[box type=”bio”] What to Learn from this Article?[/box]
Although extremely rare, Scheie syndrome patients may develop cervical myelopathy; treating physicians should be aware of the high risks of anesthesia, as well as of the nature of the disease which may not allow for fusion.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 27-30| Farzam Vazifehdan, Vasilios G Karantzoulis, Robert Ebner, Vasilios G Igoumenou. DOI: 10.13107/jocr.2250-0685.936
Authors: Farzam Vazifehdan [1], Vasilios G Karantzoulis [1], Robert Ebner [1], Vasilios G Igoumenou [1, 2]
[1] Spine Center Stuttgart, Paulinenhilfe, Diakonie-Klinikum, Stuttgart, Germany.
[2] Department of Orthopaedics, National and Kapodistrian University of Athens, School of Medicine, Athens, Greece.
Address of Correspondence:
Dr. Vasilios G Igoumenou,
Spine Center Stuttgart, Paulinenhilfe, Diakonie-Klinikum, Stuttgart, Germany, 38 Rosenbergstrasse, 70176, Stuttgart, Germany.
E-mail: vasigou@med.uoa.gr
Abstract
Introduction: Scheie syndrome is an extremely rare systematic disease that represents the most attenuated form of mucopolysaccharidosis Type I disorder. Although associated with a variety of manifestations, Scheie syndrome leading to the development of cervical myelopathyis yet to be reported. Our purpose was to present a unique case of a Scheie syndrome patient, who underwent surgery due to cervical myelopathy, and to discuss the clinical and imaging findings, as well as the challenges and outcomes of surgical treatment.
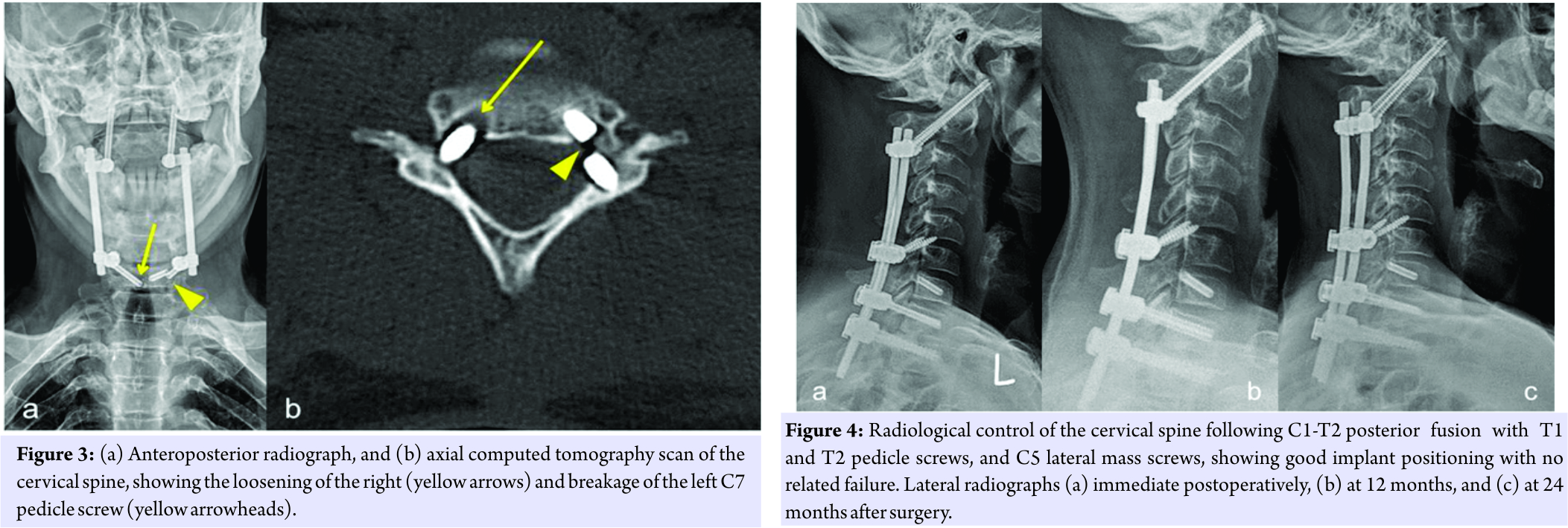
Case Report: A 33-year-old man with Scheie syndrome presented with neck and radicular pain, upper extremity weakness, and insecure gait. The workup studies revealedcervical spine stenosis at multiple levels, caused by accumulation of soft tissue, within the cervical spinal canal. Despite the high risks of anesthesia, and the patient’s inherent poor bone quality that could lead to failure of spinal fusion, we decided to proceed with surgery; indeed, decompressive laminectomies combined with C1-7 posterior stabilization led to immediate pain relief.Despite counter advised, the patient returned to sports rather early, and 6months after index procedure neck pain relapsed, while screw breakage and cutout occurred at the level of C7. Consequently, the initial instrumentation was revised and extended at T2 level. At 2years follow-up, the patient remained continuously pain-free and ambulatory.
Conclusion: Although cervical myelopathy in Scheie syndrome represents an extremely rare entity,it can make a severe impact on patients’ quality of life. If timely managed though, these patients can be offered a significant relief from symptoms. Surgery is rather challenging and treating physicians should be aware of the high risks of anesthesia. Especially spine surgeons should be aware of the nature of the disease, since it may not allow for fusion, causing instrumentation to fail.
Keywords: Scheie syndrome, mucopolysaccharidosis, cervical myelopathy, surgical management.
Introduction
Mucopolysaccharidoses (MPS) represent a group of inherited disorders caused by incomplete degradation and storage of acid mucopolysaccharides, which are major components of the intercellular substance of connective tissue [1]. With seven types and several subtypes that have been described, MPS disorders, apart from being progressive and multivisceral diseases, present a clinical spectrum of great variance that involves the musculoskeletal system, heart, lungs, eyes (cornea, retina and optic nerves), liver, spleen, and in some cases the CNS [2]. MPS type I (MPS I) is an autosomal-recessive inherited lysosomal storage disease caused by a deficiency of the enzyme alpha-L-iduronidase, which results in the accumulation of dermatan sulfate and heparan sulfate [1, 3]. Three subtypes of the disease have been described, which in a descending order of severity are: Hurler syndrome (MPS IH), Hurler-Scheie syndrome (MPS IH/S), and Scheie syndrome (MPS IS) [3]. With an overall prevalence of 1/100,000 live births and significant variability in presentation, diagnosis of MPS I in all its forms poses a true challenge [4]. The true incidence of MPS IS remains unknown, but two European studies have estimated it to range between 0.5/1,000,000 and 0.7/1,000,000 births [5, 6]. Issues involving the cervical spine are common in MPS patients, therefore careful monitoring is required since surgery may be necessary [7, 8]. However, the associated medical conditions (airway obstruction, cardiac valvulopathy) and the risk of neurological impairment constitute surgical management highly demanding [1]. Moreover, the inherent poor bone quality of these patients constitutes spinal fusion a surgical challenge, since fusion often fails. Scarce evidence exist in the literature regarding surgical management of cervical myelopathy in MPS I [9]. We report a patient with MPS IS, who developed cervical myelopathy, aiming to provide insights to the treating physicians regarding this rare entity. To the best of our knowledge, the aforementioned case is unique in that a Scheie syndrome patient underwent spine surgery due to cervical spinal cord compression.
Case presentation
A 33-year-old man with MPS IS presented neck and radicular pain with an onset of symptoms of three months, along with a recent onset of insecure gait, of about two weeks. The patient was of below-average stature, and regarding his metabolic disease he claimed that he had never received any treatment. In addition, he maintained a rather athletic lifestyle, which was significantly affected by the presenting symptomatology. Conservative treatment had not been able to relieve him from his symptoms, and clinical examination showed sensorimotor deficits corresponding to C6 and C7 dermatomes bilateral with the left upper extremity being slightly more affected. Bilateral paresthesias were also present over the plantar sides of the feet, along with hyperreflexia of the left leg. Bilateral upper extremity weakness [4/5] in three muscle groups was noticed, and the electrophysiological study that was performed was indicative of myelopathy. Plain radiographs were consistent with the characteristic abnormal vertebral formation that occurs in MPS, without evidence of atlantoaxial instability whatsoever (Fig. 1). Μagnetic resonance (MR) imaging revealed spinal stenosis at C2-5 levels with concomitant myelopathic hyperintense signs, secondary to a marked soft tissue thickening that was lying mainly posterior to the dens (Fig. 2).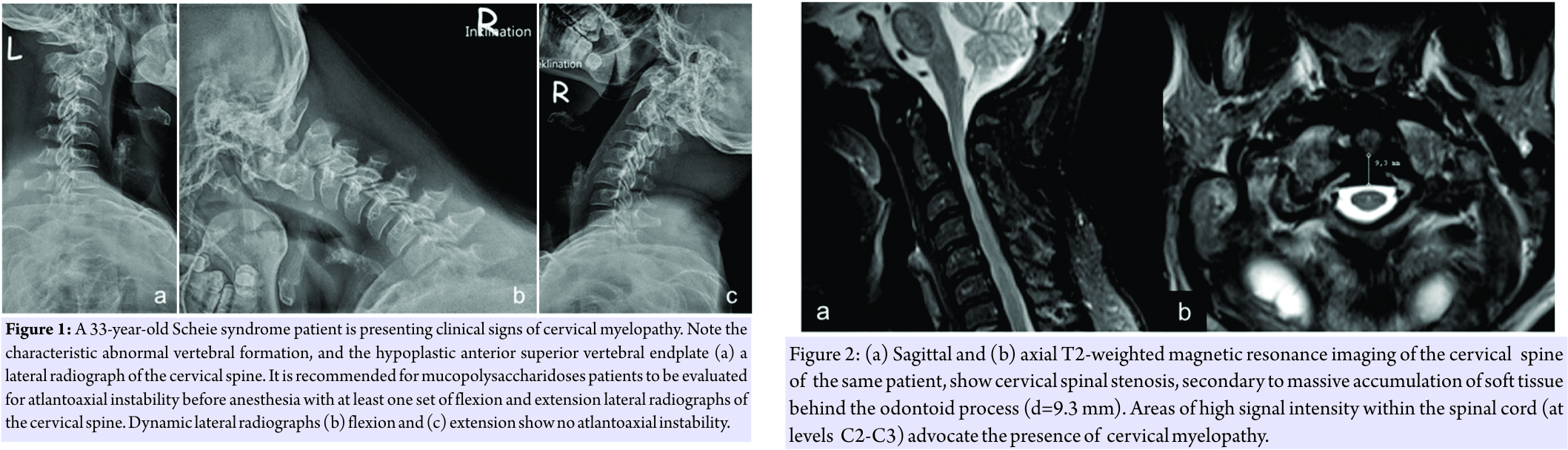
Discussion
Spinal cord compression at the occipitocervical junction is common in MPS patients, while it has historically been postulated to be the most common cause of premature death in persons with MPS type IV [3]. Spinal stenosis results from the accumulation of soft tissue behind the odontoid process and/or from dural thickening [3]. MR imaging can reveal posteriorly prominent intervertebral discs, thickened dura and hypertrophy of the ligamentum flavum [8]. In fact, in the case here presented, a hyperintense soft tissue thickening that was lying posterior to the odontoid process, and a hypertrophic ligamentum flavum resulted to spinal cord compression and myelopathy. As a general rule, in the setting of myelopathy surgery should be offered, especially in a young active patient. However, surgical management in MPS patients constitutes of a great challenge. Firstly Firstly, these patients are at high risk of anaesthetic and surgical complications [2]. Secondly, high level recommendations and high quality evidence that could assist in the decision making process do not exist, owing to the great scarcity of cases; even in the most severe form of the disease (MPS IH), only 3.4% of patients develop cervical spinal stenosis [9]. Nevertheless, in order to offer our patient a relief from symptoms, to reverse the myelopathic symptomatology and to prevent from further deterioration, we decided to proceed with surgery. The index surgery was planned on the basis of the patient’s special characteristics. Serious doubts existed with respect to the bone healing properties of the patient, and considerations were made regarding whether a revision surgery would be necessary in the future. This led us to the decision, to perform a C1-C7 posterior instrumentation with screws only at the most upper (C1/2) and lower (C7) levels. Six months later, however, breakage and loosening of the caudal screws occurred, a failure that was attributed both to the nature of MPS and to the fact that the patient returned to sports soon enough after surgery, though counter advised; without providing for proper fusion to occur, the material fatigue led unavoidably to instrumentation failure. After the revision surgery the patient complied with the given instructions, and even after sustaining a severe head injury, the spinal instrumentation remained intact. The patient throughout the postoperative period remained pain free and ambulatory, and claimed to be rather satisfied with the outcome. The only complaint, consistent at every follow-up, was the limited neck range of motion. Neck stiffness should be expected though, when C1/2 fusion is performed, and it represents more a sequelae rather than a complication.
Conclusions
Cervical myelopathy in Scheie syndrome represents an extremely rare entity and surgical treatment can be mandatory for symptom relief. However, surgery in these patients is rather challenging since it carries high surgical and anesthesia risks. If instrumentation is to be performed, the minimum necessary appliance of hardware is recommended. The nature of the disease may not allow for fusion, causing instrumentation to fail, thereby increasing the surgery-related morbidity. Preoperative planning should further include the management of potential future surgical complications, while patients should be closely followed and thoroughly informed of the possible complications and restrictions that may emerge after surgery.
Clinical Message
Patients with Scheie syndrome may develop cervical myelopathy, consequently requiring surgery. Surgical considerations, however, regarding delayed spinal fusion and the high risks of anesthesia, render surgical management rather challenging. Thorough pre-operative planning and patient compliance are of paramount importance, for satisfactory outcome to be achieved.
References
1. Abelin Genevois K, Garin C, Solla F, Guffon N, Kohler R. Surgical management of thoracolumbar kyphosis in mucopolysaccharidosis type 1 in a reference center. J Inherit Metab Dis 2014;37(1):69-78.
2. Valayannopoulos V, Wijburg FA. Therapy for the mucopolysaccharidoses. Rheumatology (Oxford) 2011;50 Suppl 5:v49-59.
3. White KK, Sousa T. Mucopolysaccharide disorders in orthopaedic surgery. J Am Acad Orthop Surg 2013;21(1):12-22.
4. D’Aco K, Underhill L, Rangachari L, Arn P, Cox GF, Giugliani R, Okuyama T, Wijburg F, Kaplan P. Diagnosis and treatment trends in mucopolysaccharidosis I: findings from the MPS I Registry. Eur J Pediatr 2012;171(6):911-9.
5. Baehner F, Schmiedeskamp C, Krummenauer F, Miebach E, Bajbouj M, Whybra C, Kohlschutter A, Kampmann C, Beck M. Cumulative incidence rates of the mucopolysaccharidoses in Germany. J Inherit Metab Dis 2005;28(6):1011-7.
6. Moore D, Connock MJ, Wraith E, Lavery C. The prevalence of and survival in Mucopolysaccharidosis I: Hurler, Hurler-Scheie and Scheie syndromes in the UK. Orphanet J Rare Dis 2008;3:24.
7. Vijay S, Wraith JE. Clinical presentation and follow-up of patients with the attenuated phenotype of mucopolysaccharidosis type I. Acta paediatr 2005;94(7):872-7.
8. White KK, Harmatz P. Orthopedic management of mucopolysaccharide disease. J Pediatr Rehabil Med 2010;3(1):47-56.
9. van der Linden MH, Kruyt MC, Sakkers RJ, de Koning TJ, Oner FC, Castelein RM. Orthopaedic management of Hurler’s disease after hematopoietic stem cell transplantation: a systematic review. J Inherit Metab Dis 2011;34(3):657-69.
 |
 |
 |
 |
| Dr. Farzam Vazifehdan | Dr. Vasilios G Karantzoulis | Dr. Robert Ebner | Dr. Vasilios G Igoumenou |
| How to Cite This Article: Vazifehdan F, Karantzoulis VG, Ebner R, Igoumenou VG. A Unique Case of Cervical Myelopathy in an Adult Patient with Scheie Syndrome. Journal of Orthopaedic Case Reports 2017 Nov-Dec : 7(6):Page 27-30 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




