[box type=”bio”] Learning Point for this Article: [/box]
FOP is a rare disorder that gradually decreases mobility and, therefore, quality of life. Surgery for bone resection is NOT indicated because the bone will form again in the same place. In case of surgery in these patients, care must always be taken to avoid the activation of new ossifications.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 39-43| Douglas Colmenares-Bonilla, Alejandra Gonzalez-Segoviano. DOI: 10.13107/jocr.2250-0685.990
Authors: Douglas Colmenares-Bonilla[1], Alejandra Gonzalez-Segoviano[2]
[1]Department Pediatric Orthopedic, Hospital Regional de Alta Especialidad del Bajio, Leon, Guanajuato, Mexico.
[2]Fellow in Pediatric Orthopedic Surgery Course, Hospital Regional de Alta Especialidad del Bajio, Leon, Guanajuato, Mexico.
Address of Correspondence:
Dr. Douglas Colmenares-Bonilla, Pediatric Orthopedics Department, Hospital Regional de Alta Especialidad del Bajio, Blvd. Milenio 130, Col San Carlos La Roncha. Leon, Guanajuato, Mexico CP 37670, Mexico.
E-mail: douglas_cb@yahoo.com
Abstract
Introduction: Fibrodysplasia ossificans progressiva (FOP) is the severest disease of ossification in the human. It forms an exoskeleton gradually. This process is started for a nodule that ossifies as days goes by. The initial pathway cannot be stopped unless early immunosuppress management is started very early after the aggression has been received. These aggressions may vary from contusions, viral illnesses, surgery, and other minor trauma.
Because of this process, the FOP patient gradually worsens and decreases its autonomy as described from ability to walk, dress, or even to eat and breathe.
Case Report: An 11-year-old female comes to evaluation for multiple ossifications, which worsen her autonomy and the ability to walk. The last ossification keeps the knee bent at 90° by a bony bridge from the femur to the tibia. To try to walk, it is necessary to flex hip, and ankle, with tilting of the pelvis, with pain and loss of autonomy. Due to the characteristic ossification pattern, FOP is diagnosed and the possibility of surgery to prolong autonomic gait is suggested. The procedure is performed under immunosuppression, and the knee is extended to a position that allows the patient to walk again freely. The steroid management is continued the convenient time to avoid exacerbation of the disease at a distance, and suspend it definitively afterward.
Conclusions: The FOP is adding an exoskeleton and its episodes of exacerbation end in new ossifications that deteriorate the quality of life. Once the ossifications have appeared, it is not possible to stop or reverse the process. Performing an osteotomy to prolong gait is a risky procedure. However, the present study shows that final ossification is expected at the point of resection of the extracted bone and suggests that immunosuppressing the patient could prevent distant exacerbations. The risk-benefit ratio of the procedure may be favourable if it is performed at a quiescent stage of the disease.
Keywords: Osteotomy, ossificans progressiva, surgery, flare up, knee deformity.
Introduction
Fibrodysplasia ossificans progressiva (FOP), also known as progressive ossifying myositis, is the most severe disease related to ossification in humans. Its incidence is estimated to be as low as 1 in 1 million inhabitants, with no predominance of race or sex [1]. Its first manifestations are around the year at 5 years old, and diagnosis can be delayed an average of 5 years since first symptoms [2]. In this condition, there is heterotopic bone formation in the connective tissue, starting with rapidly growing soft tumors toward the stiffness of the near joints, in a proximal-distal direction and from head to toe [3]. It usually begins in the cervical spine, limiting the movement of this segment of the spine and evolves to ossify the scapular waist, to later achieve bony bridges and limit the movement of the pelvic girdle [4], irreversibly affecting mobility and quality of life [5]. The diagnosis is based on radiographic data: Ectopic ossification and skeletal malformations [2 – 4]. Patients are normal at birth, except for brachy symphalangism of big toes [6, 7, 8]. During growth, nodules of fibrous tissue, which is highly inflammatory and painful, develop rapidly, then matured into skeletal bone, thereby mediating progressive and irreversible immobility [2, 3, 5, 6]. A flare-up triggers an entire pathological process that begins with a subcutaneous nodule and a continuous cascade of inflammatory events mediated by cellular hypoxia and tissue edema, concluding in ossification. In the axial skeleton, it starts with nodules, however, in the extremities; it is usually due to diffuse edema. These bone growths are episodic and progressive [7, 9]. The activation of the disease and the appearance of new trauma nodules are described secondary to minor contusions, intramuscular vaccination, mandibular anesthetic blocks, muscular fatigue, and viral diseases such as influenza [1, 2]. Natural history progresses toward complete immobility, leading to total dependence for all activities [10]. The ectopic bone in the mandible (chin on chest deformity) is responsible for severe weight loss and malnutrition, complicated by heart failure and pneumonia due to a rigid rib cage with occlusion of the airway due by cervical deformity [11]. The life expectancy is around 45 years [10, 11]. Mortality is due to respiratory, infectious, and cardiovascular complications [12]. To date, there is research treatment applied during the emergence of new flare-ups, which is showing promising results, changing the path of trauma – ossification, but it is not able to reverse existing ossifications [13].
Objectives
The objective of this study is to describe a school-aged girl patient with this disease in whom the leading cause of functional limitation is the knee bone bridge, which causes tilting of the pelvis, scoliosis, limb shortening, back pain, and inability to walk. It aims to find the best time to perform scheduled surgical management in this condition, with the objective to improve quality of life, trying to avoid trigger an inflammatory response, and thus the activation of a new heterotopic ossification.
Case Report
It is evaluated in the pediatric orthopaedic service an 11-year-old female patient, who does not have any significant family history. The only antecedent to the birth is the varus deformity of the first toe of both feet. From the 5th year of life, it begins with subcutaneous nodules in the lumbosacral region, which rapidly progress to ossification and prevent it from moving the left shoulder. It is submitted to multiple surgeries for resection of nodules, and diagnostic biopsies, however soft tumors reappear and worsen ossifications. He stops going to seek medical evaluations for the fear of continuing the ossifications 2 years later. Throughout the childhood suffers multiple falls with concussions of varied magnitude, as much in the head as in the rest of the body, increasing immobility by the ossifications followed of these blows, worsening the capacity for mobility of scapular waist, cervical spine, and shoulders. She is assessed for disability due to a recent bone bridge that fixes the right knee in 90° flexion, with pelvic tilt and unstructured scoliosis with secondary low back pain. The shortening of the limbs rises to 130 mm, which makes her dependent on transport, dress, and hygiene. Physical examination with weight 30 kg, size 1.36 m. Posture with the left shoulder descent, left dorsal scoliosis, and right lumbar support with the right forefoot. In side view, there is antepulsion of head, neck and shoulders, and semi-flexed hip and knee with right forefoot support (Fig. 1).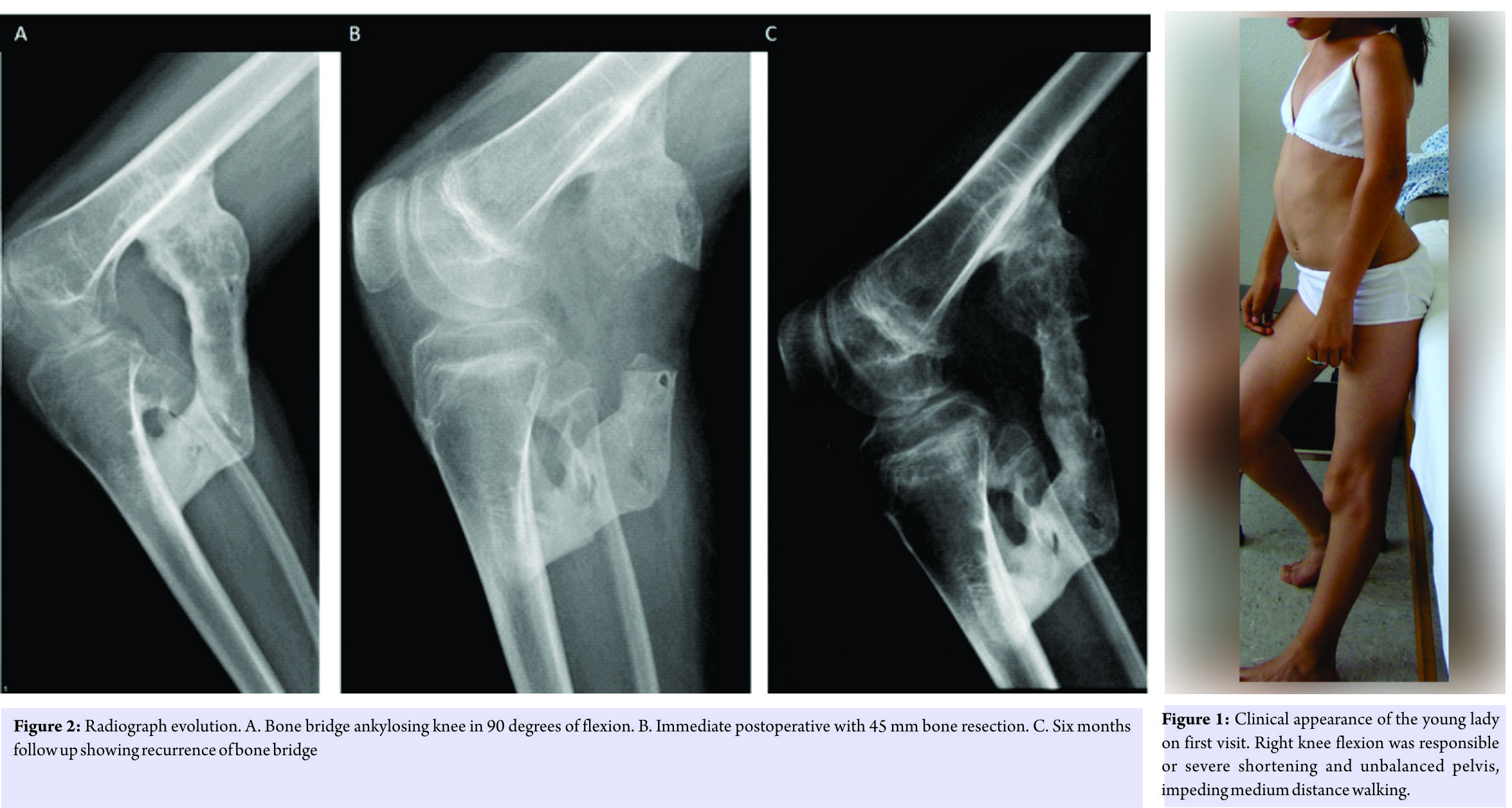
Blood test within normal parameters
On a scheduled basis and with prior wide informed consent to the patient and her caregiver, the procedure of removal of the osseous knee bridge is performed, under the following care: Standardization of erythrocyte sedimentation rate parameters, C-reactive protein and procalcitonin, application of 3 boluses of methylprednisolone (30 mg/kg/day) for 3 days before surgery, and alendronate 10 mg/day uninterrupted for six weeks. Surgical management is performed under regional anesthesia (subarachnoid block) and sedation, without using tourniquet. By blunt dissection, the femoral-tibial bone bridge is freed and a 45 mm segment is removed under fluoroscopic control (Fig. 3). Absorbable suture is used. Mobility of the knee is corroborated under anesthesia obtaining flexion of 120° and almost full extension (Fig. 4). In the immediate postoperative period, a medium compressive bandage is placed, a passive knee mobilizer and intermittent cold therapy are installed to aid in help control. Walking is indicated within the following 12 hours, family assisted.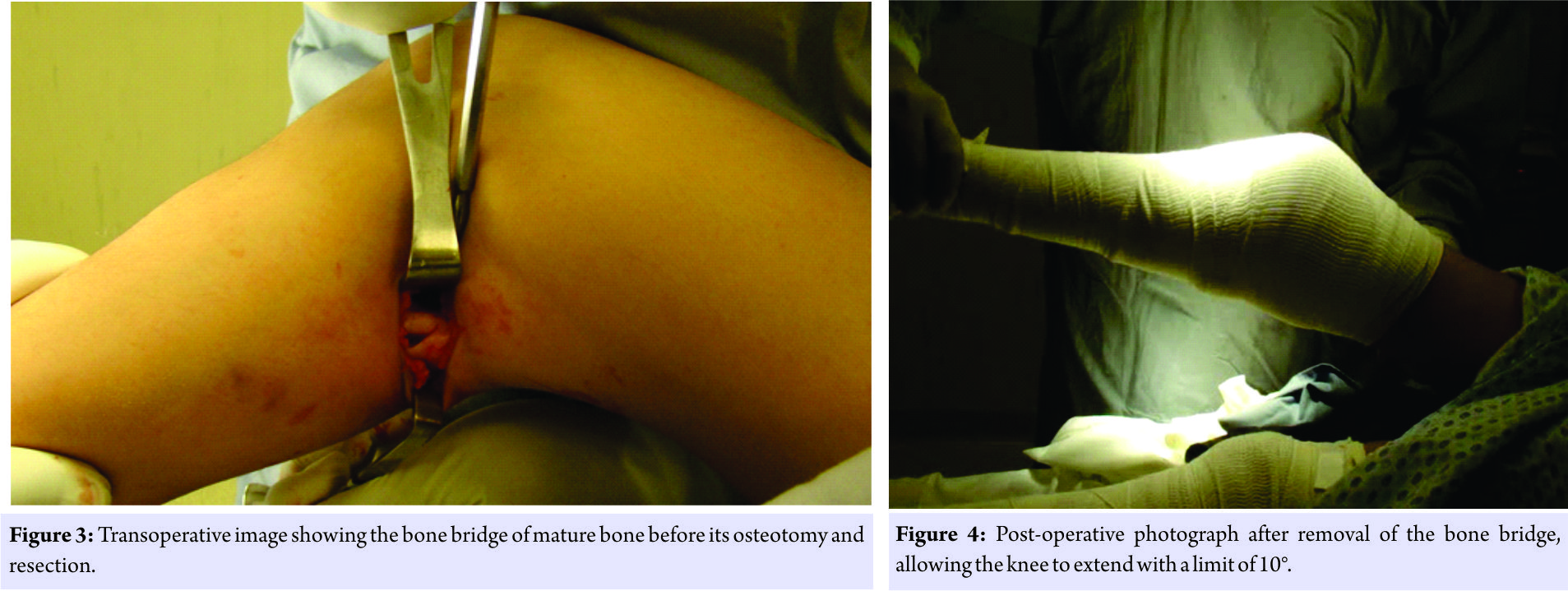
Discussion
Current management for FOP is limited to the prevention of new flare-ups and ossifications, symptomatic management and maintenance of function [13]. Release of contractures or joint restrictions usually leads to new ossification or reactivation of the disease locally or at distance [14]. The location of the ossification will determine the severity of the functional sequelae. It has been described the management of these patients should be only conservative, however, the clinical conditions in which a safe surgery it can be performed are poorly described. Any type of programmed aggression (surgery, trauma) should be performed if possible during a non-active phase of the disease [15], even though it has not been determined which are the laboratory or clinical parameters that signal the onset of these quiescent phases, but with the patient with an unmistakable evidence of not having a flare up or ossifying activity [13 -15]. Having a programmed aggression, provides the opportunity to try to decrease the factors that aggravate the condition and schedule the best time for it. Steroid management has been shown to reduce the possibility of flare-ups secondary to tissue injury [1], so to date it remains the first tool to use following major trauma or surgeries. In the case of the patient is given prior and after surgery.
To the best of our knowledge, there are not enough reports in the literature that show the clear effects of surgeries on the exacerbation of ossification in FOP [11, 12,15]. There is no evidence to suggest that nsaids, COX2 inhibitors, leukotrienes, or plasma cell stabilizers modify the course of the disease. Bone marrow transplantation has not been effective; however, it seems that prolonged immunosuppression may be useful [1, 13]. It is important to emphasize that in these patients, pneumococcal and influenza immunizations, applied only subcutaneously, should be routinely applied.
Conclusion
Performing scheduled surgeries in patients with FOP will always be discussed, and there are many authors against this practice. The rule is ossification relapse, and the only justification for this surgery is the end of prolonging the autonomy time, with the knowledge that the benefit in mobility is only temporary, and at the end, there will be ossification at the place of surgery. FOP patients will sometimes require emergency surgery and, as there is not enough knowledge of the disease, there are no precautions necessary to prevent the onset of the disease. Steroids are, at this time, the basis of prevention for new ossifications, while scientific studies may provide another option. Many of the patients with FOP have undergone surgery procedures throughout their life and, in most cases, the doctors involved are not familiar with the disease or the consequences of the surgery. Before scheduling surgery in patients with FOP, the risk and benefit of the procedure should be evaluated, and the patient and family members decide what is most favorable to the patient. It will be necessary to evaluate in the long term and with a larger number of patients, the safety of a surgical treatment to maintain the patient’s mobility and independence for the longest time.
Clinical Message
Performing an osteotomy in patients with FOP is not recommended due to the high possibility of triggering and activate the disease. However, some patients with FOP will be operated under emergency conditions, without being able to prepare them to reduce the possibility of complications. It is questionable to perform an osteotomy, whose sole purpose would be to prolong autonomy. Each case should be evaluated individually by letting the patient know the risks and benefits of the procedure. After bone bridge resection, re-ossification is a rule.
References
1. Kaplan FS, Pignolo RJ, Shore EM. Granting immunity to FOP and catching heterotopic ossification in the act. Semin Cell Dev Biol 2016;49:30-6.
2. Pignolo RJ, Bedford-Gay C, Liljesthröm M, Durbin-Johnson BP, Shore EM, Rocke DM, et al. The natural history of flare-ups in Fibrodysplasia Ossificans Progressiva (FOP): A comprehensive global assessment. J Bone Miner Res 2016;31:650-6.
3. Al Kaissi A, Kenis V, Ben Ghachem M, Hofstaetter J, Grill F, Ganger R, et al. The diversity of the clinical phenotypes in patients with fibrodysplasia ossificans progressiva. J Clin Med Res 2016;8:246-53.
4. Singh A, Pradhan G, Kumari C, Kapoor S. Early recognition of fibrodysplasia ossificans progressiva-important for the clinician. JNMA J Nepal Med Assoc 2016;54:91-3.
5. Ortiz-Agapito F, Colmenares-Bonilla D. Quality of life of patients with fibrodysplasia ossificans progressiva. J Child Orthop 2015;9:489-93.
6. Towler OW, Shore EM, Xu M, Bamford A, Anderson I, Pignolo RJ, et al. The congenital great toe malformation of fibrodysplasia ossificans progressiva?-A close call. Eur J Med Genet 2017;60:399-402.
7. Sferopoulos NK, Kotakidou R, Petropoulos AS. Myositis ossificans in children: A review. Eur J Orthop Surg Traumatol 2017;27:491-502.
8. Colmenares-Bonilla D, González-Sandoval B. Fibrodisplasia Osificante Progresiva: Informe De Caso Con Diagnóstico Temprano Y Propuesta De Rehabilitación. Acta Ped Mex. 38, 2 2017, 101-107.
9. Kaplan FS, Pignolo RJ, Shore EM. Granting Immunity to FOP and Catching Heterotopic Ossification in the Act. Semin. Cell Dev. Biol. 2016, 49, 30–6.
10. Connor JM, Evans DA. Fibrodysplasia Ossificans Progressiva. The Clinical Features and Natural History of 34 Patients. Bone & Joint Journal 1982.
11. Moore, R. E.; Dormans, J. P.; Drummond, D. S.; Shore, E. M.; Kaplan, F. S.; Auerbach, J. D. Chin-on-Chest Deformity in Patients with Fibrodysplasia Ossificans Progressiva. JBJS Case Connector 2009, 1497–1502.
12. Kaplan, FS; Zasloff, MA; Kitterman, JA; Shore, EM Early Mortality and Cardiorespiratory Failure in Patients with Fibrodysplasia Ossificans Progressiva. J. Bone Joint Surg. Am. 92, 686–691 (2010).
13. Glaser DL, Kaplan FS. Treatment considerations for the management of fibrodysplasia ossificans progressiva. Clin Rev Bone Miner Metab. 2005;3:243–250.
14. Kitterman JA, Kantanie S, Rocke DM, et al. Iatrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics 2005;116:e654-e661.
15. Glaser DL, Rocke DM, Kaplan FS (1998) Catastrophic falls in patients who have fibrodysplasia ossificans progressiva. Clin Orthop Rel Res 346:110–116.
 |
 |
| Dr. Douglas Colmenares-Bonilla | Dr. Alejandra Gonzalez-Segoviano |
| How to Cite This Article: Colmenares-Bonilla D, Gonzalez-Segoviano A. Bone Resection Osteotomy in Fibrodysplasia Ossificans Progressiva. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 39-43 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




