[box type=”bio”] Learning Point of the Article: [/box]
Lumbar puncture with unstyletted needle should be avoided. Intradural epidermoid is a cause for acute paraparesis in children.
Case Report | Volume 8 | Issue 6 | JOCR November – December 2018 | Page 96-99 | Suresh Pillai, Alice T Cherian. DOI: 10.13107/jocr.2250-0685.1278
Authors: Suresh Pillai[1], Alice T Cherian[1]
[1]Department of Spine Surgery, Baby Memorial Hospital, Calicut , Kerala, India.
Address of Correspondence:
Dr. Suresh Pillai,
Preethi”, Opposite kseb, Court Junction, Mavelikkara, Alapuzha, Kerala, India.
E-mail: sureshorth@gmail.com
Abstract
Introduction: Lumbar puncture with unstyletted needle or any other spine trauma can cause implantation of skin fragments inside the dura and can cause acquired intraspinal epidermoid tumors. There is significant delay found between the episode of lumbar puncture and the presentation of the tumor. To the best of our knowledge, there is no reported case of intraspinal epidermoid tumor presenting as acute paraparesis secondary to infection of the tumor in the literature.
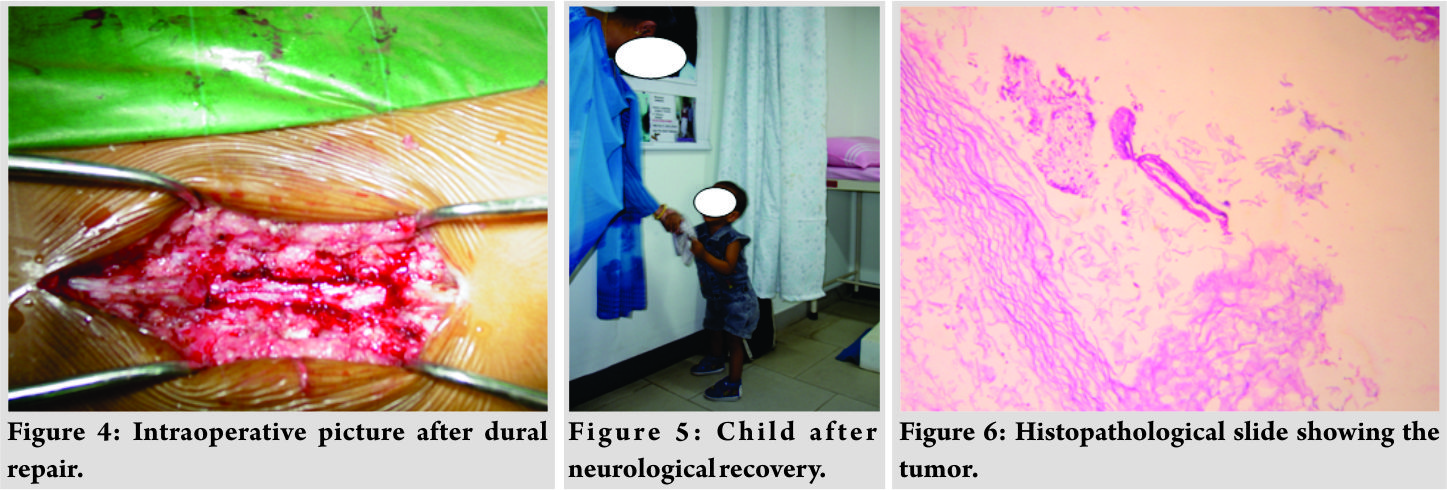
Case Report: A 19-month-old boy presented with acute paraparesis with acute bowel bladder involvement following an episode of fever cough and diarrhea. Investigations revealed that he had an intradural tumor with a secondary infection which caused the problem. Child was treated surgically with complete neural recovery. He has been under follow-up for possible recurrence
Conclusion: Use of unstyletted needle for lumbar puncture is a possible cause for intraspinal epidermoid tumors. To the best of our knowledge, there is no reported case of intraspinal epidermoid tumor with secondary infection presenting as acute paraparesis, in the literature.
Keywords: Epidermoid, infection, intradural, paraparesis
Introduction
Intraspinal epidermoid tumors can be congenital or acquired. The acquired tumors are extremely rare: However, they are well documented in the literature [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15]. The earliest report was made by Choremis and Associates [1]. These acquired tumors are caused by skin fragments which are implanted in the spine as a result of lumbar puncture or other trauma to the spine [7, 9]. Due to the significant time lag between the trauma and the development of a symptomatic tumor, the relationship is often overlooked and this may even cause a delay in proper diagnosis. The majority of these tumors are reported in children but they are also seen in adults [14]. So far no cases have been reported in the literature with signs and symptoms of acute paraplegia due to secondary infection of an already existing asymptomatic intraspinal epidermoid tumor. Our case seems to be unique in that respect. A previously healthy child presented with fever and acute paraparesis and, on further investigation, was found to have an iatrogenic extraspinal epidermal inclusion cyst. Despite all the new technological advances in medicine, the performance of lumbar puncture with unstyletted needles is still a common practice, especially among infants [5, 8, 12, 14, 15, 16]. This practice is the main etiological factor for the development of these tumors.
Case Report
A previously healthy 19-month-old boy initially presented with fever, cold, cough, and diarrhea about 3 weeks before to admission. At that time, he was treated with oral cefixime for 5 days by his pediatrician. His fever and diarrhea resolved after 1 week. However, he developed difficulty walking following that and became completely bedridden in the next week. At the time of admission, he was unable to stand up and had some intermittent dribbling of urine. There was no disturbance in the bowel habits. The only significant information in his medical history was that he underwent lumbar puncture in the neonatal period in the 1st week of life for suspected sepsis and meningitis. 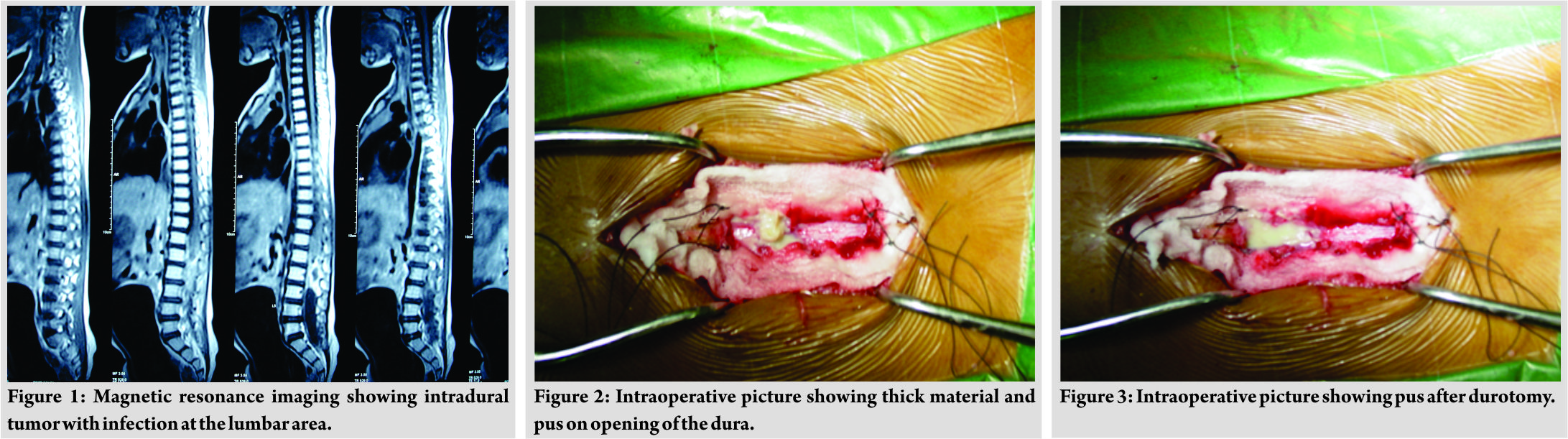
Discussion
Histologically, epidermoid tumors consist of a mass of desquamated cells containing keratohyalin encased in a capsule of the stratified squamous epithelium [8]. Pathogenesis of intraspinal epidermoid tumors can be congenital or acquired. Congenital tumors arise from embryonic rests of epidermal cells, associated with spinal malformations such as spina bifida and other dysraphic states [8, 17, 18]. The iatrogenic tumors result from the direct introduction of epidermal tissue into the spinal canal by lumbar puncture or by penetrating trauma of the spine from bullet wounds, stab wounds, and et cetera. Gibson and Norris found that solid fragments of tissue are trapped inside the needle when hollow needles are used to penetrate skin [19]. They also noted that stylet fitted needles did not trap skin fragments as long as this style was well fitted. Van Glider and Schwartz were able to produce intraspinal epidermoid tumors in rats by implanting skin homograft into the epidural and subarachnoid space [20]. The incidence of intraspinal epidermoid tumors, in general, is rather low. They constitute <1% of all the spinal tumors collectively. Approximately 40% of the acquired types are considered to be late complications of lumbar puncture [15]. Recently, there seems to be a slight increase in the incidence of these cases which is probably due to better awareness and early diagnosis [8, 15]. These tumors are reported mainly among children but they are also seen in adults [14, 16]. Most patients have uniform symptoms such as low back pain and rigidity. Some patients may develop bladder dysfunction and varying degrees of decrease in muscle power in the lower limbs by the time of diagnosis [1]. The time interval between lumbar puncture and the diagnosis of a symptomatic tumor varies from case to case, varying from several months to a number of years [6]. Our patient did not have any symptoms until he developed a febrile illness and secondary infection of the growing tumor, most likely from transient bacteremia associated with his febrile illness. Infection of the tumor and the accumulated pus resulted in the development of acute paraparesis. Complete surgical removal of these tumors is a rather difficult procedure. Due to this, there is a definite risk for recurrence [20, 21]. However, the advent of MRI has improved the accuracy of early diagnosis and the possibility of complete resection [12]. Close follow-up of the patient with periodical neurological examination is important in detecting the recurrence early. The most important issue is the prevention of these types of tumors. This can be achieved by strict adherence to proper protocol when performing a lumbar puncture in children. The use of properly fitted, styletted needles is the key factor. In emergency situations, the ease of entry into the subarachnoid space while using an unstyletted needle may be a greater priority than the future risk of developing an epidermoid tumor. Some authors have advocated the method of spinal puncture in which the stylette is removed after passing through the epidermis and dermis and then advancing the needle until cerebrospinal fluid flow occurs [7, 22]. Considering the morbidity associated with iatrogenic epidermoid tumors one should take the precaution of doing lumbar puncture only with properly fitted styleted needles.
Conclusion
Use of unstyletted needle for lumbar puncture is a possible cause for intraspinal epidermoid tumors. To the best of our knowledge, there is no reported case of the intraspinal epidermoid tumor with secondary infection presenting as acute paraparesis, in the literature.
Clinical Message
Considering the morbidity associated with iatrogenic epidermoid tumors one should take the precaution of doing lumbar puncture only with properly fitted styleted needles.
References
1. Choremis C, Economos D, Gargoulas A, Papadatos C. Intraspinal epidermoid tumours (cholesteatomas) in patients treated for tuberculous meningitis. Lancet 1956;271:437-9.
2. Blockey NJ, Schorstein J/ Intraspinal tumours in lumbar region of children. J Bone Joint Sur[Br] 1961;43:556-62.
3. Manno NJ, Uihlein A, Kernohan JW. Intraspinal epidermoids. J Neurosurg 1962;19:754-65.
4. Boyd HR/ Iatrogenic intraspinal epidermoid. Report of a case. J Neurosurg 1966;24:105-7.
5. Shaywitz BA. Epidermoid spinal cord tumors and previous lumbar punctures. J Pediatr 1972;80:638-40.
6. Batnitzky S, Keucher TR, Mealey J Jr. Campbell RL. Iatrogenic intraspinal epidermoid tumors. JAMA 1977;237:148-50.
7. Halcrow SJ, Crawford PJ, Craft AW. Epidermoid spinal cord tumour after lumbar puncture. Arch Dis Child 1985;60:978-9.
8. McDonald JV, Klump TE. Intraspinal epidermoid tumors caused by lumbar puncture. Arch Neurol 1986;43:936-9.
9. Gardner DJ, O’Gorman AM, Blundell JE. Intraspinal epidermoid tumour: Late complication of lumbar puncture. CMAJ 1989;141:223-5.
10. Baba H, Wada M, Tanaka S, Imura K. Intraspinal epidermoid cyst after lumbar puncture. Int Orthoped 1994;18:116-8.
11. Roux A, Mercier C, Larbrisseau A, Dube LJ, Dupuis C, Del Carpio R, et al. Intramedullary epidermoid cysts of the spinal cord. Case report. J Neurosurg 1992;76:528-33.
12. Ziv E, McComb G. Iatrogenic epidermoid tumour: Two cases and a review of the literature. Spine 2004;29:15-8.
13. Ferrara P, Costa S, Rigante D, Mule A, D’Aleo C, Pulitanò S, et al. Intramedullary epidermoid cyst presenting with abnormal urological manifestations. Spinal Cord 2003;41:645-8.
14. Miyake S, Kobayashi N, Murai N, Kondoh T, Kohmura E. Acquired lumbar epidermoid cyst in an adult. Neurol Med Chirurgica 2005;45:277-9.
15. Per H, Kumandaş S, Gümüş H, Yikilmaz A, Kurtsoy A. Iatrogenic epidermoid tumor: Late complication of lumbar puncture. J Child Neurol 2007;22:332-6.
16. Chandra PS, Manjari T, Devi BI, Chandramouli BA, Srikanth SG, Shankar SK, et al. Intramedullary spinal epidermoid cyst. Neurol India 2000;48:75-7.
17. Mazzola CA, Albright AL, Sutton LN, Tuite GF, Hamilton RL, Pollack IF, et al. Dermoid inclusion cysts and early spinal cord tethering after fetal surgery for myelomeningocele. N Engl J Med 2002;347:256-9.
18. List CF. Intraspinal epidermoids, dermoids, and dermal sinuses. Surg Gynecol Obstet 1941;73:525-38.
19. Gibson T, Norris W. Skin fragments removed by injection needles. Lancet 1958;2:983-5.
20. VanGliden JC, Schwartz HG. Growth of epidermoids from skin implants to the nervous system and surrounding spaces of the newborn rat. J Neurosurg 1967;26:14-20.
21. Lunardi P, Missori P, Gagliardi FM, Fortuna A. Long-term results of the surgical treatment of spinal dermoid and epidermoid tumors. Neurosurgery 1989;25:860-4.
22. Mushlin S. Best technique for lumbar puncture. N Engl J Med 1974;290:1262.
 |
| Dr. Suresh Pillai |
| How to Cite This Article: Pillai S, Cherian A T. Iatrogenic Intraspinal Epidermal Inclusion Cyst with Secondary Infection: A Cause for Acute Paraparesis. Journal of Orthopaedic Case Reports 2018 Nov-Dec; 8(6): 96-99. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com