[box type=”bio”] Learning Points for this Article: [/box]
The described technique of Arthroscopic fixation of avulsed tibial spine in children by non absorbable suture is simple in clinical practice and provides predictable outcome.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 80-84| Skand Sinha, Durgashankar Meena, Ananta K Naik, M Selvamari, Rajendra K Arya. DOI: 10.13107/jocr.2250-0685.960
Authors: Skand Sinha [1], Durgashankar Meena [1], Ananta K Naik [1], M Selvamari [1], Rajendra K Arya [1]
[1] Department of Orthopaedics, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India
Address of Correspondence:
Dr. Skand Sinha,
Department of Orthopaedics, PGIMER, Dr. Ram Manohar Lohia Hospital, New Delhi – 110 001, India.
E-mail: skandsinha@gmail.com
Abstract
Introduction: Tibial spine avulsion fracture is more frequent in children than adults. Various methods of fixation have been mentioned, but concern remains about crossing the tibial physis. We present a technique of arthroscopic fixation with non-absorbable suture.
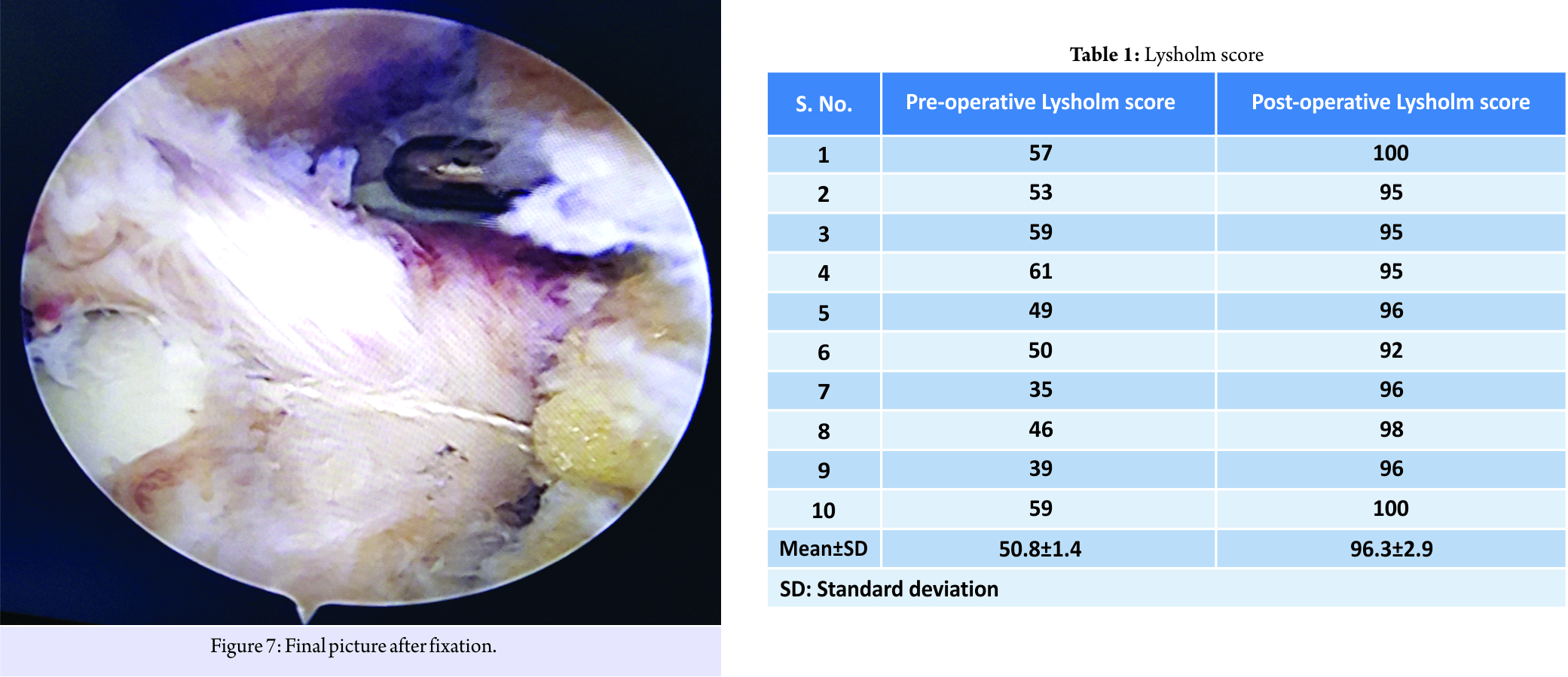
Case Report: A total of 10 skeletally immature patients with tibial spine avulsion of Meyers and McKeever Type 2 and 3 were included in the study. The knee was arthroscopically cleared of hematoma. The avulsed tibial insertion of anterior cruciate ligament was reduced and held in place with tibial guide. By drilling guide wire through the tibia, reduced fragment, a fiber wire was passed. The avulsed fragment was tied on a suture post on tibia. Outcome was evaluated radiologically and clinically (Lysholm score, pivot shift, and KT 1000) at 12 months after surgery. All cases attained full range of motion, stable knee and could return to previous level of activity. The mean pre-operative Lysholm score of 50.8 ± 1.4 (35–59) improved to 96.3 ± 2.9 (92–100). The mean pre-operative anterior translation of tibia (measured by KT 1000) of 7.6 ± 1.26 improved significantly to mean of 3.3 ± 0.82 mm after surgery.
Conclusion: The presented technique of arthroscopic fixation of avulsed tibial spine is a simple technique that provides reproducible results. It also offers cost-effective, secure fixation.
Keywords: Tibial, spine, fixation.
Introduction
Avulsion of tibial spine is more frequent in pediatric age group than adults [1]. Greater elasticity of anterior cruciate ligament (ACL) fibers and incompletely ossified tibial spine predisposes to this injury [2, 3]. Conservative management has limited role and requires strict monitoring as it commonly leads to loss of reduction and ligament laxity [4]. Surgical intervention is recommended for Meyers and McKeever Type 2 and Type 3 fractures [5]. There are various methods described for arthroscopic/open fixation of tibial spine such as cannulated screw [6, 7], suture anchor [8], and absorbable/non-absorbable pull out suture [9, 10, 11, 12]. Seon et al. [13] found no significant difference in clinical outcome after screw or suture fixation. Bong et al. [14] reported fiber wire fixation to be superior to cannulated cancellous screw fixation. Biomechanical comparison of two single-armed number 2 ethibond sutures, bioabsorbable nails, single bioabsorbable screw, or a single metal screw on immature bovine knees yielded similar results [15]. Recent literature suggests that arthroscopic suture fixation provides stable fixation, early mobilization with good functional outcome [16, 17, 18, 19]. However with any suture fixation technique, there are issues like keeping the small fragment fixed in its position while drilling, suture passage, and changeover of instruments. We present a simple technique of arthroscopic suture fixation of avulsed tibial spine with fiber wire that simplifies these issues.
Case Report
A total of 10 skeletally immature patients with tibial spine avulsion of Meyers and McKeever Type 2 and 3 were subsequently included in the study. X-ray and magnetic resonance imaging of knee were used to document injuries.
Surgical technique
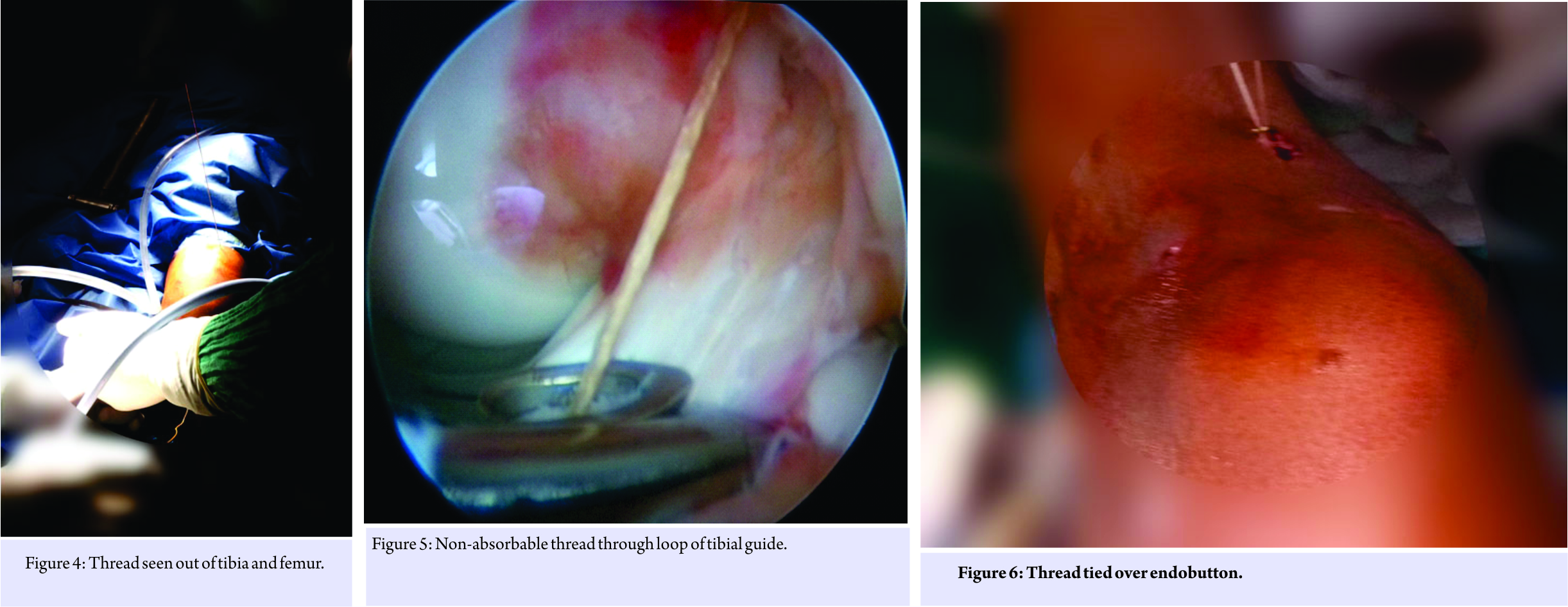
Under regional anesthesia, the patient is positioned supine. After preparation, lower limb is placed over side post with the knee in 90o flexion. Arthroscopy is performed using anterolateral and anteromedial portals. The anterolateral portal is made slightly proximal and lateral to facilitate viewing anterior aspect of knee. Joint is cleared of hematoma and debris. Any interposed tissue between avulsed fragment and fracture crater or intermeniscal ligament is released. It is important to clear the anterior aspect of avulsed fragment (Fig. 1). Reduction of avulsed fragment is done with a probe. The ACL tibial guide (Arthrex) is introduced through anteromedial portal (Fig. 2). Hook of tibial guide (looped) placed on avulsed fragment at the posterolateral extent of fragment. The tibial guide is used to compress avulsed fragment in its crater. A 2.4 mm guide wire (with eye at trailing end) is inserted 1 cm medial to tibial tuberosity through tibial guide (Fig. 3). The guide wire is passed through tibia, avulsed fragment, and lateral side of intercondylar notch with absolute care that there is no movement at the knee while passing the wire through femur. The guide wire is delivered out of skin on anterolateral side of thigh. The eyed side of guide wire is kept outside tibia. Care is taken to pass the guide wire distal to femoral physis by increasing flexion beyond 90° and checked on image intensifier. A fiber wire passed into eye of guide wire. The guide wire is delivered out from femoral side by gentle taps on T-handle fixed to the leading end of wire from femoral side. The free end fiber wire remains outside tibia (Fig. 4). Now, tibial side of free end of fiber wire is secured with artery forceps and the guide wire is completely pulled. This results in one end of fiber wire outside tibia and the other end outside femur. With the loop of tibial guide, the femoral side of fiber wire is retrieved (Fig. 5) from anteromedial portal. Same steps are repeated to pass another fiber wire anteromedial to previous one as far as possible. Free end of threads outside anteromedial portal is knotted. One of the free ends of fiber wire outside tibia is pulled to bring the knot outside tibia and knot is cut. With traction on free ends of the fiber wire outside tibia, the avulsed fragment is snugly seated in the crater and the free ends are tied over a suture disc/endobutton over tibia (Fig. 6). The final intra-articular reduction is checked (Fig. 7). Wound was closed and long leg splint was applied.
All cases were mobilized with support and protected weight-bearing was allowed from next day of surgery. Isometric hamstring and quadriceps strengthening exercise were started with brace on. Brace was used for 3 weeks. Range of motion exercises was initiated after 3 weeks. Lysholm score (table 1) and pivot shift test were used to evaluate clinical outcome. Objective measurement of anterior translation of tibia (ATT) was done by KT1000 pre-operative and at 12 months in every patient. Radiological evaluation was done by true anteroposterior, lateral radiograph of knee in the post-operative period and 6 months. All cases were followed up for 12 months.
There were 10 cases between 9 and 15 years of age with a mean of 12.1 ± 1.9. Nine subjects were male and one was female. The time interval from injury to surgery was in range of 5–23 days with a mean of 10.7 ± 6 days. The most common mode of injury was fall during playing. Pre-operative Lachman and pivot shift test was positive in all cases. The pre-operative ATT measured by KT 1000 that was in range of 6–9 mm with a mean of 7.6 ± 1.26. It improved to 2–5 mm with a mean of 3.3 ± 0.82 mm. The improvement in ATT was statistically significant. The ATT of operated knee was nearly the same as that of the normal opposite knee, which was in range of 1–5 mm with a mean of 3.1 ± 1.1. There was no statistically significant difference of ATT between operated and normal knee. The mean pre-operative Lysholm score of 50.8 ± 1.4 (35–59) improved to 96.3 ± 2.9 (92–100). Pivot shift test was negative in all cases. Radiologically, all cases had union of avulsed tibial spine in reduced position at follow up and all could return to their previous level of activity.
Discussion
Surgical intervention for tibial avulsion of ACL in children is fraught with potential risk of growth disturbance [20]. However, a secure fixation is essential for early mobilization and full range of motion. There are different techniques described for suture fixation of avulsed fragment [21]. Drilling of pilot hole and passage of suture is integral to all methods. Keeping the avulsed fragment stable in its bed during drilling and suture passage is of paramount importance, but it is also a challenge, especially if the fragment is small. There is risk of further fragmentation of small avulsed fragment by multiple drilling. The task of keeping the avulsed fragment reduced and stable in its crater while drilling and passage of suture through the avulsed fragment is simplified by this technique. We use the ACL tibial guide (Arthrex, which has ovoid area with the hook) to keep the avulsed fragment reduced in its crater. The large contact area of guide keeps the fragment firmly in place till it is fixed. The tibial guide is used as avulsed fragment stabilizer, guide as well as suture retriever. This technique does not require any changeover of instruments in surgeon’s hand as required in routine suture pull out techniques, for maintaining reduction of fragment, drilling, suture passage, and retrieval, as all these tasks are completed as a single step, making this technique simpler. The only precaution, we exercise, is to pass the guide wire passes through non-articular area of lateral femoral condyle that is away from physis. Other difference with routine suture pull out technique is the passage of wire through anterolateral soft tissue sleeve of thigh. However, we found it not to be of any clinical significance in terms of clinical outcome. Wire passage for tunnel creation through distal femur is also reported in ACL reconstruction in children with no adverse outcome [20]. As fragment reduction, drilling and suture passage is performed in one go, the tourniquet and operative time are short. Although most authors stress on the importance of avoidance of crossing the epiphyseal plate [22], it has been observed that drill holes of approximately 3% of the cross-sectional area of the physes cause no growth disturbance [23]. However, if this is 7% or more then only it leads to growth disturbance [24]. McConkey et al. [20] observed that tunnel size of 6–7 mm that is perpendicular to the physis, minimizes the damage to the growth plate. Shea et al. [25] found it safe even drilling a tunnel of 9 mm in anatomic ACLR with open physis. During the procedure, we ensure that the crossing of tibial physis is as perpendicular to physis as possible while drilling. Only two drill holes were created that too with guide wires only. Hence, the effective breach of tibial physis would be <3%. Union of avulsed fragment in all cases, achievement of stability and significant improvement in Lysholm score depict the effectiveness of this technique. All the cases could return to previous level of activity. The described technique is simple, reproducible, and very cost-effective.
Conclusion
The presented technique of arthroscopic fixation of avulsed tibial spine with non-absorbable suture is a simple technique that provides reproducible secure fixation and satisfactory clinical outcome. It is also cost-effective.
Clinical Message
Arthroscopic fixation is recommended for avulsion fractures of tibial spine except Meyers and McKeever Type 1. Non-absorbable suture fixation provides stable fixation so that early mobilization with good functional outcome can be achieved.
References
1. 1. Zionts L. Fractures and dislocations about the knee. In: Green NE, Swiontkowski MR, editors. Skeletal Trauma in Children. Philadelphia, PA: WB Saunders; 2009. p. 452-5.
2. Wiley JJ, Baxter MP. Tibial spine fractures in children. Clin Orthop Rel Res 1990;255:54-60.
3. Noyes FR, DeLucas JL, Torvik PJ. Biomechanics of anterior cruciate ligament failure: An analysis of strain-rate sensitivity and mechanisms of failure in primates. J Bone Joint Surg Am 1974;56:236-53.
4. McLennan JG. Lessons learned after second-look arthroscopy in Type III fractures of the tibial spine. J Pediatr Orthop 1995;15:59-62.
5. Sapre V, Bagaria V. Tibial Spine Avulsion Fractures: Current Concepts and Technical Note on Arthroscopic Techniques Used in Management of These Injuries. InTech, DOI: 10.5772/54967; 2013.
6. Van Loon T, Marti RK. A fracture of the intercondylar eminence of the tibial treated by arthroscopic fixation. Arthroscopy 1991; 7:385-8.
7. Reynders P, Reynders K, Broos P. Pediatric and adolescent tibial eminence fractures: Arthroscopic cannulated screw fixation. J Trauma 2002;53:49-54.
8. Vega JR, Irribarra LA, Baar AK, Iñiguez M, Salgado M, Gana N, et al. Arthroscopic fixation of displaced tibial eminence fractures: A new growth plate-sparing method. Arthroscopy 2008;24:1239-43.
9. Ahn JH, Yoo JC. Clinical outcome of arthroscopic reduction and suture for displaced acute and chronic tibial spine fractures. Knee Surg Sports Traumatol Arthrosc 2005;13:116-21.
10. Lehman RA Jr. Murphy KP, Machen MS, Kuklo TR. Modified arthroscopic suture fixation of a displaced tibial eminence fracture. Arthroscopy 2003;19:E6.
11. Su WR, Wang PH, Wang HN, Lin CJ. A simple, modified arthroscopic suture fixation of avulsion fracture of the tibial intercondylar eminence in children. J Pediatr Orthop B 2011;20:17-21.
12. Medlar RG, Jansson KA. Arthroscopic treatment of fractures of the tibial spine. Arthroscopy 1995;11:328-31.
13. Seon JK, Park SJ, Lee KB, Gadikota HR, Kozanek M, Oh LS, et al. A clinical comparison of screw and suture fixation of anterior cruciate ligament tibial avulsion fractures. Am J Sports Med 2009;37:2334-9.
14. Bong MR, Romero A, Kubiak E, Iesaka K, Heywood CS, Kummer F, et al. Suture versus screw fixation of displaced tibial eminence fractures: A biomechanical comparison. Arthroscopy 2005;21:1172-6.
15. Mahar AT, Duncan D, Oka R, Lowry A, Gillingham B, Chambers H, et al. Biomechanical comparison of four different fixation techniques for pediatric tibial eminence avulsion fractures. J Pediatr Orthop 2008;28:159-62.
16. Kocher MS, Foreman ES, Micheli LJ. Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy 2003;19:1085-90.
17. Owens BD, Crane GK, Plante T, Busconi BD. Treatment of Type III tibial intercondylar eminence fractures in skeletally immature athletes. Am J Orthop (Belle Mead NJ) 2003;32:103-5.
18. Mah JY, Adili A, Otsuka NY, Ogilvie R. Follow-up study of arthroscopic reduction and fixation of Type III tibial-eminence fractures. J Pediatr Orthop 1998;18:475-7.
19. Tudisco C, Giovarruscio R, Febo A, Savarese E, Bisicchia S. Intercondylar eminence avulsion fracture in children: Long-term follow-up of 14 cases at the end of skeletal growth. J Pediatr Orthop B 2010;19:403-8.
20. McConkey MO, Bonasia DE, Amendola A. Pediatric anterior cruciate ligament reconstruction. Curr Rev Musculoskelete Med 2011;4:37-44.
21. Yuan Y, Huang X, Zhang Y, Wang Z. Treatment of tibial eminence fractures with arthroscopic suture fixation technique: A retrospective study. Int J Clin Exp Med 2015;8:13797-803.
22. Rockwood CA, Wilkins KE, King RE. Fractures In Children. Philadelphia, PA: Lippincott; 1984. p. 940-6.
23. Garces GL, Mugica-Garay I, Lopez-Goncalves Coviella N, Guerardo E. Growth-plate modifications after drilling. J Pediatr Orthop 1994;14:225-8.
24. Coyle C, Jagernauth S, Ramachandran M. Tibial eminence fractures in the paediatric population: A systematic review. J Child Orthop 2014;8:149-59.
25. Shea KG, Belzer J, Apel PJ, Nilsson K, Grimm NL, Pfeiffer RP, et al. Volumetric injury of the physis during single-bundle anterior cruciate ligament reconstruction in children: A 3-dimensional study using magnetic resonance imaging. Arthroscopy 2009;25:1415-22.
 |
 |
 |
 |
 |
| Dr. Skand Sinha | Dr. Durgashankar Meena |
Dr. Ananta K Naik | Dr. M Selvamari | Dr. Rajendra K Arya |
| How to Cite This Article: Sinha S, Meena DS, Naik AK, Selvamari M, Arya RK. Arthroscopic Fixation of Tibial Spine Avulsion in Skeletally Immature: The Technique. Journal of Orthopaedic Case Reports 2017 Nov-Dec; 7(6): 80-84 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com