tissue dissection are some of the factors which reduce the incidence of humeral non-union. LCP, when used with nail in situ, has the advantages that even monocortical screws can be used where the nail occupies the majority of the diameter of humeral canal.
Clinical Message
Although excellent results have been reported with conservative treatment of humerus shaft fractures, when a decision is made to operate shaft humerus fractures, compression plating remains the gold standard. Meticulous surgical dissection should be performed so as to maximally preserve the fracture biology. Humerus non-union secondary to interlocking nailing is a complex situation to manage and poses a significant challenge both to the patient as well as the surgeon. Detailed personal history taking should be done before commencing the treatment, and if anything detrimental for fracture union, for example, smoking is found, it should be immediately stopped.
References
1. Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J, et al. Humeral nailing revisited. Injury 2008;39:1319-28.
2. Egol KA, Koval KJ, Zuckerman JD. Humeral shaft fractures. In: Egol KA, Koval KJ, Zuckerman JD, editors. Handbook of Fractures. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. p. 203-13.
3. Foster RJ, Dixon GL, Bach AW, Appleyard RW, Green TM. Internal fixation of fractures and nonunions of the humeral shaft. J Bone Joint Surg (Am) 1985;67(A): 857-65.
4. Foulk DA, Szabo RM. Diaphyseal humerus fractures: Natural history and occurrence of nonunion. Orthopedics 1995;18:333-5.
5. Healy WL, White GM, Mick CA, Brooker AF Jr. Weiland AJ. Nonunion of the humeral shaft. Clin Orthop Relat Res 1987;219:206-13.
6. Rosen H. The treatment of nonunious and psedoarthrosis of the humeral shaft. Orthop Clin North American 199021:725-42.
7. McKee MD, Larsson S. Humeral shaft fractures. In: Bucholz RW, Court-Brown CM, Heckman JD, Tornetta P III, editors. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. p. 999-1038.
8. Hierholzer C, Sama D, Toro JB, Peterson M, Helfet DL. Plate fixation of ununited humeral shaft fractures: Effect of type of bone graft on healing. J Bone Joint Surg Am 2006;88:1442-7.
9. Bosch U, Skutek M, Kasperczyk WJ, Tscherne H. Nonunion of the humeral diaphysis-operative and nonoperative treatment. Chirurg 1999;70:1202-8.
10. Lammens J, Baudin G, Driesen R, Driesen R, Moens P, Stuyck J, et al. Treatment of nonunion of the humerus using the Ilizarov external fixator. Clin Orthop 1998;353:223-30.
11. Ring D, Jupiter JB, Quintero J, Sanders RA, Marti RK. Atrophic ununited diaphyseal fractures of the humerus with a bony defect: Treatment by wave-plate osteosynthesis. J Bone Joint Surg Br 2000;82:867-71.
12. Wenzl ME, Fuchs S, Schmidt HG, Wolter D. Titanium internal fixator systems the upper extremity. Trauma Berufskrankh 2001;3 Suppl 4:454-60.
13. Dujardin FH, Mazirt N, Tobenas AC, Duparc F, Thomine JM. Failure of locked centro-medullary nailing in pseudarthrosis of the humeral diaphysis. Rev Chir Orthop Reparatrice Appar Mot 2000;86:773-80.
14. Svend-Hansen H, Skettrup M, Rathcke MW. Complications using the seidel intramedullary humeral nail: Outcome in 31 patients. Acta Orthop Belg 1998;64:291-5.
15. Bain G, Sandow M. Treatment of humeral shaft fractures with the Seidel intramedullary nail. Joint Surg Br 1992;748:39.
16. Farragos AF, Schemitsch EH, McKee MD. Complications of intramedullary nailing for fractures of the humeral shaft: a review. J Orthop Trauma 1999;13:258-67.
17. McKee MD, Miranda MA, Riemer BL, Blasier RB, Redmond BJ, Sims SH, et al. Management of humeral nonunion after the failure of locking intramedullary nails. J Orthop Trauma 1996;10:492-9.
18. Ring D, Jupiter J. Humerus nonunion after intramedullary rod fixation. Locking compression plate without removing the nail. Tech Orthop 2004;18:356-9.
19. Brinker MR, O’Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am 2007;89:177-88.
| How to Cite This Article: Singh J, Kalia A, Khatri K, Dahuja A. Resistant Non-union of Humerus After Intramedullary Nailing Treated with Locking Compression Plate with Bone Grafting With Nail in Situ and Shoulder Spica: A Case Report. A Case Report. Journal of Orthopaedic Case Reports 2017 Sep-Oct;7(5):80-83 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com