[box type=”bio”] What to Learn from this Article?[/box]
Complete response of primary lymphoma of acetabulum to chemotherapy may induce good remodeling and delay primary surgical interference.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 6-9| Karem M. Zekry, Norio Yamamoto, Katsuhiro Hayashi, Akihiko Takeuchi, Hiroyuki Tsuchiya. DOI: 10.13107/jocr.2250-0685.924
Authors: Karem M. Zekry [1, 2], Norio Yamamoto [1], Katsuhiro Hayashi [1], Akihiko Takeuchi [1], Hiroyuki Tsuchiya [1]
[1] Department of Orthopaedic Surgery, Graduate School of Medical Science, Kanazawa University, Kanazawa, Japan,
[2] Department of Orthopaedic Surgery, Faculty of Medicine, Minia University, Minia, Egypt.
Address of Correspondence:
Dr. Hiroyuki Tsuchiya,
Department of Orthopaedic Surgery, Graduate School of Medical Science, Kanazawa University, 13-1 Takaramachi, Kanazawa, 920-8641, Japan.
E-mail: tsuchi@med.kanazawa-u.ac.jp
Abstract
Introduction: Primary lymphoma of the bone (PLB) is uncommon clinical entity with the vast majority of the cases are non-Hodgkin’s lymphoma. Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of PLB.
Case Report: We report a case of 60-year-old female presented with pain in the right hip that persisted for 2months. Plain X-ray, computed tomography, and magnetic resonance imaging of the right hip showed a lytic lesion involving the right acetabulum and adjoining iliac bone with extraosseous mass. The histopathological and immunohistochemical examination confirmed a diagnosis of DLBCL. Treatment with cyclophosphamide, epirubicin, vincristine, and prednisone plus rituximabestablished a complete response (CR) with remodeling of the acetabulum. At the last follow-up, the patient had the ability to walk without any support which obviates the need of primary surgical interference for the tumor.
Conclusion: The PLB must be considered in the differential diagnosis of lytic lesions involving the pelvic bones in older adults, especially when accompanied by extraosseous soft tissue mass. Our patient of PLB showed goodremodeling of the acetabular area after CR to chemotherapy without primary surgical interference for the tumor with the limitation of weight-bearing during chemotherapy treatment to prevent fracture.
Keywords: B-cell lymphoma, primary lymphoma of the bone, non-Hodgkin’s lymphoma.
Introduction
According to the WHO classification, primary lymphoma of the bone (PLB) is defined as a monostotic disease involving single skeletal site with or without involvement of the regional lymph nodes, or as a polyostotic disease affecting multiple skeletal sites without visceral or lymph node involvement [1]. PLB is an uncommon disease and constitutes <5% of malignant bone tumors, 4–5% of extranodal lymphoma, and <1% of all non-Hodgkin’s lymphoma. Most cases of PLB are of diffuse large B-cell lymphoma (DLBCL) subtype [2]. The etiology of PLB is not well-known and can involve any part of the skeleton [3]. As PLB has a better response to therapy, it is essential to differentiate it from other causes of lytic bone lesions, such as carcinomas and other primary bone tumors [4]. We report a case of PLB (DLBCL subtype) of the right acetabulum, which is a rare presentation, in whom local control was achieved with chemotherapy alone without any need of surgical interference to reconstruct the acetabular area. Patient provided written informed consent for this report.
Case Report
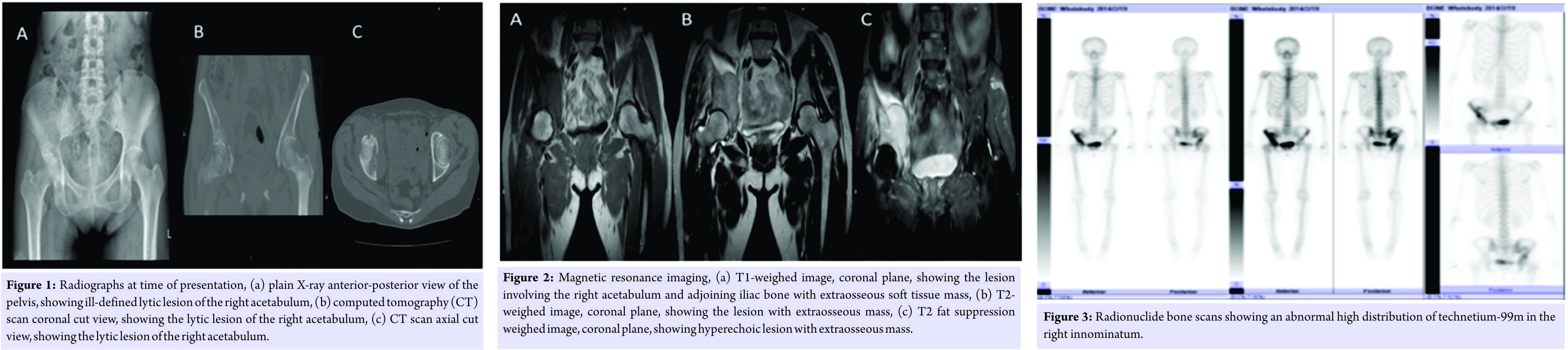
A 60-year-old female presented to our Department of Orthopedic Surgery, Kanazawa University Hospital, in February 2014, with pain in the right hip and low-grade fever that persisted for 2months. Clinical examination neither revealed painful range of motion of the right hip without obvious swelling nor enlarged lymph nodes. Plain X-ray showed ill-defined lytic lesion of the right acetabulum. Computed tomography (CT) and magnetic resonance imaging (MRI) showed a destructive lytic lesion of the right acetabulum and adjoining iliac bone with an extraosseous mass. Technetium-99m (99mTc) radionuclide bone scans were performed to exclude multiple bone lesions and showed increased tracer uptake in the right innominatum, including the ilium and acetabulum. 18F-fluorodeoxyglucose-positron emission tomography-CT (FDG-PET-CT) scan showed abnormal 18F-FDG uptakes involving the right innominatum.
Next, a CT-guided needle biopsy of the lesion was performed, and a histopathological examination showed diffuse infiltration of round tumor cells of approximately the same size. Immunohistochemistry showed that the cell membrane was strongly positive for cluster of differentiation (CD)20, CD79α, and CD3 and negative for CD5, and CD10 supporting a B-cell origin. Further examinations, including bone marrow aspiration and biopsy, and CT scans of the neck, chest, and abdomen, were normal.
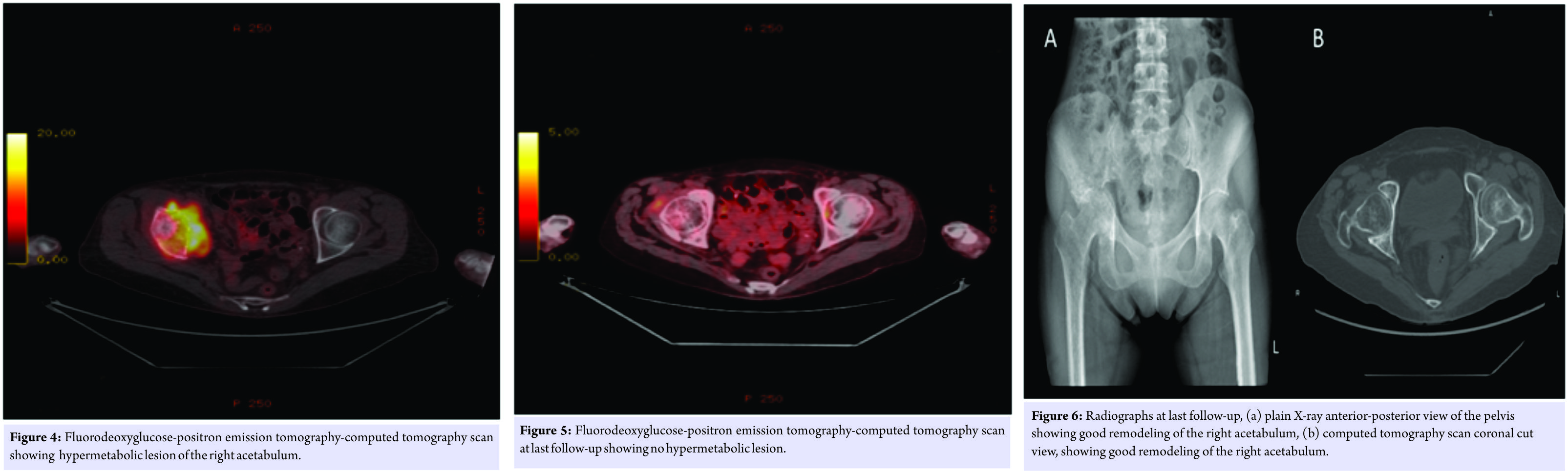
The patient was diagnosed with PLB of the right acetabulum (DLBCL subtype). The patient was treated with six cycles of R-CHOP regimen (1000 mg cyclophosphamide, 80 mg epirubicin, and 2 mg vincristine on day 1, and 100 mg prednisone on days 1-5, every 3weeks plus rituximab). During chemotherapy treatment, only partial weight-bearing with crutches was allowed. During follow-up, the MRI and CT showed marked shrinkage of the tumor with the good remodeling of bone, and at last follow-up, the patient was in a very good condition with no pain of the right hip and achieved a complete response (CR), as confirmed by FDG-PET-CT. The patient had the ability to walk without any type of support, and no surgical interference was planned to reconstruct the acetabular area.
Discussion
Clinically, most of PLB patients are >45 years of age with a slight male preponderance (male: female=1.2:1.8) [5]. Any region of the skeleton can be involved, however, Heyning. The femur is the most commonly affected site, which accounts for 50% of the cases. The secondary affected site is the pelvis with a proportion of 20%, while other sites include the spine, ribs, mandible, scapula, and proximal phalanx of the thumb [6]. Patients with PLB commonly present with local bone pain, a mass, softtissue swelling, pathological fracture, or hypercalcemic crisis [7]. At the time of initial presentation, the plain X-rays are usually normal. A solitary lytic lesion with a permeative or moth-eaten pattern of destruction, and a periosteal reaction may be observed in aggressive types, and this appearance should be differentiated from osteosarcomas and Ewing’s sarcoma. 99mTc radionuclide bone scans show increased tracer uptake in 98% of patients, with markedly increased activity in 64% of patients, which are usually non-specific [8]. CT is useful in delineating cortical destruction. However, the features are usually non-specific. Following successful treatment, CT shows bone remodeling with a persistent architecture that is similar to that of Paget’s disease of the bone [9]. On T1-weighted MRI, the signal intensities in the lesion range between isointense and hypointense, while on T2-weighted MRI, the signal intensities are varied [10]. Within months of successful treatment, a rapidly decreasing tumor volume can be observed, with complete disappearance of the soft tissue component. Minor bone marrow signal abnormalities that have no clinical relevance may persist for up to 2 years [9]. PLB usually shows abnormal 18F-FDG uptake on FDG-PET-CT. PET-CT is an essential tool for precisely determining a response to therapy. In cases of CR, PET scanning shows no hypermetabolic lesions, with a rapid decline in FDG uptake [11]. Over the past two decades, chemotherapy (CHOP-based) has been considered the standard treatment for PLB with or without radiotherapy. Radiotherapy has been used alone or in combination with chemotherapy. Radiotherapyalone in limited-stage disease resulted in a poor5-year overall survival (OS) of 45% even when patients have been carefully selected for apparently limited-stage disease [12]. The introduction of rituximab since March 2001 resulted in a real improvement in the progression-free survival (PFS) for patients with problem-based learning (PBL); the 3-year PFS for patients who treated with CHOP plus rituximab was 88% compared with 52% for those who treated with standard CHOP alone (P = 0.025) [13]. The role of radiotherapy in advanced stage PBL is controversial. In a study by Ramadan et al., patients with advanced-stage disease, who were treated with chemotherapy plus radiotherapy, had a poorer outcome compared with those who treated with chemotherapy alone (10-year OS was 25% and 56%, respectively) [13]. In our case, the complete local tumor control was achieved with chemotherapy alone. The surgery is indicated only for prophylactic fixation of impending fractures or the treatment of pathological fractures or spinal cord compression [4]. In this case, we present a PLB lesion of the right acetabulum, which is a rare clinical entity. The differential diagnoses for this lesion include osteosarcoma, Ewing sarcoma, and chondrosarcoma, and therefore, the CT-guided biopsy was required for the diagnosis. This case is a well-documented case that PLB can be successfully managed by chemotherapy alone (R-CHOP-based chemotherapy) with good remodeling of the bone even if the acetabular area was severely involved with invasion of the articular surface and reinforces the evidence that the CT, MRI, and FDG-PET-CT are useful imaging modalities for the evaluation and follow-up of the successful response of lymphoma to chemotherapy.
Conclusion
The PLB must be considered in the differential diagnosis of lytic lesions involving the pelvic bones in older adults, especially when accompanied by extraosseous soft tissue mass. Our patient of PLB showed good remodeling of the acetabular area after CR to chemotherapy without primary surgical interference for the tumor with the limitation of weight-bearing during chemotherapy treatment to prevent fracture. The total hip arthroplasty may be needed in the future for management of secondary degenerative changes of the hip so that long-term follow-up is recommended.
Clinical Message
Although primary lymphoma of the acetabulum is a rare entity, it must be considered in the differential diagnosis of the pelvic lesions involving the acetabulum. CR to chemotherapy may induce good remodeling of the acetabulum even if the lesion is lytic with the involvement of subchondral bone and this may delay primary surgical interference.
References
1. Unni KK, Hogendoorn PC.Hematopoietic neoplasms. In: World Health Organization Classification of Tumors, Pathology and Genetics of Tumors of Soft Tissue and Bone. Lyon: IARC Press; 2002. p. 301-8.
2. Lakshmaiah KC, Guruprasad B, Purohit S, Rao S, Bishwas S, Lokanath D. Primary non-Hodgkin’s lymphoma of bone: Poly-ostotic versus mono-ostotic subtypes. Ecancermedicalscience 2013;7:330.
3. Heyning FH, Hogendoorn PC, Kramer MH, Hermans J, Kluin-Nelemans JC, Noordijk EM,et al. Primary non-Hodgkin’s lymphoma of bone.Aclinicopathological investigation of 60 cases. Leukemia 1999;13:2094-8.
4. Zhou H, Gao F, Bu B, Fu Z, Sun X, Huang C,et al. Primary bone lymphoma: A case report and review of the literature. Oncol Lett 2014;8:1551-6.
5. Jawad MU, Schneiderbauer MM, Min ES, Cheung MC, Koniaris LG, Scully SP.Primary lymphoma of bone in adult patients. Cancer 2010;116:871-9.
6. Bao J. Young males with primary lymphoma of bone presenting with musculoskeletal pain are prone to be misdiagnosed as ankylosing spondylitis: A case report. Rheumatol Int 2012;32:263-4.
7. Catlett JP, Williams SA, O’Connor SC, Krishnan J, Malkovska V. Primary lymphoma of bone: An institutional experience. Leuk Lymphoma 2008;49:2125-32.
8. Niitsu N, Nakayama M, Umeda M. A clinical study of primary lymphoma of bone. Rinsho Ketsueki 1998;39:432-5.
9. Power DG, McVey GP, Korpanty G, Treacy A, Dervan P, O’Keane C,et al. Primary bone lymphoma. Single institution case series. Ir J Med Sci 2008;177:247-51.
10. Barbieri E, Cammelli S, Mauro F, Perini F, Cazzola A, Neri S, et al. Primary non-Hodgkin’s lymphoma of the bone: Treatment and analysis of prognostic factors for Stage I and Stage II. Int J Radiat Oncol Biol Phys 2004;59:760-4.
11. Fidias P, Spiro I, Sobczak ML, Nielsen GP, Ruffolo EF, Mankin H,et al. Long-term results of combined modality therapy in primary bone lymphomas. Int J Radiat Oncol Biol Phys 1999;45:1213-8.
12. Baar J, Burkes RL, Bell R, Blackstein ME, Fernandes B, Langer F. Primary non-Hodgkin’s lymphoma of bone: A clinic-pathological study. Cancer 1994;73:1194-9.
13. Ramadan KM, Shenkier T, Sehn LH, Gascoyne RD, Connors JM. A clinic-pathological retrospective study of 131 patients with primary bone lymphoma: A population-based study of successively treated cohorts from the British Columbia cancer agency. Ann Oncol 2007;18:129-35.
 |
 |
 |
 |
 |
| Dr. Karem M. Zekry | Dr. Norio Yamamoto | Dr. Katsuhiro Hayashi | Dr. Akihiko Takeuchi | Dr. Hiroyuki Tsuchiya |
| How to Cite This Article: Zekry KM, Yamamoto N, Hayashi K, Takeuchi A, Tsuchiya H. Primary Lymphoma of the Pelvis:A Case Report. Journal of Orthopaedic Case Reports 2017 Nov-Dec; 7(6): 6-9 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com