[box type=”bio”] Learning Points for this Article: [/box]
We reported 2 rare cases with chronic AARF with rotatory Oc-C1 subluxation and facet deformity of Oc-C1 joint, and orthopedic surgeons should pay attention to pathological changes not only in C1–C2 joint but also in Oc–C1 joint.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 59-63| Masafumi Kashii, Kenta Masuhara,Takashi Kaito, Motoki Iwasaki. DOI: 10.13107/jocr.2250-0685.950
Authors: Masafumi Kashii [1, 2], Kenta Masuhara [2],Takashi Kaito [2], Motoki Iwasaki [2]
[1] Department of Orthopedic Surgery, Toyonaka Municipal Hospital, 4-14-1 Shibaharacho, Toyonaka, Osaka, Japan,
[2] Department of Orthopedic Surgery, Osaka University Graduate School of Medicine, 2-2 Yamadaoka, Suita, Osaka, Japan.
Address for correspondence:
Dr. Masafumi Kashii, Department of Orthopedic Surgery, Toyonaka Municipal Hospital, 4-14-1 Shibaharacho, Toyonaka, Osaka 560-8565, Japan.
E-mail: mkashii-osk@umin.ac.jp
Abstract
Introduction: The relationship between the morphometry of atlantoaxial joint and chronic atlantoaxial rotatory fixation (AARF) is well known, but disorders in the atlanto-occipital joint in chronic AARF are not fully elucidated. The authors report two rare cases of secondary deformities in the atlanto-occipital joint in chronic AARF.
Case Reports: Two patients with chronic AARF were treated with closed manipulation, skull traction and halo-vest immobilization. Clinical outcomes and radiographs were reviewed retrospectively, focusing on pathological changes in the atlanto-occipital joint using multiplanar reconstruction computed tomography and three-dimensional computed tomography images. Case 1 (12-year-old girl) had rotatory subluxation with a superior facet deformity of the atlas in the atlanto-occipital joint before the initiation of treatment. After a series of conservative treatments, both atlantoaxial and atlanto-occipital rotatory fixation could not be reduced, and both the superior facet deformity of the atlas and osteoarthritic changes in the atlanto-occipital developed. She was monitored without surgery because the disorder progressed to the spontaneous fusion of the occipital bone to the axis. Case 2 (13-year-old boy) had rotatory subluxation without facet deformity of the atlas in the atlanto-occipital joint before the initiation of treatment. However, both the superior facet deformity of the atlas and osteoarthritic changes in the atlanto-occipital developed over time, and both atlantoaxial and atlanto-occipital rotatory fixation could not be reduced after a series of conservative treatments. He still had severe neck pain and severely restricted neck mobility and underwent spinal fusion.
Conclusion: Atlanto-occipital rotatory subluxation and facet deformity in the atlanto-occipital joint may occur after prolonged AARF. It is necessary to pay attention to pathological changes not only in the atlantoaxial joint but also in the atlanto-occipital joint, when orthopedic surgeons treat patients with AARF.
Keywords: Atlantoaxial rotatory fixation, atlanto-occipital joint, rotatory subluxation, facet deformity.
Introduction
Atlantoaxial rotatory fixation (AARF) is a rotatory dislocation or subluxation of the atlantoaxial (C1–C2) joint in children [1]. In general, acute AARF resolves either spontaneously or by conservative treatment [1, 2]. However, sometimes AARF is resistant to conservative treatment if the definitive diagnosis is delayed and acute AARF becomes chronic [3, 4, 5, 6]. Ishii et al. observed the morphometry of C1–C2 joint using three-dimensional computed tomography (3D CT) imaging in patients with chronic AARF [7]. Deformity of the superior facet of the axis (C2) and >20° of lateral inclination of the atlas observed on 3D CT are known factors in the progression to intractable AARF [7]. Occipito AARF (OAARF) is thought to be an extremely rare and intractable condition involving fixed rotational subluxation of the atlas (C1) for both the occipital bone (Oc) and C2; there are only 7 reports about cases of OAARF in the literature [8, 9, 10, 11, 12, 13, 14]. However, there is a possibility that disorders of the atlanto-occipital (Oc–C1) joint in patients with AARF are neglected. Using conventional CT images, Ono et al. have already pointed out that the compensatory rotation of Oc for C1 and hypermobility between Oc and C1 may develop in chronic AARF [3]. Pang and Li reported significantly increased rotation of Oc on C1 in chronic AARF [6]. They suggest that most of the compensatory alteration in Oc–C1 laxity takes place sometime after prolonged C1–C2 fixation for 3 months [6]. Until now, disorders in the Oc–C1 joint in chronic AARF have not been fully elucidated because disorders in the craniocervical lesion are difficult to evaluate with plain radiographs, conventional CT, and magnetic resonance imaging. There are no reports to investigate the morphology of Oc–C1 joint with rotatory subluxation in detail. In the present report, we first describe two rare cases of chronic AARF with rotatory subluxation and secondary facet deformities in Oc–C1 joint.
Case Reports
Case 1
A 12-year-old girl presented with neck pain and torticollis after having spent a lot of time playing video games with her neck in the flexion position. Her condition was diagnosed as AARF, and she underwent intermittent neck traction, but her symptoms did not decrease. The time elapsed from symptom onset to first presentation at our hospital was 6 months. During the physical examination, her neck was in the neutral position, and she had neck pain on motion and restricted neck mobility with no neurological deficits.
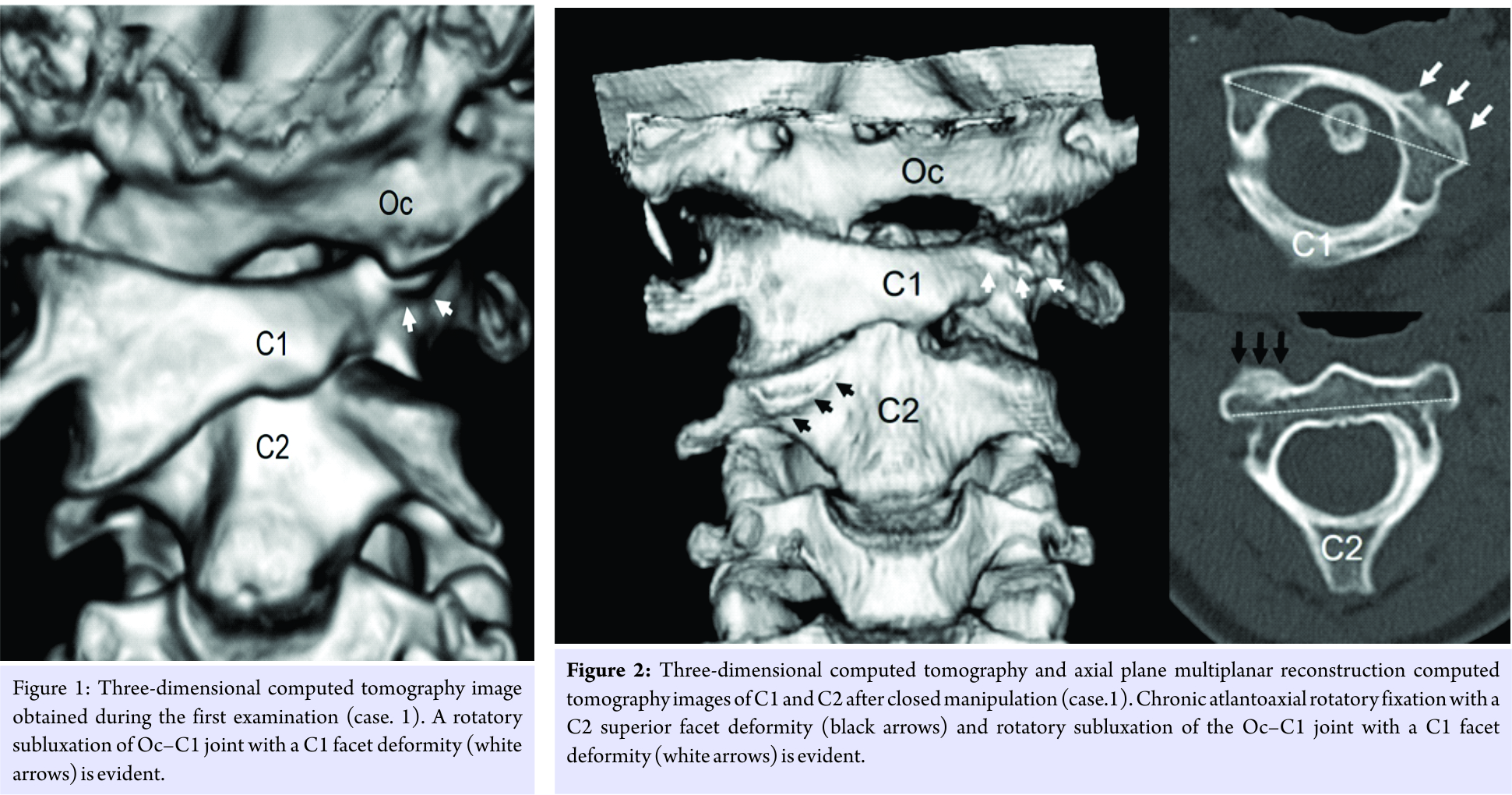
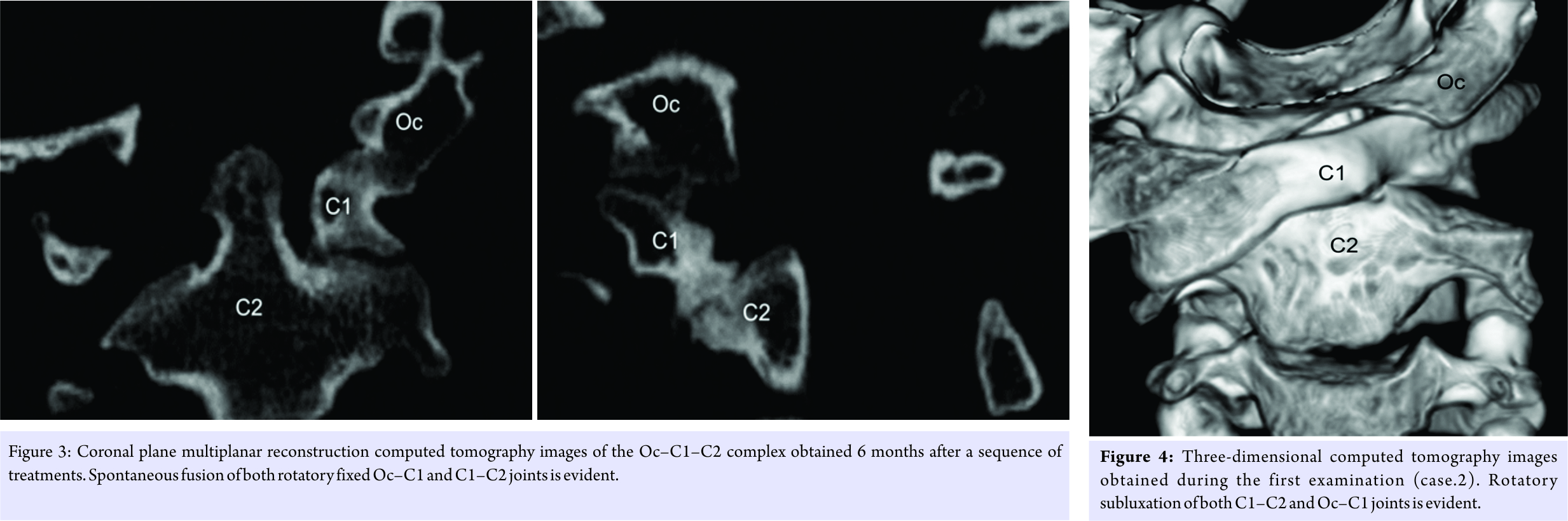
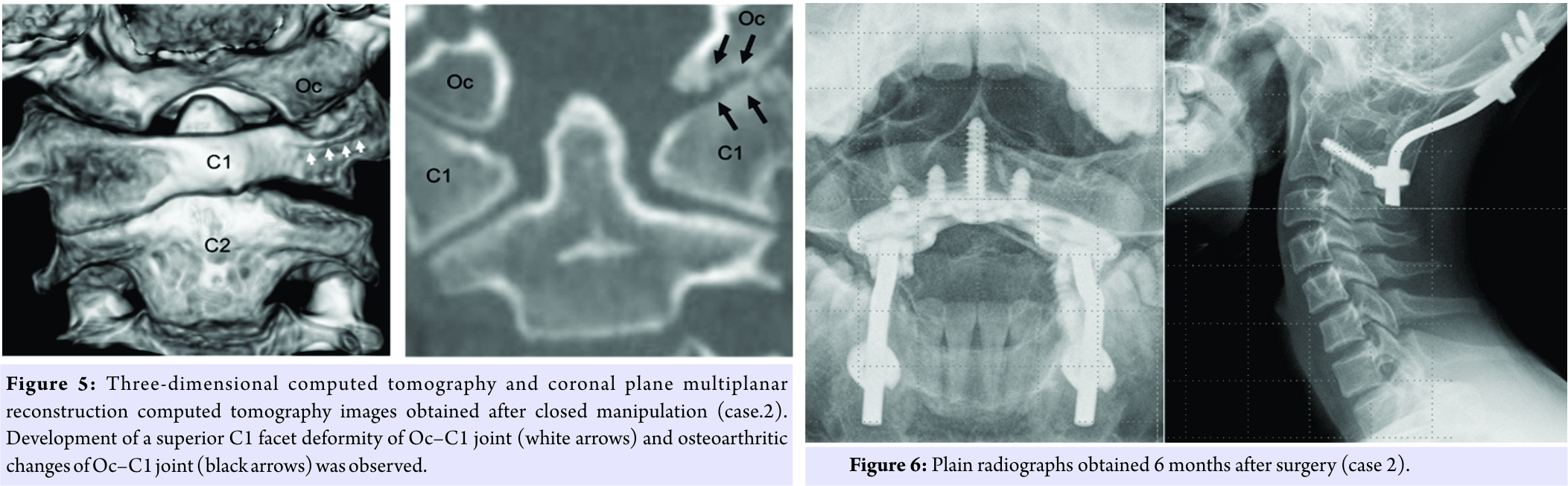
She had fielding Type Ⅲ AARF, and 3D CT images revealed that C1 was turned to the left and slightly bent to the right against C2. On 3D CT images, rotatory subluxation in both C1-2 (C1 rotational angle for C2: 58°) and Oc–C1 joint (Oc rotational angle for C1: 36°) with a C1 superior facet deformity was observed (Fig. 1). At the first visit, treatment options were discussed with her family. Options of surgical reduction and fusion or closed manipulation and halo immobilization were discussed, and the family chose the latter. She underwent closed manipulation and immobilization based on remodeling therapy advocated by Ishii et al. [5]. First, she was fitted with a halo ring under general anesthesia, and she underwent careful closed manipulation. Cervical range of motion (ROM) was found, under general anesthesia, not to be limited. After closed manipulation, 3D CT and multiplanar reconstruction (MPR) CT images revealed that AARF with a C2 superior facet deformity remained and both rotatory subluxation with a C1 superior facet deformity and osteoarthritic changes in the Oc–C1 joint were observed (Fig. 2). As successful reduction could not be confirmed, patients underwent continuous skull traction for 2 weeks. After skull traction, halo-vest immobilization was performed for 8 weeks. Although closed manipulation, continuous skull traction, and halo-vest immobilization were performed, the Oc rotational angle for C1 remained 34° and AARF with Oc–C1 rotatory subluxation was not reduced. After a series of treatments, the girl’s neck pain gradually diminished and she reported only a slight limitation of cervical ROM. Treatment options were discussed with her family, and we decided to monitor her without surgery. MPR CT images at 6 months after treatment revealed spontaneous fusion of both rotatory fixed Oc–C1 and C1–C2 joints (Fig. 3). 30 months later, she had only a small restriction of neck motion.
Case 2
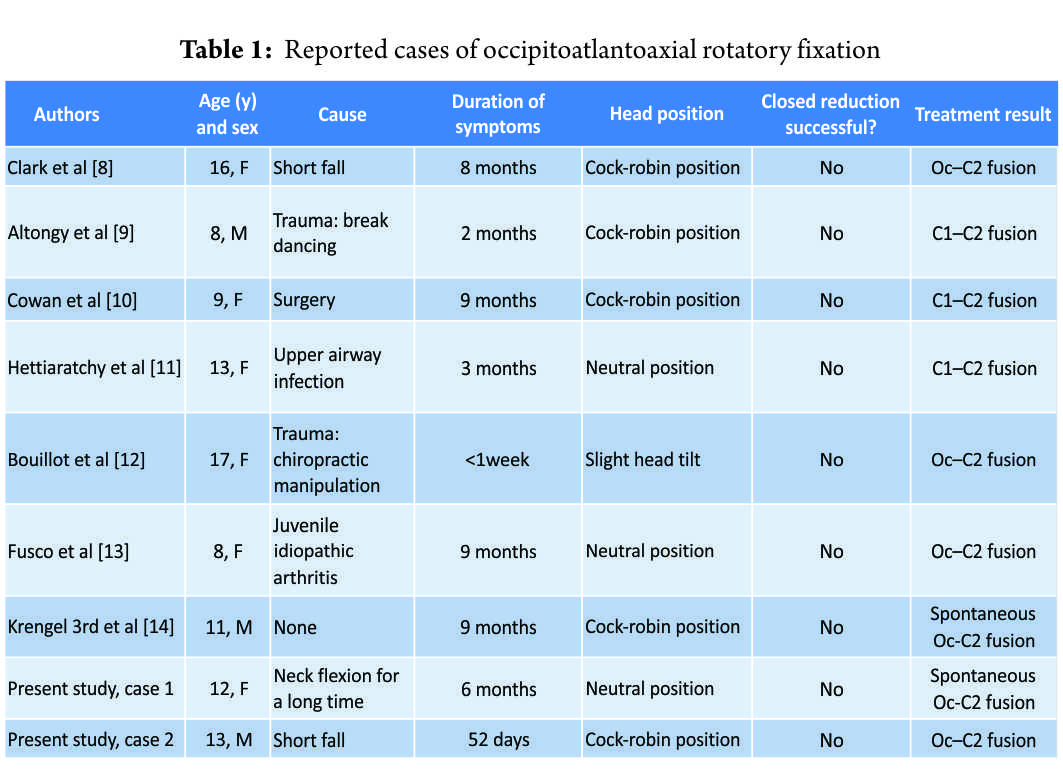
After a shortfall while playing football, a 13-year-old boy sustained a clavicle fracture and had concurrent neck pain and torticollis. Cervical plain radiographs obtained at an orthopedic clinic did not find AARF. His symptoms continued, and eventually, AARF was diagnosed at another orthopedic clinic. The elapsed time from symptom onset to the first presentation at our hospital was 52 days. During the physical examination, his neck was in the “cock robin” position, and he had severe pain on motion and severely restricted neck mobility with no neurological deficits. He had fielding Type I AARF, and both C1–C2 rotatory subluxation (C1 rotational angle for C2: 46°) and Oc–C1 rotatory subluxation (occipital rotational angle for C1 was 35°) were evident on 3D-CT images (Fig. 4). On MPR CT images, deformity of the superior C1 facet and osteoarthritic changes in the Oc–C1 joint was not observed before the initiation of treatment. He also had no obvious congenital morphometric anomaly such as Down syndrome and Klippel-Feil syndrome. Just like case 1, treatment options were discussed with his family, and the family chose the closed manipulation and halo immobilization. He was fitted with a halo ring under general anesthesia, and he underwent careful closed manipulation. The patient underwent halo-vest immobilization with his neck in the neutral position for 6 weeks. Afterward, he had less of a “cock robin” posture, but he still had severe neck pain and severely restricted neck motion. On 3D CT images, it was apparent that Oc–C1 rotatory subluxation (occipital rotational angle for C1: 19°) and AARF (C1 rotational angle for C2: 23°) remained and that deformity of the superior C1 facet and osteoarthritic changes in the Oc–C1 joint had developed (Fig. 5). He underwent closed manipulation again, and then, continuous skull traction for 2 weeks. However, reduction of AARF with Oc–C1 rotatory subluxation was not achieved, and he still had severe neck pain and severely restricted neck mobility. He experienced a great deal of limitation of his activities of daily living because of severe neck pain; therefore, we performed the surgery. His family hoped to preserve the motion of Oc-C1, and we first attempted the intraoperative reduction of C1-C2 joint by releasing C1-C2 joint contracture and inserting a C1 lateral mass screw. After the exposure of C1 and C2, we found the highly developed venous plexus between C1 and C2 and massive bleeding that is difficult to control (intraoperative blood loss: 1520 ml). As a result, he underwent Oc-C2 fusion surgery. 6 months later, complete joint fusion had been achieved (Fig. 6). 3 years later, he experienced no limitation of his activities of daily living and had only a small restriction of neck motion.
Discussion
As a result of treatment with remodeling therapy for chronic AARF, we encountered 2 cases of irreducible AARF. In case 1, chronic AARF could not be reduced, and the disorder progressed to spontaneous fusion of the Oc–C1–C2 complex. In case 2, although symptom duration was <3 months, AARF with both rotatory subluxation and progressive facet deformity of Oc–C1 joint could not be reduced. We first describe pathological changes in the Oc–C1 joint with rotatory subluxation in patients with chronic AARF. To the best of our knowledge, there are only 7 previous reports of OAARF [8, 9, 10, 11, 12, 13, 14] (Table 1).
In 6 cases of OAARF, spinal fusion was performed [8, 9, 10, 11, 12, 13]. Treatment results of closed manipulation and external fixation in OAARF are poorer than in chronic AARF without Oc–C1 rotatory subluxation [8, 9, 10, 11, 12, 13]. The pathogenesis of OAARF can be explained by two theories: (1) That AARF develops after upper airway infection or trauma and that compensatory Oc–C1 joint subluxation develops after prolonged AARF over time, and (2) that both Oc–C1 joint and C1–C2 joint subluxations develop simultaneously and are induced by a high-energy injury. Several studies support the first theory as the main cause of OAARF [3, 6]. Pang and Li reported significantly increased rotation of Oc on C1 in chronic AARF [6]. In their study, the mean Oc–C1 rotational angle was 5° in 12 patients with acute AARF, 9.1° in 7 patients with subacute AARF (for 1–3 months), and 31.2° in 10 patients with chronic AARF (for >3 months ). There were extreme differences in the Oc–C1 rotatory angle between the chronic AARF group and both the acute and subacute AARF groups (P < 0.0000001). Reports of OAARF have also described head positions ranging from neutral (3 previous reports and our case 1), to a slight cock-robin position, to a pronounced cock-robin position [8, 9, 10, 11, 12, 13, 14]. In case 1, her neutral neck position was explained by the complete compensatory rotation of Oc for C1. Fusco et al. persisted that pediatric neurosurgeons should always be aware of possible occipitocervical instability while evaluating AARF, particularly in the presence of a neutral head position [13]. Sugiura et al. accurately measured in vivo 3D kinematics of the upper cervical spine in rheumatoid arthritis during head rotation, and they elucidated the relationships between the contracture of the C1–C2 facet and segmental rotational motion in the Oc–C1–C2 complex [15]. Their results suggest that joint contracture at the C1–C2 joint by the destruction of the articular facet promotes a compensatory increase in rotational motion at the Oc–C1 joint. In case 1, there had been no trauma, the time elapsed from symptom onset to treatment initiation was about 6 months, and compensatory Oc–C1 joint rotatory subluxation might have been induced by prolonged chronic AARF. In case 2, with the patient experienced a shortfall, the time elapsed from symptom onset to treatment initiation was relatively short (52 days), and there was little possibility that compensatory changes in the Oc–C1 joint developed. Oc and C1 form the biaxial condyloid joint, which is tightly connected by the anterior and posterior atlanto-occipital membranes, and the anatomical morphology of the Oc–C1 joint strongly restricts the rotational movement of Oc–C1 [16]. In case 2, it was quite unlikely that subluxation of Oc–C1 could easily develop, and there was the possibility that the Oc–C1 subluxation might be related to the congenital morphometric anomaly of Oc–C1 such as condylar hypoplasia. Regarding pathological changes in the Oc–C1 joint in chronic AARF, we speculate that a misaligned Oc–C1 joint may induce a C1 superior facet deformity to persistent vertical loading, causing osteoarthritic changes, decreasing instability of the Oc-C1-C2 complex, and finally, leading to bony fusion of the Oc–C1–C2 complex. Ishii et al. reported the existence of the C2 facet deformity in chronic AARF, and they postulated that the C2 facet deformity may be derived from a secondary change due to persistent vertical loading on the misaligned facet joint [7]. In addition, they confirmed that the C2 facet deformity was remodeled after closed manipulation [7]. In surgery for OAARF, there is no consensus regarding the fusion area [8, 9, 10, 11, 12, 13]. Researchers have reported that C1–C2 fusion was performed in 3 cases [9, 10, 11] and Oc–C2 fusion was performed in 3 cases [8, 12, 13]. Some researchers reported that the Oc–C1 joint rotatory deformity was the compensatory change resulting in C1–C2 joint deformity, and they performed C1–C2 posterior fusion to preserve the motion of Oc–C1 [9, 10, 11]. They predicted a post-operative decrease in the compensatory change but gave no description of it. In addition, they have not yet reported on long-term results. In case 2, we selected Oc–C2 fusion because there is a possibility that severe neck pain will remain with osteoarthritic changes in the remaining Oc–C1 joint. Another reason for choosing that procedure was an unmovable dislocated atlas that made it impossible to insert a C1 lateral-mass screw during surgery. Long-term results of Oc–C2 fusion for children are unknown, just as they are for C1–C2 fusion surgery, and there is a serious problem to overcome: Cervical ROM is more restricted in Oc–C2 fusion than in C1–C2 fusion. In surgery for OAARF, there is no consensus regarding the fusion area, but the presence or absence of Oc–C1 pathological changes may be of some help to determine the appropriate area for spinal fusion.
Conclusion
In this paper, the authors reported two rare cases with chronic AARF with rotatory Oc–C1 subluxation and facet deformity of Oc–C1 joint. Both rotatory subluxation and osteoarthritic changes in Oc–C1 joint may occur subsequent to prolonged AARF. It is necessary for orthopedic surgeons to pay attention to pathological changes not only in C1–C2 joint but also in Oc–C1 joint.
Clinical Message
We experienced two rare cases with chronic AARF with both rotatory subluxation and facet deformity in the Oc–C1 joint, and AARF could not be reduced. Osteoarthritic changes of Oc-C1 may occur subsequent to prolonged AARF and may be an intractable factor in chronic AARF. We advocate that surgeons use MPR CT and 3D CT images to assess pathological changes not only in the C1–C2 joint but also in the Oc–C1 joint.
References
1. Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am 1977;59:37-44.
2. Subach BR, McLaughlin MR, Albright AL, Pollack IF. Current management of pediatric atlantoaxial rotatory subluxation. Spine (Phila Pa 1976) 1998;23:2174-9.
3. Ono K, Yonenobu K, Fuji T, Okada K. Atlantoaxial rotatory fixation. Radiographic study of its mechanism. Spine (Phila Pa 1976) 1985;10:602-8.
4. Crossman JE, David K, Hayward R, Crockard HA. Open reduction of pediatric atlantoaxial rotatory fixation: Long-term outcome study with functional measurements. J Neurosurg 2004;100 3 Suppl:235-40.
5. Ishii K, Toyama Y, Nakamura M, Chiba K, Matsumoto M. Management of chronic atlantoaxial rotatory fixation. Spine (Phila Pa 1976) 2012;37:E278-85.
6. Pang D, Li V. Atlantoaxial rotatory fixation: Part 3-a prospective study of the clinical manifestation, diagnosis, management, and outcome of children with alantoaxial rotatory fixation. Neurosurgery 2005;57:954-72.
7. Ishii K, Chiba K, Maruiwa H, Nakamura M, Matsumoto M, Toyama Y. Pathognomonic radiological signs for predicting prognosis in patients with chronic atlantoaxial rotatory fixation. J Neurosurg Spine 2006;5:385-91.
8. Clark CR, Kathol MH, Walsh T, el-Khoury GY. Atlantoaxial rotatory fixation with compensatory counter occipitoatlantal subluxation. A case report. Spine (Phila Pa 1976) 1986;11:1048-50.
9. Altongy JF, Fielding JW. Combined atlanto-axial and occipito-atlantal rotatory subluxation. A case report. J Bone Joint Surg Am 1990;72:923-6.
10. Cowan IA, Inglis GS. Atlanto-axial rotatory fixation: Improved demonstration using spiral CT. Australas Radiol 1996;40:119-24.
11. Hettiaratchy S, Ning C, Sabin I. Nontraumatic atlanto-occipital and atlantoaxial rotatory subluxation: Case report. Neurosurgery 1998;43:162-4.
12. Bouillot P, Fuentes S, Dufour H, Manera L, Grisoli F. Imaging features in combined atlantoaxial and occipitoatlantal rotatory subluxation: A rare entity. Case report. J Neurosurg 1999;90 2 Suppl:258-60.
13. Fusco MR, Hankinson TC, Rozzelle CJ. Combined occipitoatlantoaxial rotatory fixation. J Neurosurg Pediatr 2011;8:198-204.
14. Krengel WF 3rd, Kim PH, Wiater B. Spontaneous ankylosis of occiput to C2 following closed traction and halo treatment of atlantoaxial rotary fixation. Global Spine J 2015;5:233-8.
15. Sugiura T, Nagamoto Y, Iwasaki M, Kashii M, Kaito T, Murase T, et al. In vivo 3D kinematics of the upper cervical spine during head rotation in rheumatoid arthritis. J Neurosurg Spine 2014;20:404-10.
16. Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation: Part 1-normal occipital condyle-C1 interval in 89 children. Neurosurgery 2007;61:514-21.
 |
 |
 |
 |
| Dr. Masafumi Kashii | Dr. Kenta Masuhara | Dr. Takashi Kaito | Dr. Motoki Iwasaki |
| How to Cite This Article: Kashii M, Masuhara K, Kaito T, Iwasaki M. Rotatory Subluxation and Facet Deformity in the Atlanto-occipital Joint in Patients with Chronic Atlantoaxial Rotatory Fixation: Two Case Reports. Journal of Orthopaedic Case Reports 2017 Nov-Dec; 7(6): 59-63 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com