[box type=”bio”] Learning Point of the Article: [/box]
Traumatic lateral translation of the lumbosacral spine is a highly unstable injury with complete disruption of posterior ligamentous integrity, requiring careful reduction and thorough decompression and stable but rigid posterior fixation and fusion.
Case Report | Volume 8 | Issue 6 | JOCR November – December 2018 | Page 31-33 | Sandeep Sonone, Aditya Dahapute, Nandan Marathe, Saurabh Muni. DOI: 10.13107/jocr.2250-0685.1244
Authors: Sandeep Sonone[1], Aditya Dahapute[1], Nandan Marathe[1], Saurabh Muni[1]
[1]Department of Orthopaedics, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Aditya Dahapute,
Department of Orthopaedics, MSB 6th floor, KEM Hospital, Aurobindo Marg, Parel, Mumbai-400 012, Maharashtra, India.
E-mail: adityadahapute1986@gmail.com
Abstract
Introduction: Traumatic lumbar spondylolisthesis, though a rare lesion, is frequently noted in patients with multiple traumatic injuries sustained in a high-velocity trauma like a road traffic accident.
Case Report: Here, we report a case of traumatic Biplanar translational injury at L5-S1 level with neurological deficit in a 22-year male with motor vehicle accident. Open reduction, decompression, and fusion with rigid fixation were achieved and spine alignment was restored, but the neurological recovery remained uncertain.
Conclusion: These are highly unstable injuries with complete disruption of posterior ligamentous integrity, requiring careful reduction and thorough decompression and stable but rigid posterior fixation and fusion.
Keywords: Traumatic, spondylolisthesis, biplanar injuries, high-velocity trauma.
Introduction
Spondylolisthesis refers to the displacement of a vertebral body on the one below it [1]. It has several etiologies, the most common being spondylolysis and spondylotic degeneration [2]. Five types of spondylolisthesis are reported in literature including dysplastic, isthmic, degenerative, traumatic, and pathologic spondylolisthesis [3]. Traumatic spondylolisthesis is usually accompanied by a fracture of the posterior elements, which result in instability and listhesis [4]. Fracture dislocation of L5-S1 is a rare and severe lesion of the lumbosacral junction usually secondary to violent trauma of the lumbosacral area [5]. Many pathophysiologic hypotheses have been proposed concerning the mechanism. Watson-Jones pointed hyperextension stress as an efficient traumatic vector in the first reported case of lumbosacral dislocation [6]. Roaf suggested that hyperflexion axial rotation and compression forces were responsible for lumbosacral dislocation [7]. These hypotheses might collectively explain the lateral translation seen in this case associated with superior facet fracture.
Case Report
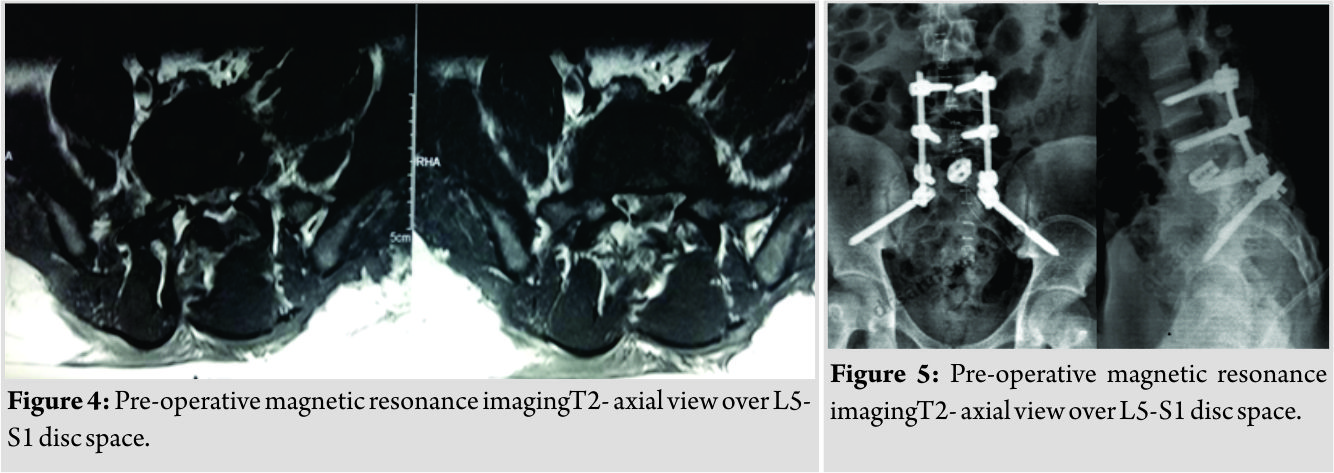
A 22-year young male sustained motor vehicle accident while driving a truck on a highway. Although not sustaining any life-threatening serious injuries, he injured his back and complained of severe debilitating back pain on presentation along with difficulty in moving his left lower limb with difficulty in micturition. On further examination and investigation, he was found to have traumatic spinal instability with traumatic lateral translation of spine along with retrolisthesis at L5-S1 level. On examination, he had a left foot drop with ankle areflexia and severe tenderness at lumbosacral spine. X-ray revealed the right lateral translation at L5 over S1(Fig.1). Computed tomography scan showed lateral translation of spine along with retrolisthesis on sagittal view, with the left facet joint fracture of L5-S1(Fig. 2). 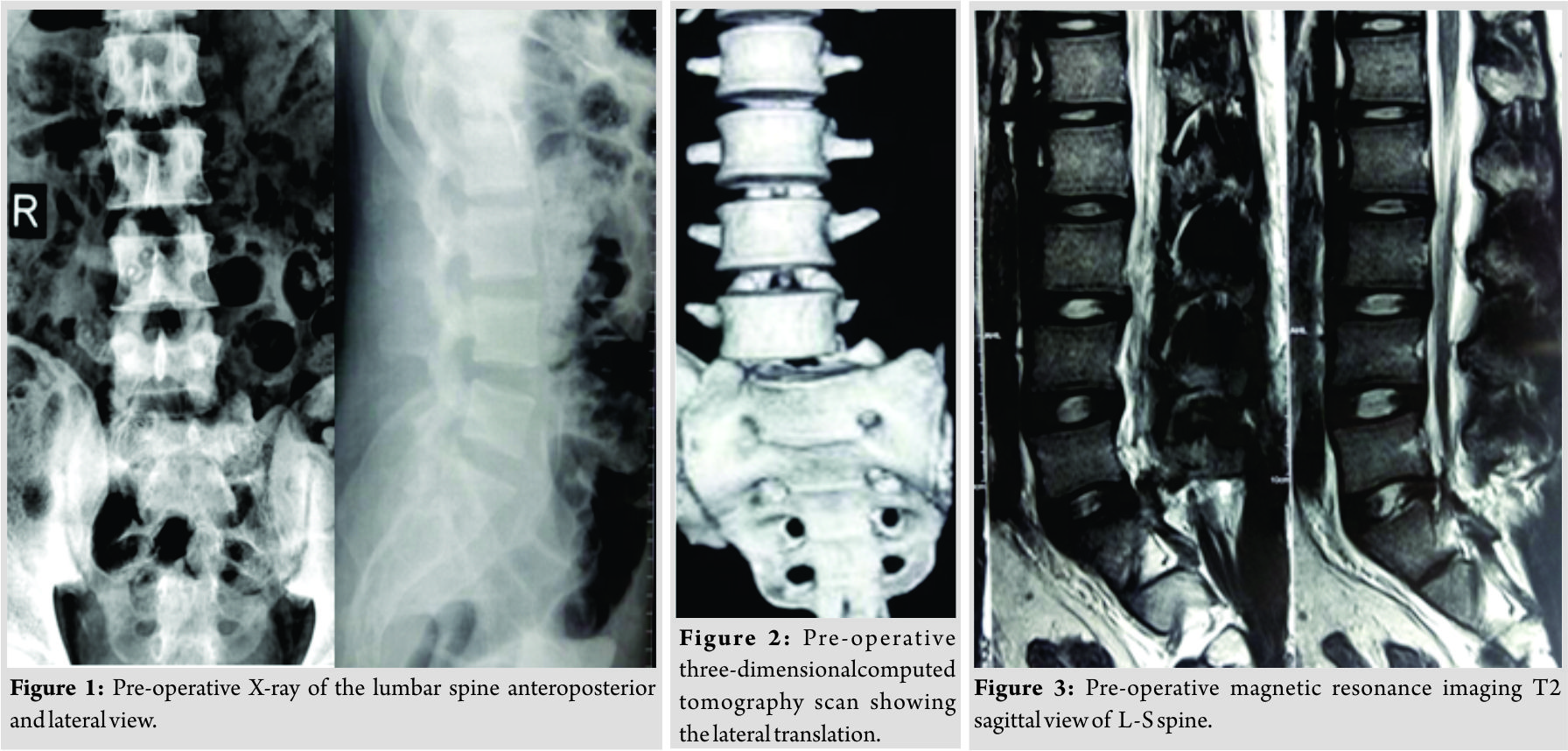
Discussion
Among the array of literature available for various traumatic spine ailments, the one for traumatic lumbosacral spine instability in either plane is quite rare. Only few case reports exist except for a review of independent case reports by Herron and William [8] in which 18 such cases were reviewed, and it states that neural injury is frequent in cases involving facet fracture with flexion and rotation been the mechanism of injury. Review of literature of similar cases suggests that these associated listhesis or instability have been diagnosed later or is picked up incidentally, and mostly have never been a primary complaint as associated other injuries have taken precedence and except for this case report; none had neurological deficit at presentation. This causes the delay in its diagnosis and treatment [11]. Here, the patient presented with neurodeficit occurring because of the component of lateral translation with hyperflexion-rotation injury causing immediate neural compromise as is noted a case series of four by Mc Grath and Das [9]. Assessment of MRI of reported cases shows that usually in traumatic listhesis there is complete destruction of disc due to crushing injury as vertebrae translate over each other, but surprisingly, in this case, there is well-maintained disc height. This may be due to lateral translation with facet fracture; same was the finding noted in only one case report similar to this reported by Vialle and Court[10]. Treatment of listhesis and associated lateral translation whatever may be the cause entails decompression fixation and fusion with or without reduction, here, it had to be very meticulous as bilateral L5 and S1 roots where affected in the trauma which not only had to be decompressed but also were to be taken care of while attempting to reduce the translation. It was essential to restore normal lumbar alignment, decompress the nerve structures, and stabilize the lumbar spine, using open reduction and rigid fixation. Any kind of malreduction at this junctional region can cause serious deformity. Due to associated fracture with biplanar injury with posterior ligamentous disruption and frank instability at a junctional region in a young patient who is a manual laborer the fixation had to be rigid enough and to ensure that the fixation was spanned from L4 to ilium with L5-S1 fusion. Postoperatively, bladder-related complaints improved, but neurological recovery was not evident, which may be the case due to profound injury to the roots caused by lateral/coronal component of the listhesis. The patient is now pain free and mobile with ankle-foot orthosis. 6-month follow-up shows maintenance of alignment and initiation of fusion.
Conclusion
These biplanar injuries occur in high-intensity injuries. Although lateral translations are rare injuries, these are much more debilitating neurologically due to increased likelihood of nerve root affection in either plane of injury, especially the coronal plane occurring by mechanism of rotation. MRI in such cases shows root affection, but surprisingly well-maintained disc that is not crushed in lateral translational injury as compared to sagittal translational injury.
Clinical Message
These are highly unstable with complete disruption of posterior ligamentous integrity, requiring careful reduction and thorough decompression and stable but rigid posterior fixation and fusion.
References
1. Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 1984;66:699-707.
2. Fitzgerald J, Newman PH. Degenerative spondylolisthesis.J Bone Joint Surg Br1976;58:184-92.
3. Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis.J Bone Joint Surg Am1983;65:768-72.
4. Ahmed A, Mahesh BH, Shamshery PK, Jayaswal A. Traumatic retrolisthesis of the L4 vertebra. J Trauma 2005;58:393-4.
5. Tsirikos A, Saifuddin A, Noordeen MH, Tucker SK. Traumatic lumbosacral dislocation: Report of two cases. Spine 2004;29:E164-8.
6. Watson-Jones R. Fractures and Joint Injuries. 1st ed. Baltimore: Williams & Wilkins; 1940. p. 641.
7. Saiki K, Hirabayashi S, Sakai H, Inokuchi K. Traumatic anterior lumbosacral dislocation caused by hyperextension mechanism in preexisting L5 spondylolysis a case report and a review of literature. J Spinal Disord Tech 2006;19:455-62.
8. Herron LD, William RC. Fracture-dislocation of the lumbosacral spine. Report of a case and review of the literature. Clin Orthop Related Res 1984;186:205-11.
9. McGrath SW, Das De S. Lumbosacral fracture-dislocations. A report of four cases. JBJS Br 1981;63-B:58-60.
10. Vialle R, Court C. Traumatic lateral lumbosacral dislocation: One case and review of literature. Spinal Disord Tech 2005;18:286-9.
11. Ponzo L, De Gannaro GL. ???.ChirOrgami Mov 1994;79:315-9.
 |
 |
 |
 |
| Dr. Sandeep Sonone | Dr. Aditya Dahapute | Dr. Nandan Marathe | Dr. Saurabh Muni |
| How to Cite This Article: Sonone S, Dahapute A, Marathe N, Muni S. A Rare Case of Traumatic Lateral Translationof Lumbosacral Spine with Nerve Root Avulsion. Journal of Orthopaedic Case Reports 2018 Nov-Dec; 8(6): 31-33. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com