[box type=”bio”] Learning Point of the Article: [/box]
In the case of an unsuccessful closed reduction of a talus dislocation, open reduction is crucial in order to avoid further damage of the soft-tissue.
Case Report | Volume 8 | Issue 6 | JOCR November – December 2018 | Page 34-37 | Iraklis Itsiopoulos, Angelo V. Vasiliadis, Vasileios Goulios, Petros Bangeas, Konstantinos Sapalidis. DOI: 10.13107/jocr.2250-0685.1246
Authors: Iraklis Itsiopoulos[1], Angelo V. Vasiliadis[2], Vasileios Goulios[1], Petros Bangeas[1], Konstantinos Sapalidis[1]
[1]Department of Surgery, Propedeutic Surgical Clinic, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
[2]Department of Orthopaedic Surgery, General Hospital of Katerini, Katerini, Greece.
Address of Correspondence:
Dr. Angelo V. Vasiliadis,
Department of Orthopaedic and Trauma Surgery, General Hospital of Katerini, Katerini, Greece. 45 K. Varnali Str, Thessaloniki, PC 54352, Greece.
E-mail: vasiliadis.av@gmail.com
Abstract
Introduction: Talus dislocation without a concomitant fracture of the malleoli is a rare injury.
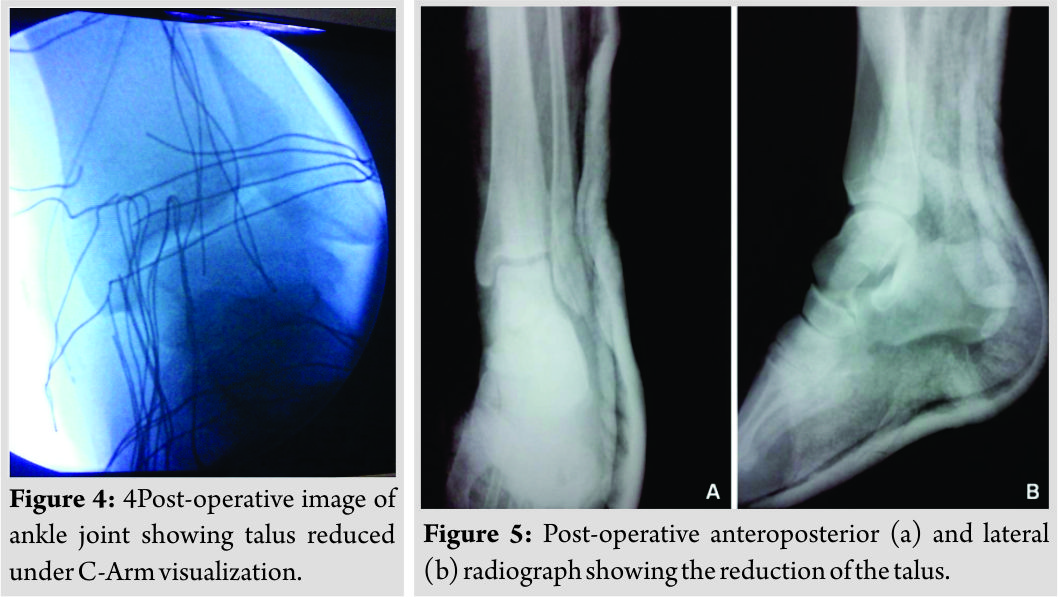
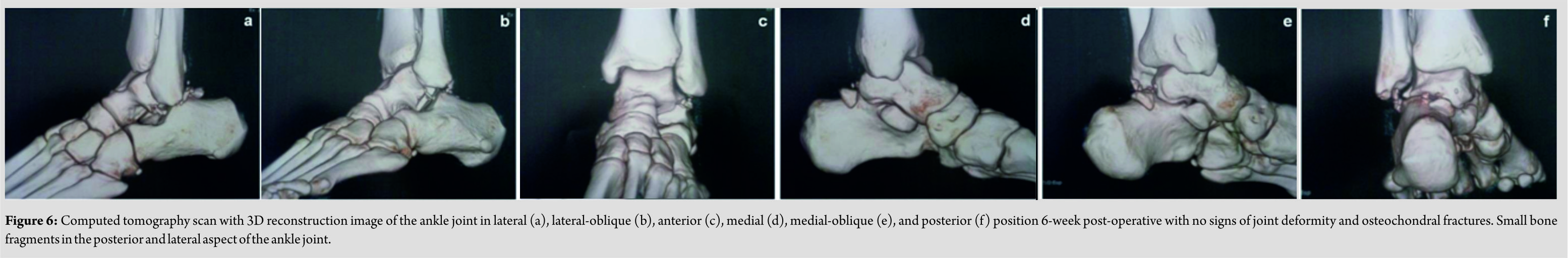
Case Report: We present a case of a closed anteromedial talus dislocation in a 25-year-old male motorcyclist due to a high-energy trauma, resulting from a fall following a road traffic accident. The talus could not be reduced by closed means making open reduction performed through a dorsal approach necessary. At 6-month follow-up, the patient has little pain and the range of ankle motion was satisfactory with some signs of bone contusion.
Conclusions: Talus dislocation is a rare injury that occurs after high-energy trauma. Open reduction can be beneficial, particularly if the initial attempt at closed reduction fails.
Keywords: Talus, closed dislocation, fracture, operative treatment.
Introduction
Ligamentous injuries involving the ankle joint are relatively common, while closed total talus dislocation without fractures of the malleoli, navicular, calcaneus, or talus is an extremely rare injury due to the presence of strong ligaments connecting these bones [1, 2]. Closed talus dislocations are usually associated with high-energy mechanical trauma and usually occur in young patients [2, 3]. Avascular necrosis of the talus, infection, and post-traumatic arthritis of the ankle joint are the most commonly reported major complications, potentially affecting otherwise healthy subjects in the most active period of their lives [4]. Treatment options remain controversial with the proposed treatment strategies varying from closed reduction versus open reduction and internal fixation [4, 5]. The purpose of this report is to describe a closed talus dislocation without any fracture of the malleoli, which was treated by open reduction. A comprehensive review of the relevant literature is provided, summarizing the present state of knowledge regarding this type of rare injury.
Case Report
A 25-year-old man was transferred to the emergency department by ambulance with an injury to the left ankle, after been involved in a road traffic accident (fall from own motorbike). He had sustained a minor injury to the head with an extensive blunt laceration of the soft tissues of the scalp (Glasgow Coma Scale, 15/15), a rib fracture accompanied by pneumothorax, as well as bruises and abrasions of the lower extremities. His primary complaint was severe pain and deformity of his left ankle. On physical examination, the ankle joint was noted to be deformed, swollen, and tender without lacerations. The skin temperature was normal, the sensory function could not be estimated because of pain, and there was motor loss. As the peripheral pulse was not palpable, the initial vascular status was assessed by applying the capillary nail refill test (observed). There is an obvious clinical deformity, and the ankle is revealed in a medial position with the talus head raised under the skin (Fig. 1).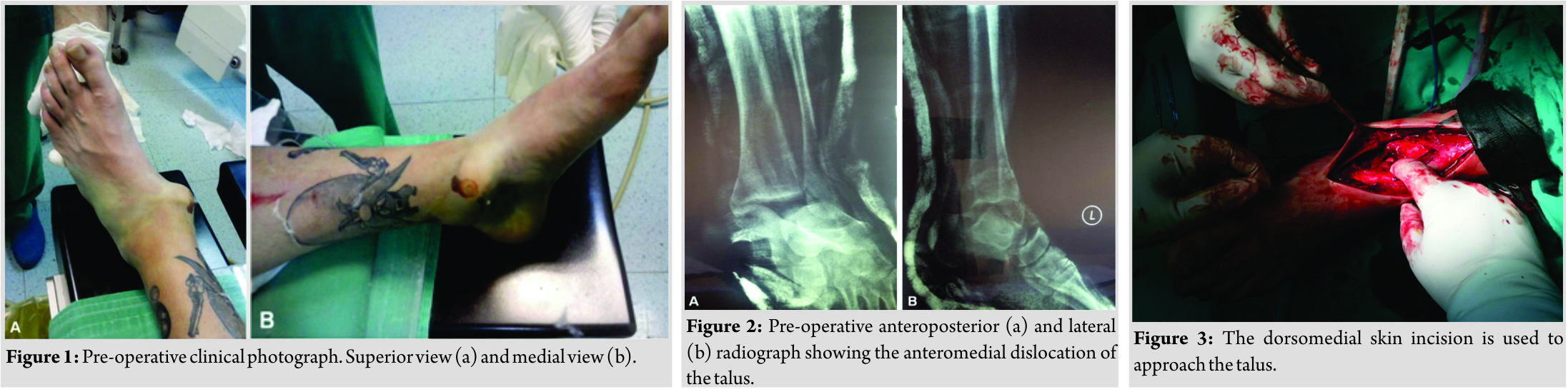
Discussion
As previously stated, talus dislocation is mainly occurred among young adults aged 20–45 years and associated with high-energy trauma [2, 3]. In the present report, we describe the case of a young adult sustaining a closed talar dislocation arising from a fall from his motorbike in a road traffic accident. In light of this report, we review the literature for the etiology, mechanism of injury, diagnosis, treatment, and follow-up outcomes of talus dislocation (Table 2). Talus dislocation without fracture of the malleoli or talus is a very rare injury [1, 2]. This injury results from high-energy trauma, and the most common etiologic factors of this type of injury are road traffic accidents [2, 3, 7, 8] and fall from a height (Table 2) [9, 10]. The usual mechanism of talus dislocation is a combination of plantar flexion while the foot comes to supination or pronation, and the dislocation can be either anterolateral (the most common) or posteromedial [2, 4]. The initial diagnosis of talus dislocation is often made using plain radiographs (anteroposterior and lateral views of the ankle joint) which can confirm clinical suspicions and reveal any fractures of the bones [3]. Late complications commonly include avascular necrosis and post-traumatic arthritis. These complications may be related to the injury, the open reduction, or a combination of both. The most sensitive diagnostic tool for avascular necrosis is MRI, usually 10 weeks after the initial trauma diagnosis [7]. The use of CT may delineate the extent of chondral damage or minor fractures which may lead to post-traumatic arthritis years after the initial injury [10]. Talus dislocation without any accompanying fracture is such a rare injury that there are no clear treatment guidelines. Most authors underline the importance of an immediate closed reduction of the dislocated ankle [3]. There are several different methods of closed reduction according to the orientation of the foot in relation to the talus [8]. However, the goal of treatment remains a stable anatomic reduction of the talus in the ankle joint. It is useful to mention that, after each closed reduction attempt, a repeat of the neurovascular examination is crucial to ensure that blood flow has been maintained and no new sensory or motor compromise has occurred. In the light of the literature for open injuries, most authors suggest that open reduction is the preferable treatment choice and that talectomy with tibial-calcaneal arthrodesis (or fusion) should be used to preserve joint stability and maintain good clinical and functional outcomes [7, 9]. Open reduction is also the preferred option after an unsuccessful attempt at closed reduction. For some authors, it is the first choice to avoid potential complications, with the most serious of these being osteonecrosis [2].
Conclusion
Talus dislocation is an infrequent injury that occurs after high-energy trauma, such as road traffic accident, or falls from a height and most frequently involves active young men. A successful outcome for the patient is the primary goal, making early diagnosis and treatment of paramount importance. Open reduction can be beneficial, particularly if the initial attempt at closed reduction fails, and if complications such as osteonecrosis are to be avoided.
Clinical Message
Dislocation of the talus is an extremely rare and is usually associated with high-energy mechanical trauma in young adult males. An early closed reduction must be attempted to avoid further soft tissue and blood supply compromise. Multiple attempts of closed reduction are not advised as they can further damage the soft-tissue, and an open reduction is indicated.
References
1. Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, et al. Anatomy of the ankle ligaments: A pictorial essay. Knee Surg Sports Traumatol Arthrosc 2010;18:557-69.
2. Rhanim A, Zanati RE, Younes Ouchrif, Hassani ZA, Kharmaz M, Berrada MS, et al. Nonoperative treatment of closed total talus dislocation without fracture: A case report and literature review. J Clin Orthop Trauma 2014;5:172-5.
3. Karampinas PK, Stathopoulos IP, Vlamis J, Polyzois VD, Pneumatikos SG. Conservative treatment of an anterior-lateral ankle dislocation without an associated fracture in a diabetic patient: A case report. Diabet Foot Ankle 2012;3: doi: 10.3402/dfa.v3i0.18411.
4. Xarchas KC, Psillakis IG, Kazakos KJ, Pelekas S, Ververidis AN, Verettas DA, et al. Total dislocation of the talus without a fracture. Open or closed treatment? Report of two cases and review of the literature. Open Orthop J 2009;3:52-5.
5. Kumar YC, Reddy S, Golla DK, Ganesh N. Closed talar dislocation without associated fracture a very rare injury, a case report. J Orthop Case Rep 2014;4:10-2.
6. Mitchell JI. Total dislocation of the astragalus. J Bone Joint Surg Am 1936;13:212-4.
7. Sié EJ, Traoré A, Sy AK, Soumaro K, Lambin Y. Delayed debridement of an open total talar dislocation reimplanted in the emergency room. J Clin Orthop Trauma 2014;5:176-80.
8. Sharifi SR, Ebrahimzadeh MH, Ahmadzadeh-Chabok H, Khajeh-Mozaffari J. Closed total talus dislocation without fracture: A case report. Cases J 2009;2:9132.
9. Lee J, Hamilton G. Complete talar extrusion: A case report. J Foot Ankle Surg 2009;48:372-5.
10. Taymaz A, Gunal I. Complete dislocation of the talus unaccompanied by fracture. J Foot Ankle Surg 2005;44:156-8.
 |
 |
 |
 |
 |
| Dr. Iraklis Itsiopoulos | Dr. Angelo V. Vasiliadis | Dr. Vasileios Goulios | Dr. Vasileios Goulios | Dr. Konstantinos Sapalidis |
| How to Cite This Article: Itsiopoulos I, Vasiliadis A V, Goulios V, Bangeas P, Sapalidis K. Open Treatment of Closed Talus Dislocation without Fracture: A Case Report and Literature Review. Journal of Orthopaedic Case Reports 2018 Nov-Dec; 8(6): 34-37. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




