[box type=”bio”] Learning Point for this Article: [/box]
Gleno-humeral dislocation must be looked for in every patient of fracture shaft humerus.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 36-38| Rajiv Kapila, Bhanu Awasthi, Manik Sehgal, Avinash Sharma, Preeti Kapila. DOI: 10.13107/jocr.2250-0685.988
Authors: Rajiv Kapila[1], Bhanu Awasthi[1], Manik Sehgal[1], Avinash Sharma[2], Preeti Kapila[3]
[1]Department of Orthopaedics, Dr. R.P.G.M.C, Kangra at Tanda, Himachal Pradesh, India.
[2]Department of Pediatrics, Dr. R.P.G.M.C, Kangra at Tanda, Himachal Pradesh, India.
[3]Department of Radiodiagnosis, Dr. R.P.G.M.C, Kangra at Tanda, Himachal Pradesh, India.
Address of Correspondence:
Dr. Rajiv Kapila,
Set No- 42, Block-G, Type-4, Dr. R.P.G.M.C, Kangra at Tanda – 176 001, Himachal Pradesh, India.
E-mail: drrajivkapila@yahoo.co.in
Abstract
Introduction: Combination of Anterior Glenohumeral Dislocation with Ipsilateral Shaft humerus fracture is a rare co-occurrence and guidelines of its management are lacking. It is a rare opportunity for orthopaedic surgeon to observe simultaneous shoulder dislocation with ipsilateral humeral shaft fracture. There has been a total of around twenty cases reported since 1940.
Case presentation: A case of elderly female with medical co-morbidities who sustained this injury while working in wheat farms. She presented with complaints of pain and swelling in right arm with inability to move right arm. She was diagnosed as a case of ipsilateral fracture of proximal humerus with anterior glenohumeral dislocation. She was successfully treated with open reduction and internal fixation (ORIF) for fracture shaft humerus with long proximal humerus locking plate, because of proximal extension of long oblique fracture line using standard delto-pectoral approach with anterolateral distal extension of surgical approach after visualising radial nerve. Following fixation of shaft, close reduction was carried out for anterior shoulder dislocation under image intensifier. Patient was put on regular physiotherapy and follow up at 4 weekly interval for a period of 3 months and subsequently bimonthly interval upto 1 year. Patient achieved near normal and pain-free range of motion at 1 year.
Conclusion: Anterior Glenohumeral Dislocation with Ipsilateral Shaft humerus fracture, can be easily missed clinically in obese patients. Close reduction is possible after attaining adequate lever arm by fixing shaft followed by attempt to reduce dislocation. Meticulous surgical technique coupled with dedicated and supervised physiotherapy is essential to bring out good functional outcome.
Keywords: Glenohumeral dislocation, Humeral shaft fracture, Co-Occurrence.
Introduction
Shoulder joint is a ball and socket joint with humeral head being ball and glenoid cavity of scapula, being socket and this joint has wide range of mobility. It is the most frequent joint to get dislocated with incidence of 8.2 to 23.9 per 10000 persons per year [1]. It is a rare opportunity for orthopaedician to observe simultaneous shoulder dislocation with ipsilateral humeral shaft fracture. There has been a total of around twenty cases reported since 1940 [2-6]. We here present a case which is unique because of fracture of proximal third of shaft of humerus with ipsilateral anterior shoulder dislocation in elderly obese female with medical co-morbidities.
Case report
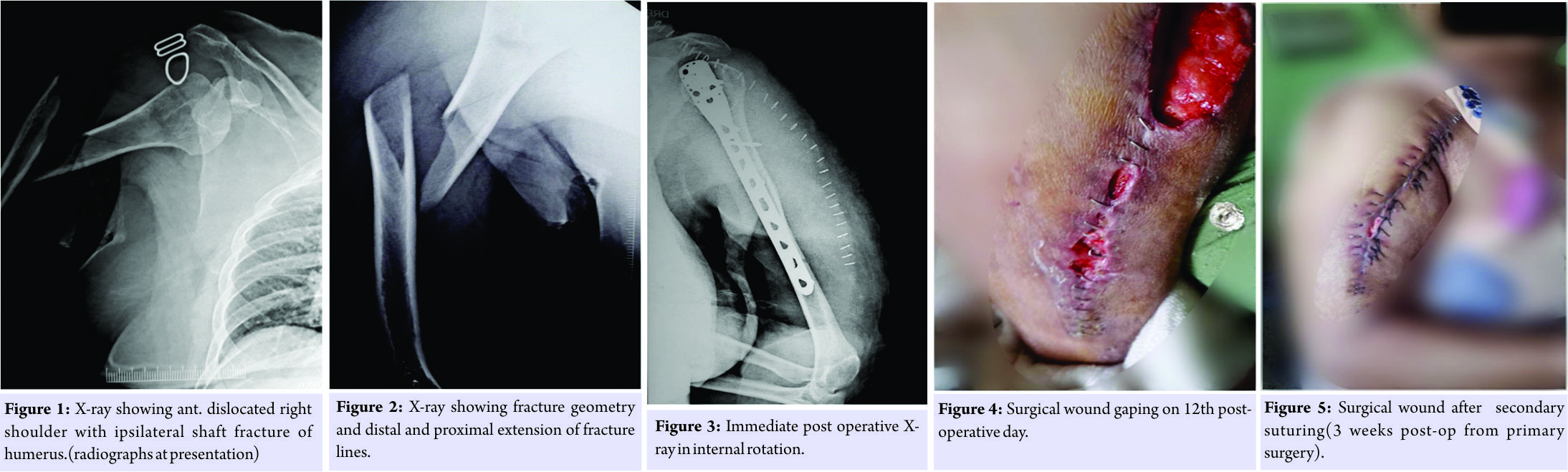
A 62 year old female presented to the emergency department after 6 hours of sustaining injury due to a fall while working in wheat farms with chief complaints of pain, swelling and inability to use her right upper dominant extremity. Gentle clinical examination was done and a clinical possibility of fracture shaft humerus was made. Patient was also evaluated for associated vascular and neurological involvement and any obvious nerve/vascular involvement was ruled out clinically. Radiological investigations revealed fracture of proximal 3rd of shaft of right humerus with ipsilateral anterior dislocation of shoulder (fig.1 and fig .2). Gentle immediate close reduction was attempted for both fracture and dislocation but without any success.
Surgical intervention was planned and pre-operative investigations revealed hypertension with elevated blood sugar levels (fasting bloosugar:180 mg% and glycosylated haemoglobin of 6.8%),medical consultation including that of cardiology and pulmonology was sought and patient was operated on 5th post admission day with open reduction and internal fixation (ORIF) for fracture shaft humerus with long proximal humerus locking plate because of proximal extension of long oblique fracture line through standard delto-pectoral approach with anterolateral distal extension of surgical approach. Radial nerve was identified and protected. Following fixation of shaft, close reduction was carried out for anterior shoulder dislocation. Reduction was found satisfactory under image intensifier and further on post- operative x-rays (fig 3).
On 4th post operative day, serous discharge was noted in surgical wound and full gaping/dehiscence of surgical wound was noticed on 12th post operative day (fig. 4), for which secondary suturing was done. Patient was discharged on 21st post op day following primary surgery. She continued to improve on regular follow-up and was instructed for gradual progressive active range of motion exercises (fig 5 and fig 6). At 1 year follow-up, there was satisfactory bone union (fig 7. And fig.8) with painless, nearly full and free range of motion with patient returning to her pre-injury activities (fig .9 and fig.10).
Discussion
Simultaneous occurrence of humeral shaft fracture with ipsilateral shoulder dislocation is an uncommon injury. Only about 20 such cases has been reported in literature as per pub med search done on the date of writing this article [3-6]. Significant amount of force is required in order to have fracture and dislocation in same limb. Axial loading forces transfer energy to the shaft and further into shoulder resulting in simultaneous injuries [7, 8]. Some authors have suggested dislocation due to indirect forces and fracture shaft due to direct impact [6, 9]. In our patient, we believe that possible mechanism of injury was fall on outstretched hand leading to transmission of force along shaft to shoulder. Shoulder dislocation was not suspected clinically in our patient as patient was not co-operative during clinical examination owing to marked pain and also had morbid obesity which impaired judgement of shoulder contour. Various case reports show that major obstacle in achieving close reduction is lack of adequate lever arm, which demands surgical intervention to fix the shaft followed by closed reduction [10-12]. After thorough review of the literature (3-6) open reduction using standard deltopectoral approach was planned and shaft fragment was fixed with long plate and then closed reduction of joint was done. Regular follow-up along with appropriate physiotherapy helped in achieving good functional outcome.
Conclusion
Shoulder dislocation with associated ipsilateral fracture shaft humerus, can be easily missed clinically in obese patient .Close reduction is possible after attaining adequate lever arm by fixing shaft followed by attempt to reduce dislocation.
Clinical Message
Although combination of anterior glenohumeral dislocation with ipsilateral fracture shaft humerus injury is unusual, it is treatable with acceptable clinical results. Fixation of shaft fragment and then utilizing this lever arm for closed reduction of joint offers good option for treatment.
References
1. Kwon YW ,Kulwicki KJ ,Zuckerman JD. Glenohumeral joint subluxations, dislocations and instability. In : Bucholz R W, Heckman JD, Court- Brown CM, et al, eds. Rockwood and Green’s fractures in adults[M]. 7th ed. Pheiladelphia: Lippincott Williams & Wilkins, 2010: 1165-209
2. Winderman A: Dislocation of the shoulder with fracture of the shaft of the humerus. Bull HospJt Dis Orthop Inst. 1940, 1: 23-25.
3. Flint JH, Carlyle LM, Christiansen CC, Nepola JV. Case report and literature review anterior shoulder dislocation with three-part proximal humerus fracture and humeral shaft fracture. Iowa Orthop J. 2009;29:105–13.
4. Chen CH, Lai PL, Niu CC, Chen WJ, Shih CH. Simultaneous anterior dislocation of shoulder and fracture of the ipsilateral humeral shaft. IntOrthop. 1998;22:65–7.
5. Chirputkar K, Basappa P, McLean I, Nimon G. Posterior dislocation of the shoulder with ipsilateral humeral shaft fracture: A case report and review of literature. ActaOrthop Belg. 2006;72:219–22.
6. Kontakis GM, Galankis IA, Steripoulous KA: Dislocation of the shoulder and ipsilateral fracture of the humeral shaft: case reports and literature review. J Trauma.1995, 39: 990-992.
7. Barquet A, Schimchak M, Carreras O, Leon H, Masliah R: Dislocation of the shoulder with fracture of the ipsilateral shaft of the humerus. Injury.1985, 16: 300-302.
8. Sankaran-Kutty M, Sadat-Ali M. Dislocation of the shoulder with ipsilateral humeral shaft fracture. Arch Orthop Trauma Surg. 1989;108:60–2.
9. J CanosaiAreste. Arch Orthop Trauma Surg 1994. 113 (6), 347-348.
10. Calderone RR, Ghobadi F, McInerney V. Treatment of shoulder dislocation with ipsilateral humeral shaft fracture. Am J Orthop. 1995;24:173–6.
11. Sasashige Y, Kurata T, Masuda Y, Shimono K, Nagata Y. Dislocation of the shoulder joint with ipsilateral humeral shaft fracture: two case reports. Arch Orthop Trauma Surg. 2006;126:562–7.
12. Baker DM. Fracture of the humeral shaft associated with ipsilateral fracture dislocation of the shoulder: report of a case. J Trauma. 1971;11:532–4.
 |
 |
 |
 |
 |
| Dr. Rajiv Kapila | Dr. Bhanu Awasthi | Dr. Manik Sehgal | Dr. Avinash Sharma | Dr. Preeti Kapila |
| How to Cite This Article: Kapila R, Awasthi B, Sehgal B, Sharma A, Kapila P. Anterior Glenohumeral Dislocation with Ipsilateral Shaft Humerus Fracture – A Rare Co-occurrence; Case Report from Hills of North India. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 36-38. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com