[box type=”bio”] Learning Point for this Article: [/box]
Restoration of function in a case of patellar tendon rupture after total knee arthroplasty, using a hamstring graft, is a simple, reproducible, and effective method.
Case Report | Volume 8 | Issue 2 | JOCR Mar – Apr 2018 | Page 57-60| Sumit Anand, Manish Kanwat, Abhinav Mishra,Ravi Mittal, C S Yadav. DOI: 10.13107/jocr.2250-0685.1050
Authors: Sumit Anand[1], Manish Kanwat[2], Abhinav Mishra[3],Ravi Mittal[3], C S Yadav[4]
[1]Department of Orthopaedics, Paras Hospitals, Sector-43, Gurgaon, Haryana, India.
[2]Department of Orthopaedics, Kanwat Orthopaedic Centre, Dwarka, New Delhi, India.
[3]Department of Orthopaedics, AIIMS, New Delhi, India.
[4]Department of Orthopaedics, Paras Hospitals, Patna, Bihar, India.
Address of Correspondence:
Dr. Sumit Anand,
Department of Orthopaedics, Paras Hospitals, Sector-43, Gurgaon, Haryana, India.
E-mail: drsumit_gmc@yahoo.com
Abstract
Introduction: The disruption of extensor mechanism during or after total knee arthroplasty is a rare but disabling complication for the patients. The results of various methods of managing patellar ligament rupture are not predictable and favorable.
Case Report: We report a case of patellar ligament rupturewhich occurred 6 months afterthe primary total knee replacement. It was managed satisfactorily using hamstring graft and minimal implant.
Conclusion: Simple and easily reproducible technique for patellar tendon reconstruction that can be performed by surgeons not routinely performing ligament reconstruction gives favorable outcome.
Keywords: Extensor mechanism rupture, Patellar tendon repair, Total knee arthroplasty, Hamstring graft.
Introduction
The rare incident of extensor mechanism disruption during or after total knee arthroplasty (TKA) is significantly incapacitating to the patients and poses atherapeutic challenge to the surgeons, especially if chronically neglected. The proximal and distal extensor mechanism disruption involving quadriceps and patellar tendon, respectively,is reported to occur in 0.17–2.5% of all total knee replacements [1] and are multifactorial in occurrence. As majority of surgical methods available to manage such patellar ligament rupture give disappointing results, we are presenting a novel surgical technique with encouraging results.
Case Report
A 69-year-old woman underwent bilateral total knee replacement for symptomatic Grade III osteoarthritis of both the knees. The surgery was performed using a midline skin incision and midvastus approach. A cemented cruciate substituting posterior stabilized implant(Stryker NRG Scorpio, right knee femoral component size 4, tibial component size 4,and insert thickness 8 mm and left knee femoral component of size 5, tibial component size 4, and insert thickness 10 mm) was used. The patella was everted during surgery as usual and patelloplasty was done. She recovered well in the post-operative period,attaining range of motion from 0 to 90° by the end of 1st week of surgery, and could walk comfortably without support 4 weeks after the surgery.She did not report until about 6 months after surgery when she started having difficulty in walking with right knee and in getting up from sitting position.She did not have any pain and did not report any trauma. On examination, she had an extension lag of 30° and could flex up to 110° (Fig. 1).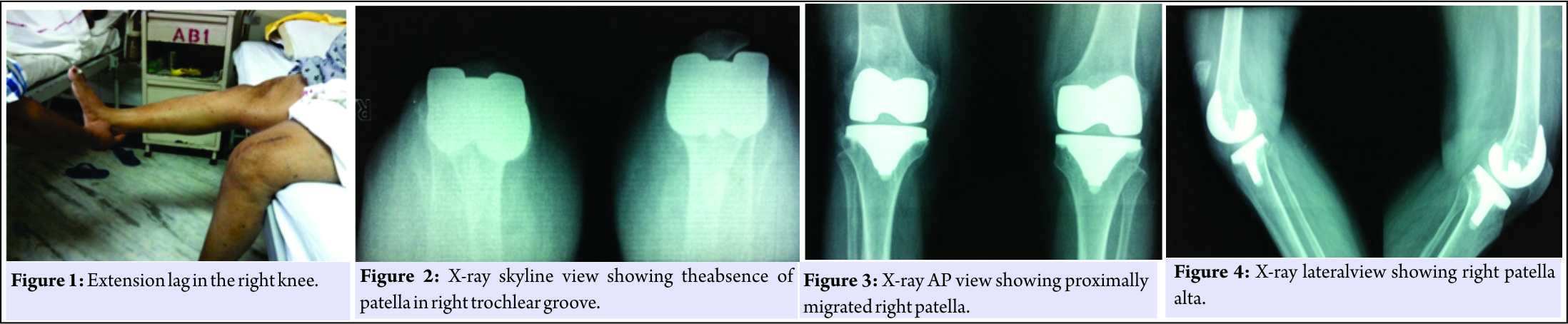
Discussion
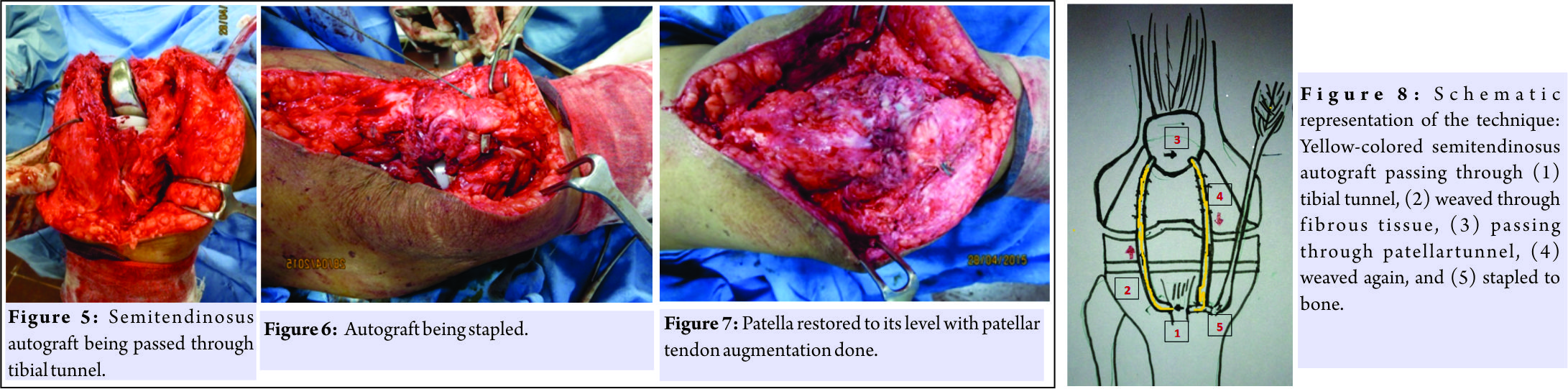
Extensor mechanism disruption is a rare but serious complication after TKA. Patellar tendon rupture can occur intraoperatively due to injury to its fibers while taking bone cuts or postoperatively due to trauma, soft tissue attenuation in associated comorbidities, and infection.Although we have numerous options available such as immobilization, direct primary repair alone by suturing, staples or wiring , and primary repair with biologic or synthetic graft or allograft reconstruction of extensor mechanism, there is no study to suggest an ideal method and the results are inconsistent even more in TKA patients. The factors deciding the treatment include the general health and demands of the patient, the level of disruption,degree of functional loss, chronicity of injury,and availability of viable tissue for direct primary repair or augmentation [2, 3, 4]. Hence, it is wiser to risk stratify patients before hand and take all precautions to prevent an injury to the extensor mechanism. If there is an intraoperative rupture of extensor mechanism, direct repair at this stage is technically easier. Dobbs et al [5] evaluated 18 knees treated for patellar tendon rupture after TKA and reported that direct repair of extensor mechanism has been associated with variable results, with only 25% of the patients having a successful outcome. The need for augmentation can be determined by direct visualization of there pair strength understress. Autogenous graft augmentation after primary repair provides healthy collagen tissue to strengthen the repair tissue [6] and is required in patients with weak connective tissue from systemic disease, infection, and exposed prosthesis or in previously operated knee. Autogenous tissue graft used are semitendinosus and gracilis tendon,free fascia lata graft, plantaris tendon, or gastrocnemius muscle flap [1]. The semitendinosus and/orgracilistendon can be placed along the patellar tendon, passed through a drill hole in patella using various techniques, and then sutured back on itself under appropriatetension [7]. Allograft augmentation using Achilles tendon or extensor mechanism allograft in the setting of a TKAis useful when host tissue is mechanically insufficient and structurally inadequate to support knee function.However, these are not available at mostcenters. Other concerns include immune reaction, disease transmission, and graft strength. Burnett et al. reported promising early results after the use of an extensor mechanism allograft to reconstruct a failed extensor mechanismin patients with previous total knee replacement [8, 9]. The results of Crossett et al. [10] on extensor mechanism repair augmented with Achilles tendon allograft were good and showed improved walking and decreased extensor lag (from 44 preoperatively to 3 postoperatively). Burnett et al. [11] summarized that tensioning the allograft on full extension is a critical determinant of success. The use of allograft for extensor mechanism restoration is best for patients with poor quality host tissue, patients with low functional demand, patients with limited life expectancy, or patients with compromised soft tissue due to multiple previous operations.Modifications such as vigorous tensioning of the graft and protected flexion postoperatively have resulted in improved outcomes, withno compromise to knee flexion. The use of synthetic grafts such as Dacron and Gore–Texpolypropylene and artificial ligaments such as Leeds–Keio ligament allows the majority of load during the early post-operative period to be borne by the synthetic graft sparing the tissue to heal. It also prevents donor site morbidity,but there is an increased risk of infection and poor results in TKA revisions [8]. Ecker et al.[12] reported a post-operative range of 146.4 using Leeds–Keio ligament to repair either disrupted patellar [13, 14] or quadriceps tendon. Many authors suggest the reconstruction with wire cerclage or metalwork to reduce the load on the reconstructed tendon to allow early rehabilitation,but it requires a second intervention to remove the implanted material. Although the cause of patellar tendon rupture in our case could not be established, possible cause can be inherently weak tendon due to old age which ruptured from micro trauma and stretching during and after surgery and then migrated due to chronic neglect. In our method, direct primary repair was not possible and the most challenging part was to bring down the patella. We recommend our method for such chronic ruptures as it gave very satisfying results.
Conclusion
Chronic patellar tendon ruptures in total knee replacement are rare.Surgical repair in such cases can be done by various methods,but there is no ideal method and the results are generally unfavorable.We found that the use of a semitendinosus autograft is effective, easily reproducible,and does not require a second surgery to remove implants.
Clinical Message
Repair of a chronically torn patellar tendon in TKA provides a good outcome, if following points are taken care of:(1) Patellar position should be well restored, (2) the tibial insertion of the semitendinosus graft should be kept intact which gives additional strength to the repair, (3) the autograft should be weaved into the residual tissue (patellar tendon fat pad)for extra strength and smooth mobility, (4) tunnels should be made both in both the patella and the tibial tuberosity, and (5) adequate tensioning should be done before final fixation with a staple.
References
1. Cadambi A, Engh GA. Use of a semitendinosus tendon autogenousgraftforrupture of the patella ligament after total knee arthroplasty. A report of seven cases. J Bone Joint Surg Am 1992;74:974-9.
2. Emerson RH Jr., Head WC, Malinin TI. Reconstruction of patellartendon rupture after total knee arthroplasty with and extensormechanism allograft. Clin Orthop Relat Res 1990;260:154-61.
3. Emerson RH Jr., Head WC, Malinin TI. Extensor mechanism reconstruction with an allograft after total knee arthroplasty. Clin Orthop Relat Res 1994;303:79-85.
4. Lynch AF, Rorabeck CH, Bourne RB. Extensor mechanism complications following total knee arthroplasty. J Arthroplasty 1987;2:135-40.
5. Dobbs RE, Hanssen AD, Lewallen DG, Pagnano MW. Quadriceps tendon rupture after total knee arthroplasty: Prevalence, complications, and outcomes. J Bone Joint Surg Series A2005;87:37-45.
6. Busfield BT, Huffman GR, Nahai F, Hoffman W, Ries MD. Ex-tended medial gastrocnemius rotational flap for treatment of chronicknee extensor mechanism deficiency in patient with and withouttotal knee arthroplasty. Clin Orthop Relat Res 2004;428:190-7.
7. Schoderbek RJ Jr., Brown TE, Mulhall KJ, Mounasamy V, Iorio R, Krackow KA, et al. Extensor mechanism disruption after total knee arthroplasty. Clin Orthop Related Res 2006;446:176-85.
8. Burnett RS, Berger RA, Paprosky WG, Valle CJ, Jacobs JJ, Rosenberg AG. Extensor mechanism allograft reconstruction after total knee arthroplasty: A comparison of two techniques. J Bone Joint Surg 2004;86:2694-9.
9. Barrack RL, Stanley T, Butler RA. Treating extensor mechanism disruption after total knee arthroplasty. Clin Orthop Related Res 2003;416:98-104.
10. Crossett LS, Sinha RK, Sechriest VF, Rubash HE. Reconstruction of a ruptured patellar tendon with Achilles tendon allograft following total knee arthroplasty. J Bone Joint Surg Am 2002;84-A:1354-61.
11. Burnett RS, Berger RA, Valle CJ, Sporer SM, Jacobs JJ, Paprosky WG, et al. Extensor mechanism allograft reconstruction after total knee arthroplasty. J Bone Joint Surg 2005;87 Suppl 1:175-94.
12. Ecker ML, Lotke PA, Glazer RM. Late reconstruction of the patellar tendon. J Bone Joint Surg Am 1979;61:884-6.
13. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981;63:932-7.
14. Mittal R, Kumar N, Yadav CS, Kumar A. Direct repair without augmentation of patellar tendon avulsion following TKA. Case Rep Orthop 2015;2015:391295.
 |
 |
 |
 |
 |
| Dr. Sumit Anand | Dr. Manish Kanwat | Dr. Abhinav Mishra | Dr. Ravi Mittal | Dr. Ravi Mittal |
| How to Cite This Article: Anand S, Kanwat M, Mishra A, Mittal R, Yadav C S.Management of Patellar Tendon Rupture after Total Knee Arthroplasty using Hamstring graft: A Case Report. Journal of Orthopaedic Case Reports 2018. Mar- April; 8(2): 57-60. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





