[box type=”bio”] Learning Point for this Article: [/box]
The use of ultrasonic bone curette is easy, safe, and very effective in microendoscopic spine surgery and it helps achieve less invasiveness and ideal decompression, without injuring the nerve root.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 57-60| Masanari Takami, Keiji Nagata, Hiroshi Yamada DOI: 10.13107/jocr.2250-0685.998
Authors: Masanari Takami[1],[2], Keiji Nagata[1], Hiroshi Yamada[2]
[1]Department of Orthopaedic Surgery, Shingu Municipal Medical Center, 18-7 Hachibuse, Shingu, Japan,
[2]Department of Orthopaedic Surgery, Wakayama Medical University, 811-1 Kimiidera, Wakayama, Japan.
Address of Correspondence:
Dr. Masanari Takami,
Department of Orthopaedic Surgery, Shingu Municipal Medical Center,18-7 Hachibuse, Shingu, Japan.
E-mail: maatomo324@gmail.com
Abstract
Introduction: We present a rare case with radiculopathy resulting from intraforaminal stenosis of the lumbar spine due to an ossification lesion. Microendoscopic surgery was chosen because of two strong advantages. One was the ease to reach the nerve foramen and ossification lesion and the other was the non-invasiveness at the posterior supporting structures of the spine. Moreover, an ultrasonic bone curette developed for microendoscopic spine surgery was applied. This is the first detailed case report of microendoscopic surgery using an ultrasonic bone curette for a patient with radiculopathy due to intraforaminal free ossification.
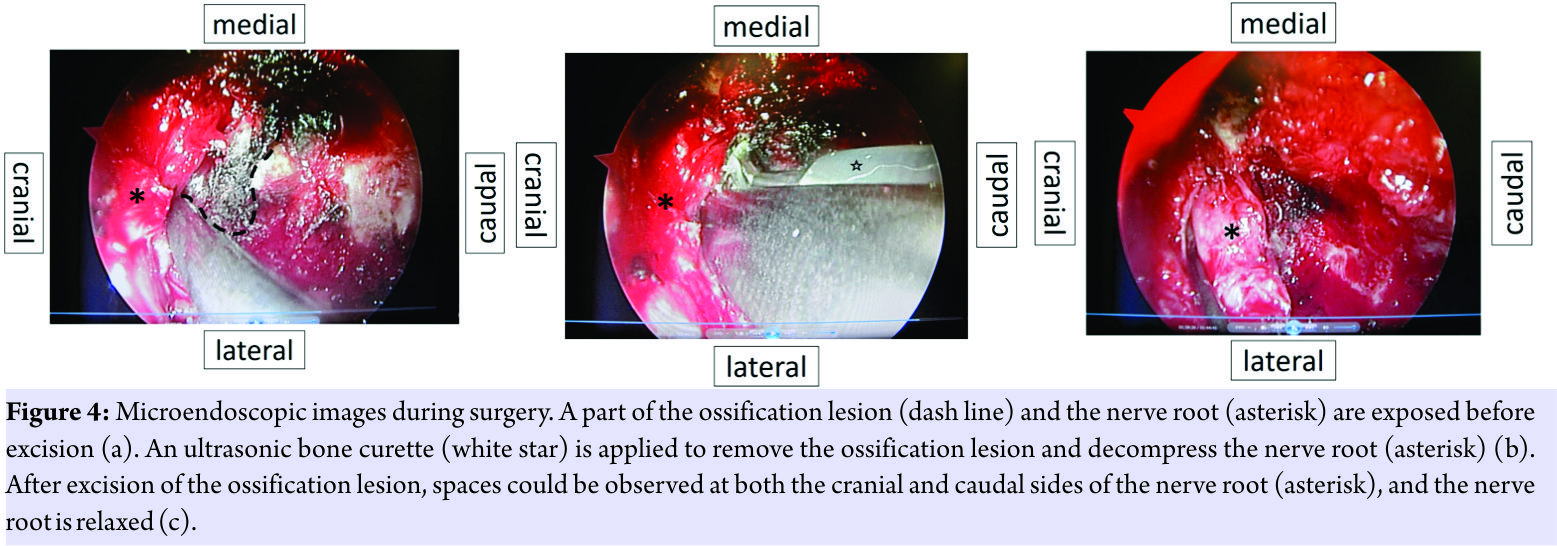
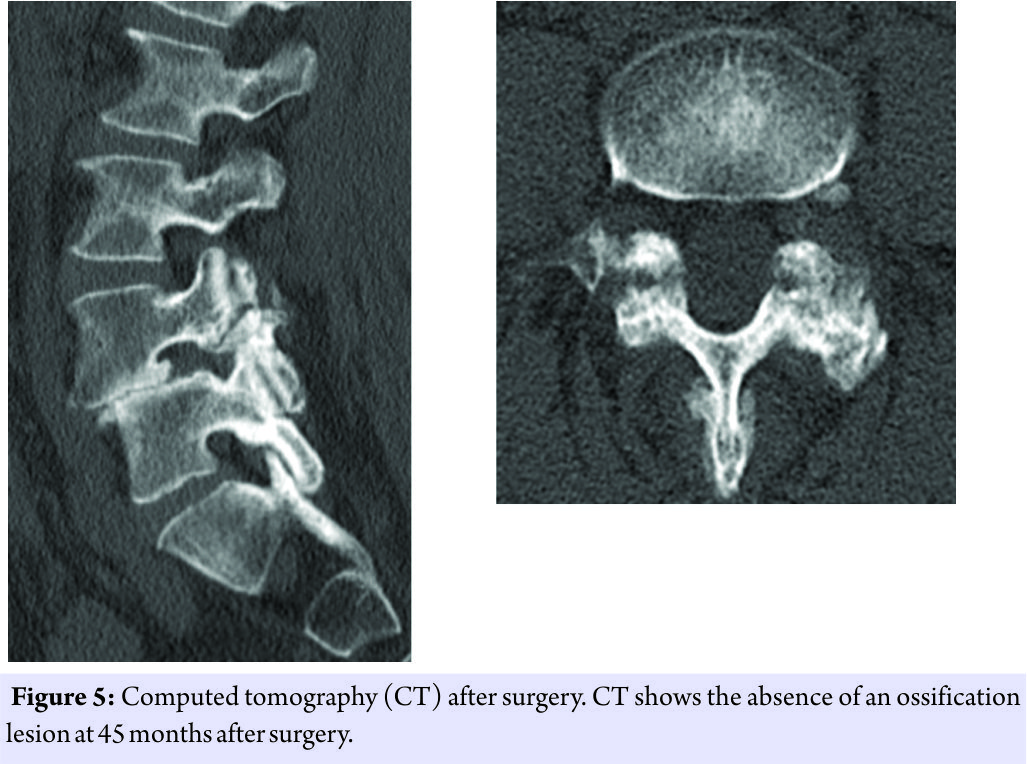
Case Report: A 49-year-old woman born in Japan had complained of severe left leg pain for over 7 months in spite of conservative treatment including selective nerve root block. There was no lumbago, muscle weakness, or loss of sensation in her leg. Plain radiography revealed spondylolytic spondylolisthesis classified as Grade II at L4–L5, but there was no instability on dynamic assessment. Computed tomography (CT) showed a free ossification lesion in the foramen at L4–L5. Considering a diagnosis of left L4 radiculopathy due to the free ossification, ossification resection and nerve decompression were performed with posterior spinal microendoscopic surgery using an ultrasonic bone curette. A tubular retractor was introduced into the extraforaminal zone using Wiltse approach. After a part of the ossification lesion and the nerve root were exposed, an ultrasonic bone curette was applied to remove the ossification mass. After decompression, the nerve root was found to be relaxed. The surgical time was 83 min, and blood loss was 5 g. According to the Japanese Orthopedic Association scoring system, her score improved from 21/29 preoperatively to 29/29 postoperatively, and the full score was maintained at the final observation. Post-operative CT revealed the absence of an ossification lesion.
Conclusions: For a rare case with radiculopathy resulting from intraforaminal stenosis of the lumbar spine due to an ossification lesion, microendoscopic surgery with an ultrasonic bone curette was very effective. The use of ultrasonic bone curette is easy and safe in microendoscopic surgery and it helps achieve less invasiveness and ideal decompression, without injuring the nerve root.
Keywords: Intraforaminal stenosis, microendoscopic spine surgery, ossification lesion, radiculopathy, spondylolytic spondylolisthesis, ultrasonic bone curette.
Introduction
We experienced to treat a patient with intraforaminal stenosis of the lumbar spine due to intraforaminal free ossification. Strategies for the surgical treatment of patients with intraforaminal lesions have been reported [1, 2, 3, 4, 5, 6]. Spinal fusion surgery allows surgeons to reach the intraforaminal space easily; however, this method is invasive. We introduced microendoscopic surgery using an ultrasonic bone curette for the patient. To the best of our knowledge, this is the first detailed case report of microendoscopic surgery using an ultrasonic bone curette.
Case report
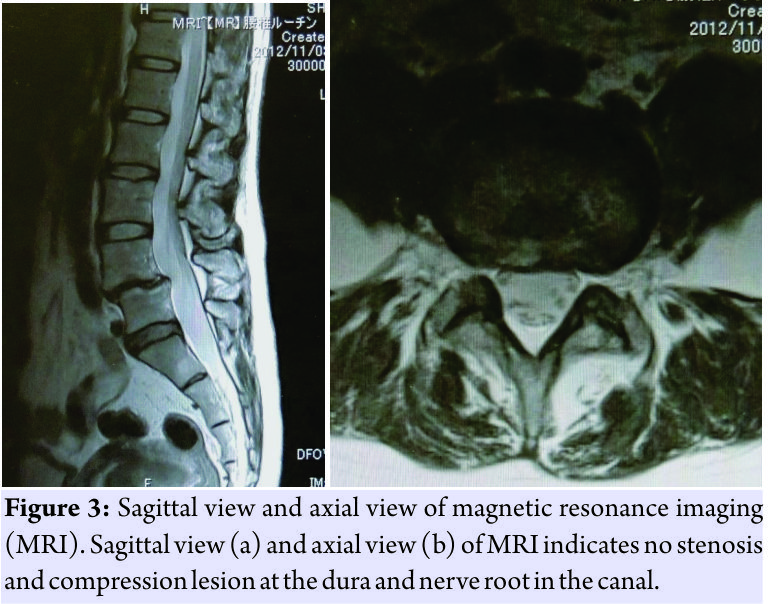
A 49-year-old woman complained of severe left leg pain and could not walk or stand up. She presented with left buttock and anterior thigh pain along the L4 dermatome. There was no lumbago, muscle weakness, or loss of sensation in her leg. The femoral nerve-stretching test was positive on the left side. Plain radiography of the lumbar vertebrae revealed spondylolytic spondylolisthesis at L4–L5, which was classified as Grade IIaccording to Meyerding classification(Fig.1); however, there was no instability on dynamic assessment. Computed tomography (CT) showed a free ossification lesion in the foramen and ossification of the yellow ligament at L4–L5, without a ragged edge (Fig.2).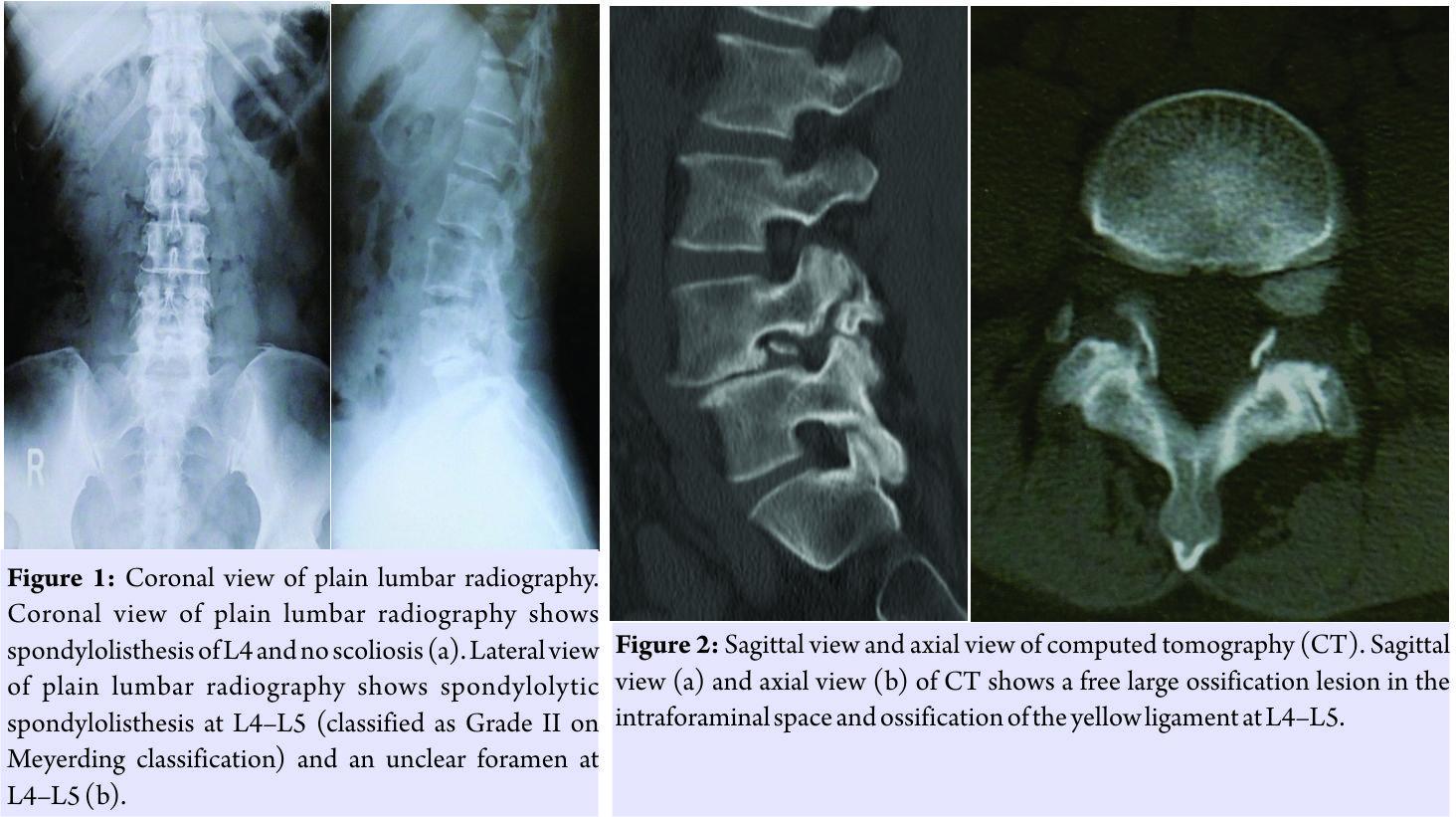
The surgical time was 83min, and blood loss was only 5g. She mentioned that there was no leg symptom immediately after the surgery and could walk without an aid on the next day of the surgery.
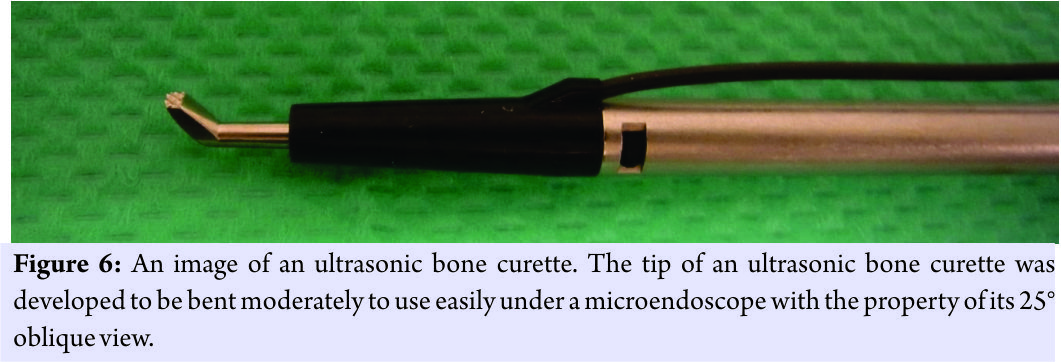
According to the Japanese Orthopedic Association scoring system, her score improved from 21/29 preoperatively to 29/29 postoperatively, and the full score was maintained at the final observation 45 months after the surgery. Post-operative CT revealed the absence of an ossification lesion (Fig. 5) and no lumbar instability.
Discussion
For this ossification lesion, some surgical options could be considered [1, 2, 3, 4, 5, 6]. In general, posterior fusion approaches, such as posterolateral fusion surgery and transforaminal lumbar interbody fusion, are selected [4]. However, these methods were considered invasive and problematic, with the possible occurrence of adjacent segment disease in the future because the patient was relatively young. Only decompression of the nerve root and open surgery through the Wiltse approach was considered [5], but entire foraminal space and the whole ossification lesion were never invisible with this means, unless almost all parts of the posterior supporting structures of the spine, such as the facet joint and pars interarticular is, were resected. Spinal canal enlargement using restorative laminoplasty is a non-fusion surgical approach and had the advantage of visibility in the foramen, but this approach is more invasive than our approach and includes a complicated procedure[1]. Nerve root decompression without instrumented fusion, i.e., Gill’s procedure[2], was not chosen because progression of anterior slip or instability could occur. Our microendoscopic method had two major advantages. One was the ease to reach the nerve foramen and ossification lesion. The reason for this was that spinal microendoscopy provides an overview of the intra foramen from the outside using the property of its 25° oblique view, without resection of the pars interarticularis and facet joint[6]. The other was the non-invasiveness at the posterior supporting structures of the spine. Therefore, we believed that our approach was the most ideal option to surgically treat our patient. Some studies have reported on the use of an ultrasonic bone curette in spinal surgery [7, 8, 9]. Although minor complications of dural tears with the use of this device have been reported [8], its use is safe in spinal surgery, with a very low complication rate [7, 9], and it is effective with a trend of reduced blood loss[7]. Some reports stated that this device was efficient during foraminotomy, cervical and thoracic corpectomies, and revision spinal surgery [7, 9]. However, there has been no report on its application in microendoscopic spinal surgery. Because the tip of this device was developed to be bent moderately(Fig.6), it is easy to use under a microendoscope with the property of its 25° oblique view. We emphasize that the use of an ultrasonic bone curette in microendoscopic spinal surgery could allow the effective, less invasive, and safe removal of an intraforaminal bony lesion, without the occurrence of allodynia associated with injury to the DRG [10].
Conclusion
For a rare case with radiculopathy resulting from intraforaminal stenosis of the lumbar spine due to an ossification lesion, microendoscopic surgery with an ultrasonic bone curette was applied. The use of ultrasonic bone curette is easy, safe, and effective in microendoscopic surgery and it helps achieve less invasiveness and ideal decompression, without injuring the nerve root.
Clinical Message
This is the first detailed case report of microendoscopic spine surgery using an ultrasonic bone curette for a patient with radiculopathy due to intraforaminal free ossification. The use of ultrasonic bone curette is easy, safe, and very effective in microendoscopic spine surgery and it helps achieve less invasiveness and ideal decompression, without injuring the nerve root.
References
1. Adachi K, Futami T, Ebihara A, Yamaya T, Kasai N, Nakazawa T, et al. Spinal canal enlargement procedure by restorative laminoplasty for the treatment of lumbar canal stenosis. Spine J 2003;3:471-8.
2. Gill GG. Long-term follow-up evaluation of a few patients with spondylolisthesis treated by excision of the loose lamina with decompression of the nerve roots without spinal fusion. Clin Orthop Relat Res 1984;182:215-9.
3. Kunogi J, Hasue M. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine (Phila Pa 1976) 1991;16:1312-20.
4. Wang SJ, Han YC, Liu XM, Ma B, Zhao WD, Wu DS, et al. Fusion techniques for adult isthmic spondylolisthesis: A systematic review. Arch Orthop Trauma Surg 2014;134:777-84.
5. Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 1968;50:919-26.
6. Yamada H, Yoshida M, Hashizume H, Minamide A, Nakagawa Y, Kawai M, et al. Efficacy of novel minimally invasive surgery using spinal microendoscope for treating extraforaminal stenosis at the lumbosacral junction. J Spinal Disord Tech 2012;25:268-76.
7. Al-Mahfoudh R, Qattan E, Ellenbogen JR, Wilby M, Barrett C, Pigott T, et al. Applications of the ultrasonic bone cutter in spinal surgery-Our preliminary experience. Br J Neurosurg 2014;28:56-60.
8. Bydon M, Xu R, Papademetriou K, Sciubba DM, Wolinsky JP, Witham TF, et al. Safety of spinal decompression using an ultrasonic bone curette compared with a high-speed drill: Outcomes in 337 patients. J Neurosurg Spine 2013;18:627-33.
9. Hazer DB, Yaşar B, Rosberg HE, Akbaş A. Technical aspects on the use of ultrasonic bone shaver in spine surgery: Experience in 307 patients. Biomed Res Int 2016;2016:8428530.
10. Darden BV 2nd, Wade JF, Alexander R, Wood KE, Rhyne AL 3rd, Hicks JR, et al. Far lateral disc herniations treated by microscopic fragment excision. Techniques and results. Spine (Phila Pa 1976) 1995;20:1500-5.
 |
 |
 |
| Dr. Masanari Takami | Dr. Keiji Nagata | Dr. Hiroshi Yamada |
| How to Cite This Article: Takami M, Nagata K, Yamada H. Microendoscopic Surgery with an Ultrasonic Bone Curette for a Patient with Intraforaminal Stenosis of the Lumbar Spine Due to an Ossification Lesion: A Technical Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 57-60. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com