[box type=”bio”] Learning Point for the Article: [/box]
Lumbar pure facetal dislocation is very rare injury. Such injuries may be associated with visceral and vascular injuries. Prompt recognition and early intervention increase the chance of neurological recovery.
Case Report | Volume 8 | Issue 3 | JOCR May – June 2018 | Page 58-60| Narendra Reddy Medagam, Charanjit Singh Dhillon, Rishi Dwivedi, Pankaj Kumar Jindal, Shrikant Ega. DOI: 10.13107/jocr.2250-0685.1108
Authors: Narendra Reddy Medagam[1], Charanjit Singh Dhillon[1], Rishi Dwivedi[1], Pankaj Kumar Jindal[1], Shrikant Ega[1]
[1]Department of Spine surgery, MIOT international hospital, Chennai. India.
Address of Correspondence:
Dr. Narendra Reddy Medagam,
East wood 3A, Fairmont gardens, manappakam, Chennai, 600089. India.
E-mail: medagam007@gmail.com
Abstract
Introduction: Bilateral facetal dislocation without facet fracture, although common in cervical spine, is a very rare entity in lumbar spine with <15 cases reported so far. Such injuries are very unstable involving all the three columns. Neurological insult and visceral affection are commonly associated with bilateral facetal dislocation.
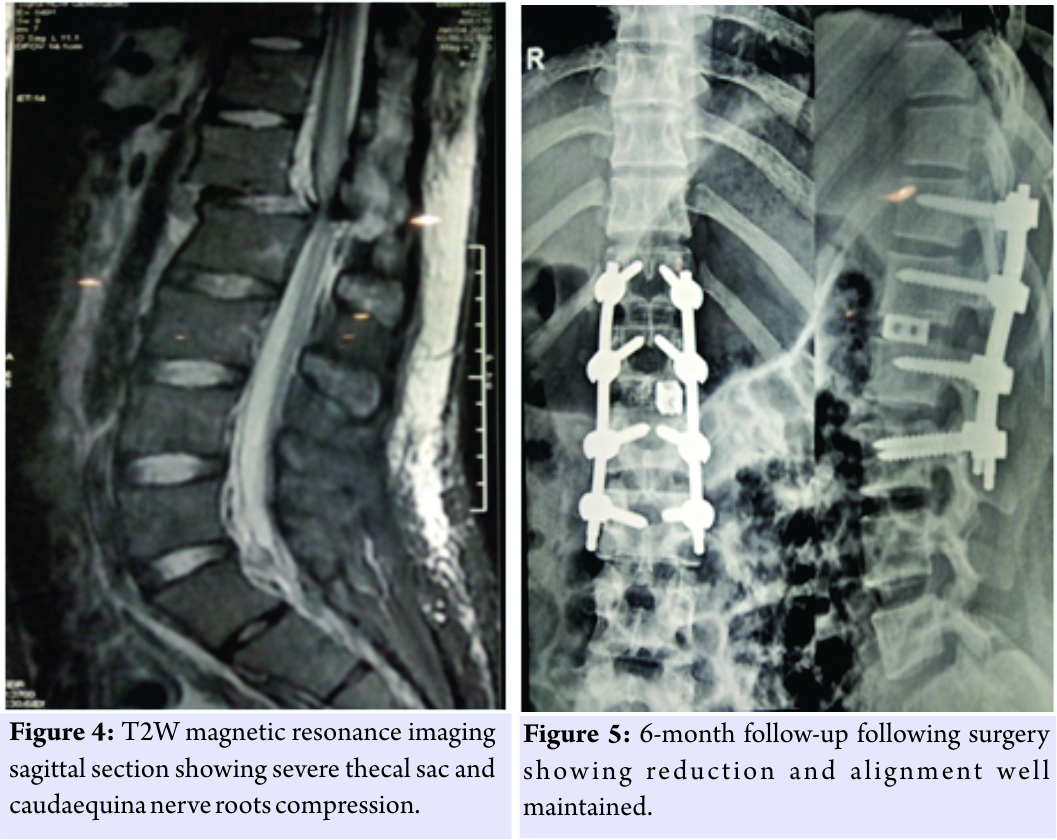
Case Report: A 22-year-old gentleman presented with ASIA Aparaplegia following road traffic accident. Radiographs/computed tomography scan revealed pure facetal dislocation L1-L2 with no evidence of facet fracture. The patient also had liver laceration. The patient underwent open instrumented reduction along with left-sided transforaminal removal of damaged disc and inter body fusion. The patient improved significantly to ASIA C neurological status at 6-month follow-up.
Conclusion: Pure facetal dislocation, although rarely seen in lumbar region, is a very unstable injury. Prompt recognition and early intervention facilitate nursing care and neurological recovery. Recognition of associated injuries is also important.
Key words: Pure facetal dislocation, lumbar facetal dislocation, lumbar spine
Introduction
Pure facet dislocation in lumbar spine is rare with <15 cases reported so far. Facet dislocation is relatively common in cervical spine but quite rare in lower spine owing to facet arrangement, large vertebral body, and firm paraspinal muscular support. These are the result of high-energy trauma and are associated with high incidence of neurological insult. Prompt recognition and early intervention are necessary for restoring spinal alignment and decompressing spinal cord.
Case Report
We present a case of a 22-year-old gentleman with traumatic L1-L2 dislocation without facet fracture. The patient presented to emergency department with alleged history of road traffic accident, when he sustained skid and fall from two wheeler 4 days back at a remote place in Andaman and Nicobar Islands, India. Immediately following trauma, the patient was not able to move his lower limbs and paralysis of his bowel bladder function for which he underwent catheterization in local hospital. Basic spine investigations were done in the form of X-rays and computed tomography (CT)scan, and the patient was immobilized on spine board while he was prepared to be referred to tertiary center. Subsequently, he was referred to our institution for definitive care. 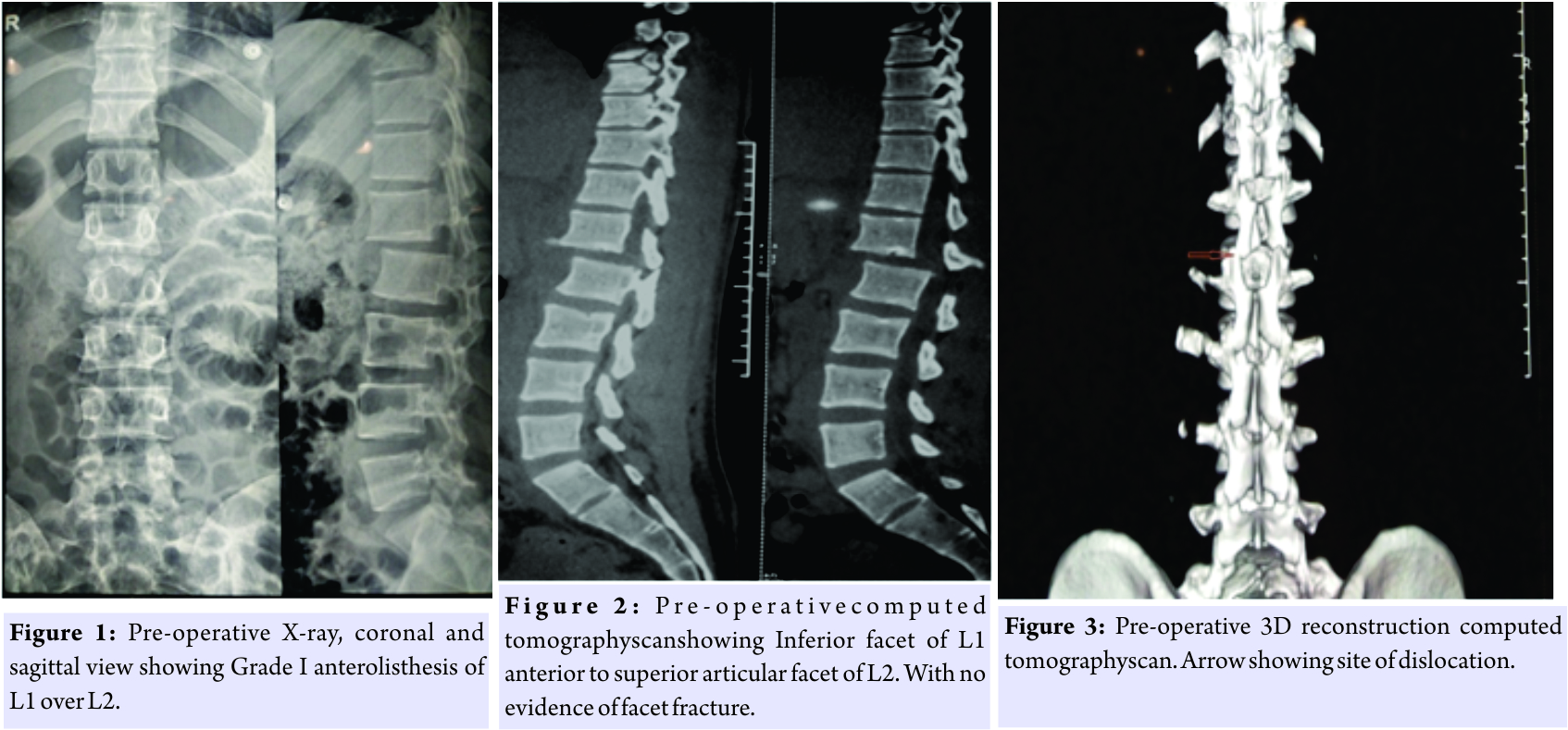
Discussion
Thoracolumbar region (T10-L2) is the most common site of injury [1]. Severity and mechanism of injury defines the stability of the spine. While stable injuries can be managed effectively by conservative means, injuries leading to spine instability [2] endangers neural structures and may warrant direct or indirect decompression and instrumentation to facilitate healing of neural and injured discoligamentous structures as well as to facilitate nursing care. Translation/rotational injuries involve all the three columns [3] and are inherently unstable injuries. Lumbar spine range of motion is predominantly in the sagittal plane with resistance to axial rotation and translation by discoligamentous complex and facet orientation. Due to this anatomical characteristic, failure of spine in rotation or translation is the result of high-energy trauma, and the end result is more unstable spine compared to compression injuries [4]. Patients presenting with thoracolumbar injury require thorough evaluation, to detect any other spine injury incidence of which can be as high as 25% which can present at non-contiguous level [5]. Thorough neurological assessment and visceral and vascular assessment are important to figure out the treatment protocol. Neurological insult is seen in 15% of patients with thoracolumbar trauma. Flexion-distraction injuries at thoracolumbar junction can be associated with abdominal visceral and vascular injuries in nearly 50% of the patients [6]. In this case, the patient had liver laceration which was managed conservatively. The high-energy injuries leading to facetal dislocations are mostly associated with facet fractures as well, making pure facetal dislocations or locked facets very rare injury with <15 cases reported in literature [7, 8]. Although radiographs are good screening tool and may reveal slipping of the vertebra leading, detailed characterization of fracture necessitates CT and MRI imaging. Parasagittal CT cuts through facet reveals locked facet while detailed evaluation is needed to detect associated fractures. Status of interspinous ligaments associated soft tissue and disc injury can be seen on MRI. Disc injury is frequently associated even with minimal slip and needs consideration while planning for the treatment. Injured posterior ligamentous complex, locked facets, and injured disc make it an unstable three-column injury. Conservative treatment has very limited role. However, few authors have reported cases of bilateral lumbosacral dislocation successfully reduced with external reduction maneuvers [9, 10]. This can be associated with high risk of neurological impairment. Surgical intervention is recommended in these cases. Instrumentation through posterior approach allows reduction and restoration of spinal alignment. Inter body fusion can be added depending on surgeon’s preference through anterior or transforaminal approach. In this case, posterior instrumented reduction was done along with transforaminal inter body fusion. The patient improved neurologically from ASIA A to ASIA C.
Conclusion
Lumbar pure facetal dislocation is very rare injury associated with high-energy trauma. Such injuries need thorough evaluation to detect neurological impairment as well as visceral and vascular involvement. Open reduction with instrumentation and lumbar inter body fusion restores segmental stability and improves patient functional ability.
Clinical Message
Upper lumbar pure facetal dislocation is very rare but severe injury. Prompt recognition and early intervention increase the chance of neurological recovery. Such injuries can be associated with visceral and vascular injuries which need thorough evaluation and management.
References
1. Gamanagatti S, Rathinam D, Rangarajan K, Kumar A, Farooque K, Sharma V, et al. Imaging evaluation of traumatic thoracolumbar spine injuries: Radiological review. World J Radiol2015;7:253-65.
2. Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: An overview. Indian J Orthop2015;49:72-82.
3. Tripathi M, Rao KV, Vazhayil V, Srinivas D, Sampath S. Rotational translational injury at the thoracolumbar junction. Neurol India 2016;64:1369-71.
4. Lee JY, Vaccaro AR, Lim MR, Oner FC, Hulbert RJ, Hedlund R, et al. Thoracolumbar injury classification and severity score: A new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci 2005;10:671-5.
5. Calenoff L, Chessare JW, Rogers LF, Toerge J, Rosen JS. Multiple level spinal injuries: Importance of early recognition. AJR Am J Roentgenol1978;130:665-9.
6. Eismont F. Fleexion-Distraction Injuries of Thoracic and Lumbar Spine. In: Levine AM, Eismont FJ, Garfin SR, Zigler JE, editor. Spine Trauma. Philadelphia PA: WB Saunders; 1998.
7. Arnold PM, Malone DG, Han PP. Bilateral locked facets of the lumbosacral spine: Treatment with open reduction and transpedicular fixation. J Spinal Cord Med 2004;27:269-72.
8. Im SH, Lee KY, Bong HJ, Park YS, Kim JT. Bilateral locked facets at lower lumbar spine without facet fracture: A case report. Korean J Spine 2012;9:278-80.
9. Newell RL. Lumbosacral fracture-dislocation: A case managed conservatively, with return to heavy work. Injury 1977;9:131-4.
10. Zoltan JD, Gilula LA, Murphy WA. Unilateral facet dislocation between the fifth lumbar and first sacral vertebrae. Case report. J Bone Joint Surg Am 1979;61:767-9.
 |
 |
 |
 |
| Dr. Narendra Reddy Medagam | Dr. Charanjit Singh Dhillon | Dr. Rishi Dwivedi | Dr. Pankaj Kumar Jindal |
| How to Cite This Article: Medagam N R, Dhillon C, Dwivedi R, Jindal P K, Ega S. Rare Case of Bilateral Pure Facet Joint Dislocation of Upper Lumbar Spine without Facet Fracture:A Case Report. Journal of Orthopaedic Case Reports 2018. May- June; 8(3): 58-60. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




