[box type=”bio”] Learning Point of the Article: [/box]
The IBSN is susceptible to neuroma formation after surgery over the anteromedial aspect of the knee.
Case Report | Volume 9 | Issue 4 | JOCR July-August 2019 | Page 10-13 | Cedric Ngbilo, Eric Choudja Ouabo, Biljana Jovanovic, Adnan Saithna, Laurent Gillain, Bertrand Sonnery Cottet. DOI: 10.13107/jocr.2019.v09i04.1456
Authors: Cedric Ngbilo[1],[4], Eric Choudja Ouabo[2], Biljana Jovanovic[2], Adnan Saithna[3], Laurent Gillain[2], Bertrand Sonnery Cottet[4]
[1]Department of Orthopedic and Traumatology Surgery, CHUV, Lausanne University Hospital, 1011 Lausanne, Switzerland,
[2]Private Practice, Center of Orthopedic Surgery, Clinique Bois-Cerf, 1006 Lausanne, Switzerland,
[3]Sano Orthopedics, Kansas City, Missouri, USA,
[4]Department of Orthopedic, Centre Orthopédique Santy, Groupe Ramsay-General Health, FIFA Medical Center of Excellence, Lyon, France.
Address of Correspondence:
Dr. Eric Choudja Ouabo,
Center of Orthopedic Surgery, Clinique Bois-Cerf, Avenue D’ouchy 31, 1006 Lausanne, Switzerland.
E-mail: e_choudja@hotmail.com
Abstract
Introduction: Neuromas of the infrapatellar branch of the saphenous nerve (IBSN) can occur after direct trauma or surgical approaches to the anterior aspect of the knee. The purpose of this case report is to highlight the clinical presentation, diagnosis, and successful surgical management
Case Report: A 20-year-old patient who had a history of recent anterior knee surgery at another institution presented with allodynia, dysesthesia, and a positive Tinel’s test over the surgical scar. The pain was exacerbated by light touch, was progressively worse, and was limiting sports participation and activities of daily living. A clinical diagnosis of neuroma of the IBSN was made and this was successfully treated by microsurgical neurolysis, resection of the neuroma, and burying of the stump. This resulted in complete resolution of pain.
Conclusion: Neuromas of the IBSN can cause significant symptoms affecting activities of daily living. Microsurgical neurolysis is a useful treatment modality associated with complete resolution of pain and high patient satisfaction.
Keywords: Pain, neuroma, knee, partial denervation, infrapatellar pain syndrome, infrapatellar branch of the saphenous nerve.
Introduction
The saphenous nerve is a branch of the femoral nerve. It is derived from the second through the fourth lumbar roots. It is a superficial structure that lies behind the posterior border of the Sartorius [1]. Its infrapatellar branch is purely sensory and innervates both the anteromedial aspect of the knee and the anteroinferior portion of the knee capsule [2, 3]. Infrapatellar pain syndrome (IPS) can be caused by trauma, such as a fall or direct blow to the knee as well as by surgical procedures such as arthroscopy [4], total knee replacement, bone-patellar tendon-bone or hamstring tendon graft harvest procedures, tibial nailing, and open anterior procedures of the knee [5]. IPS is infrequently reported in literature and can be overlooked or misdiagnosed as it develops [6]. The correct diagnosis can be elusive because anterior knee pain can be due to multiple common etiologies. IPS may lead to chronic, severe, painful saphenous neuritis, hypoesthesia, dysesthesia, reflex sympathetic dystrophy, and/or a painful saphenous neuroma [7, 8, 9, 10].
Pathophysiology
Neuromas were first described by Odier, in 1811, as extremely sensitive bulbous stumps of transected nerves [11]. These lesions may develop as part of the normal reparative process after nerve injury [12, 13]. They typically develop approximately 6–10 weeks after trauma with most presenting within 1–12 months after injury or surgery [12]. Two major types of neuromas have been described: Terminal and spindle neuromas [14]. After disruption of a nerve, Wallerian degeneration of the axon distal to the injury occurs. In an attempt to restore continuity, Schwann cells of the distal portion of the nerve proliferate creating a tunnel into which the proximal axons grow. A partial or total avulsion of the nerve is followed by axonal growth. A terminal neuroma is characterized by a bulbous tangle of sprouting axons resulting from this process [11]. In contrast, spindle neuromas are found in a peripheral nerve after microtrauma from stretching or compression by local scar tissue [12]. Pain from a neuroma may be secondary to traction on the nerve by scar tissue [15], compression of the sensitive nerve endings by adjacent soft tissues [16], nerve ischemia [17], or ectopic foci of ion channels eliciting neuropathic pain [18, 19]. Peripheral upregulation of various ion channels and receptors (sodium channels, TRPA1, CGRP, alpha-1C receptors, and nerve growth factor) may also contribute to the neuropathic pain [19, 20, 21, 22, 23].
Case Report
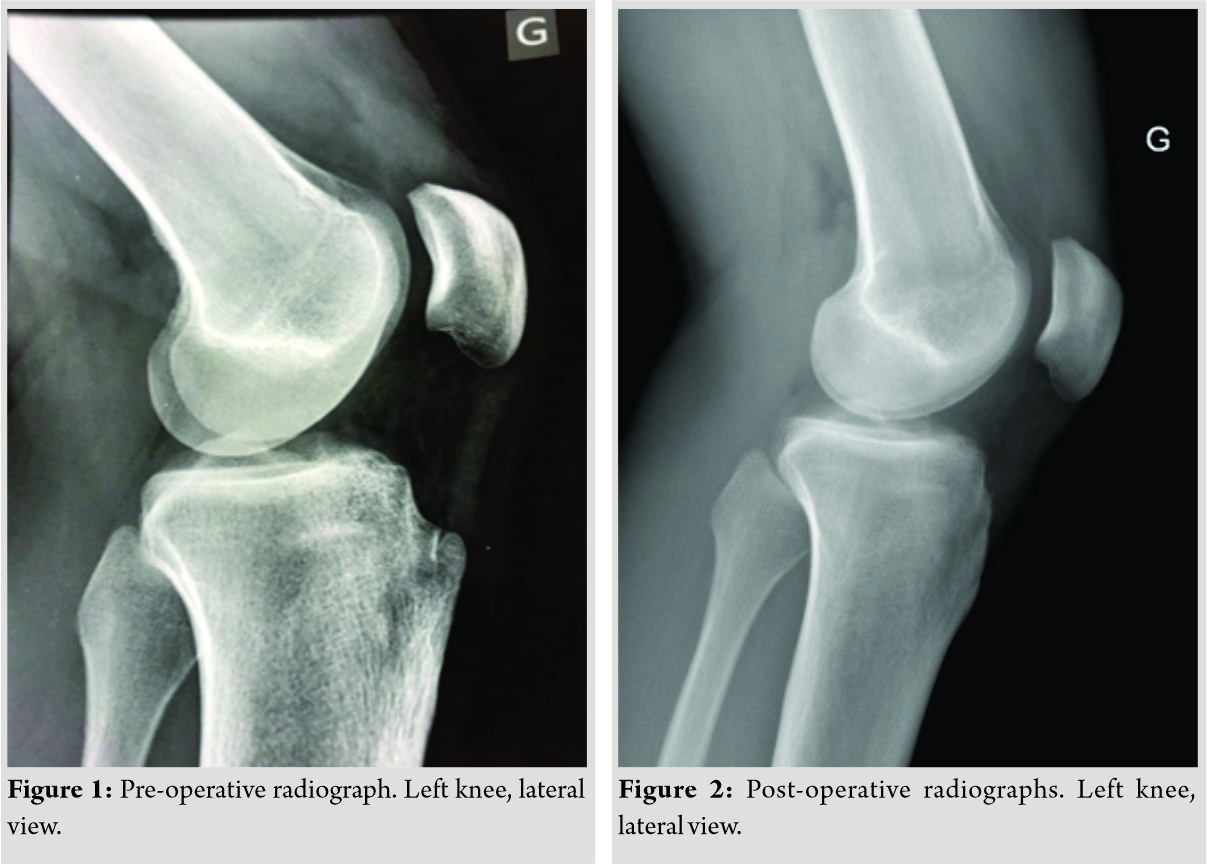
A 20-year-old patient initially presented with a long duration of anterior knee pain which was worse on kneeling, squatting, walking downhill, and also in sports participation (snowboarding). The patient underwent tibial tuberosity exostectomy through a midline incision at another institution and had excellent initial pain relief. Pre-operative radiographs (Fig. 1) demonstrated a prominent tibial tuberosity but no other pathology. Post-operative radiographs demonstrate the appearances after tibial tuberosity exostectomy (Fig. 2).
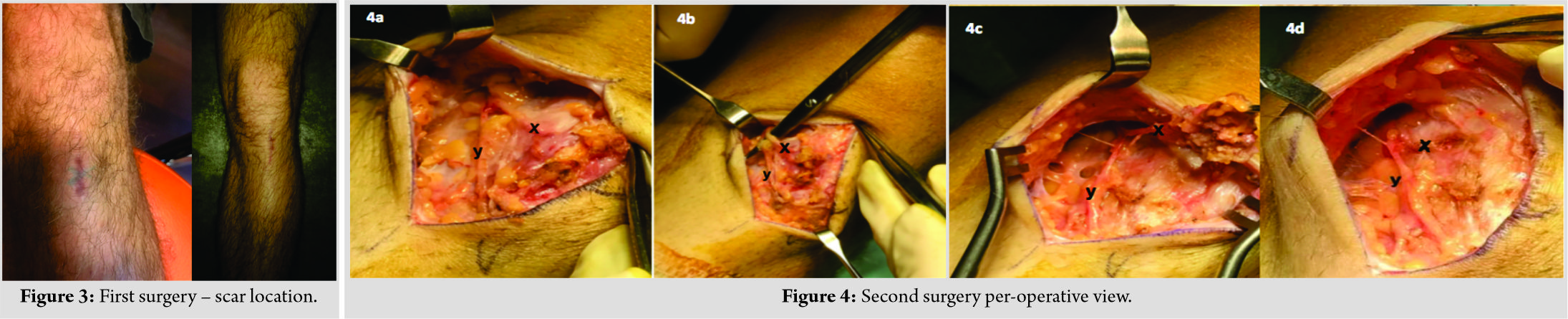
A few weeks after the tibial tuberosity exostectomy, the patient noted pain localized to the anteromedial region of the knee joint, at the surgical scar (Fig. 3), that was different in character to the pre-operative symptoms. He presented to our institution where it was noted that the pain was present even at rest and that there was no history of injury or significant trauma to the knee. Physical examination revealed features of allodynia with increased pain even on light palpation, dysesthesia, and a positive Tinel’s test at the scar (Fig. 3). The patient complained of pain at the slightest touch that was progressively worsening and restricting activities of daily life and sports participation. Due to a clear clinical localization of neuroma pain to the infrapatellar branch of the saphenous nerve (IBSN) the authors did not consider that a local anesthesia infiltration test was appropriate nor were other investigations such as electromyography, magnetic resonance imaging or ultrasound examination utilized. However, in less obvious cases, they can be considered a useful confirmatory diagnostic modality. Approximately 13 months after the index procedure, a reoperation for microsurgical exploration of the IBSN was performed. The procedure was performed with optical magnification to facilitate identification of branches of the nerve in and around the scar tissue. The two branches of the IBSN were identified (Fig 4a and b). The first branch (X), ending with a neuroma, was neurolyzed and resected with the surrounding scar tissue (Fig 4c). The end of the nerve, after cauterization, was buried deep in healthy tissue (Fig. 4d: X). The second branch was neurolyzed only (Fig. 4 a, b, c: Y). The patient experienced immediate post-operative relief of neuropathic pain. At a final follow-up of 18 months, there was no recurrence of pain. The only sequelae were a residual hypoesthesia of the territory of the resected branch of the IBSN, which was not of concern to the patient.
Discussion
This case report is useful in highlighting two main learning points. The first is a reminder that the saphenous nerve and all of its branches are susceptible to injury and subsequent neuroma formation during surgical incisions placed over the anteromedial aspect of the knee. Kerver et al. highlighted that the high degree of anatomic variability of the IBSN confers a relatively high risk of iatrogenic injury to this structure [24]. The literature reports injury to the IBSN after a wide range of surgical procedures from 9.7% to 21% in total knee arthroplasty [25, 26], 28% after arthroscopic meniscectomy [27], and in 37–86% of patients undergoing arthroscopic anterior cruciate ligament reconstruction [28]. Less frequent reports include injury to the IBSN after resection of the prepatellar bursa, in tibial nailing and retrograde femoral nailing [29, 30]. Particular care is, therefore, required to minimize this risk. Several strategies have been proposed to avoid IBSN injury during surgery, such as transillumination, ultrasonography, blunt dissection, avoidance of tourniquet use, graft harvest with the knee in 90° flexion, or identification and familiarization with safe areas through cadaver studies [24, 31]. Despite these considerations, it is accepted that the IBSN has high anatomic variability and injuries can still occur despite optimum surgical technique [24, 31]. The second key learning point is, therefore, that cauterization and resection of neuromas of the IBSN are a simple and effective procedure for abolishing symptoms. Surgical management is recommended only after a trial of non-operative management which can include the use of nonsteroidal anti-inflammatory drugs, oral gamma-aminobutyric acid analog medications, capsaicin cream, physical therapy modalities, transcutaneous electrical nerve stimulation, oral antidepressant medications, and therapeutic local anesthetic and corticosteroid injections [24, 32]. Surgical management is an excellent option when non-operative treatment fails to yield adequate symptomatic relief. Partial denervation for persistent neuroma pain of the knee is associated with high patient satisfaction and a reduction in their pre-operative pain visual analog score. Follow-up after neurectomy is associated with very good patient satisfaction and there appears to be no difference in outcome whether the follow-up period is greater or less than 2 years [33].
Conclusion
The IBSN is at high risk of iatrogenic damage during any surgery on the anteromedial aspect of the knee, especially when longitudinal incisions are used. It is important to be familiar with the pathophysiology, anatomy, diagnosis, and treatment of IPS. Diagnosis is clinical and early recognition and microsurgical treatment should greatly decrease the suffering and disability that occurs when the proper diagnosis has not been made. This report describes successful surgical management of a painful IBSN neuroma that was caused by a midline incision. IBSN neurectomy resulted in full resolution of pain. This report confirms that dissection and excision of neuromas of the IBSN can be useful treatment modality.
Clinical Message
Neuromas of the IBSN can occur after direct trauma or surgical approaches to the anterior aspect of the knee. Microsurgical neurolysis is a useful treatment modality associated with complete resolution of pain and high patient satisfaction.
References
1. Worth RM, Kettelkamp DB, Defalque RJ, Duane KU. Saphenous nerve entrapment. A cause of medial knee pain. Am J Sports Med 1984;12:80-1.
2. Arthornthurasook A, Gaew-Im K. Study of the infrapatellar nerve. Am J Sports Med 1988;16:57-9.
3. Le Corroller T, Lagier A, Pirro N, Champsaur P. Anatomical study of the infrapatellar branch of the saphenous nerve using ultrasonography. Muscle Nerve 2011;44:50-4.
4. Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop Relat Res 1995;320:88-94.
5. Grabowski R, Gobbi A, Zabierek S, Domzalski ME. Nonspecific chronic anteromedial knee pain neuroma as a cause of infrapatellar pain syndrome: Case study and literature review. Orthop J Sports Med 2018;6:2325967117751042. Doi:10.1177/2325967117751042.
6. Pendergrass TL, Moore JH. Saphenous neuropathy following medial knee trauma. J Orthop Sports Phys Ther 2004;34:328-34.
7. Morganti CM, McFarland EG, Cosgarea AJ. Saphenous neuritis: A poorly understood cause of medial knee pain. J Am Acad Orthop Surg 2002;10:130-7.
8. Poehling GG, Pollock FE Jr. Koman LA. Reflex sympathetic dystrophy of the knee after sensory nerve injury. Arthroscopy 1988;4:31-5.
9. Nahabedian MY, Johnson CA. Operative management of neuromatous knee pain: Patient selection and outcome. Ann Plast Surg 2001;46:15-22.
10. Figueroa D, Calvo R, Vaisman A, Campero M, Moraga C. Injury to the infrapatellar branch of the saphenous nerve in ACL reconstruction with the hamstrings technique: Clinical and electrophysiological study. Knee 2008;15:360-3.
11. Provost N, Bonaldi VM, Sarazin L, Cho KH, Chhem RK. Amputation stump neuroma: Ultrasound features. J Clin Ultrasound 1997;25:85-9.
12. Henrot P, Stines J, Walter F, Martinet N, Paysant J, Blum A, et al. Imaging of the painful lower limb stump. Radiographics 2000;20 Spec No:S219-35.
13. Wu KK. Morton’s interdigital neuroma: A clinical review of its etiology, treatment, and results. J Foot Ankle Surg 1996;35:112-9.
14. Rajput K, Reddy S, Shankar H. Painful neuromas. Clin J Pain 2012;28:639-45.
15. Thomas AJ, Bull MJ, Howard AC, Saleh M. Peri operative ultrasound guided needle localisation of amputation stump neuroma. Injury 1999;30:689-91.
16. Fisher GT, Boswick JA Jr. Neuroma formation following digital amputations. J Trauma 1983;23:136-42.
17. Mathews GJ, Osterholm JL. Painful traumatic neuromas. Surg Clin North Am 1972;52:1313-24.
18. Gold MS, Weinreich D, Kim CS, Wang R, Treanor J, Porreca F, et al. Redistribution of na(V)1.8 in uninjured axons enables neuropathic pain. J Neurosci 2003;23:158-66.
19. Lai J, Porreca F, Hunter JC, Gold MS. Voltage-gated sodium channels and hyperalgesia. Annu Rev Pharmacol Toxicol 2004;44:371-97.
20. Hagenacker T, Ledwig D, Büsselberg D. Feedback mechanisms in the regulation of intracellular calcium ([Ca2+]I) in the peripheral nociceptive system: Role of TRPV-1 and pain related receptors. Cell Calcium 2008;43:215-27.
21. Bałkowiec-Iskra E, Vermehren-Schmaedick A, Balkowiec A. Tumor necrosis factor-α increases brain-derived neurotrophic factor expression in trigeminal ganglion neurons in an activity-dependent manner. Neuroscience 2011;180:322-33.
22. Dawson LF, Phillips JK, Finch PM, Inglis JJ, Drummond PD. Expression of α1-adrenoceptors on peripheral nociceptive neurons. Neuroscience 2011;175:300-14.
23. Zoga V, Kawano T, Liang MY, Bienengraeber M, Weihrauch D, McCallum B, et al. KATP channel subunits in rat dorsal root ganglia: Alterations by painful axotomy. Mol Pain 2010;6:6.
24. Kerver AL, Leliveld MS, den Hartog D, Verhofstad MH, Kleinrensink GJ. The surgical anatomy of the infrapatellar branch of the saphenous nerve in relation to incisions for anteromedial knee surgery. J Bone Joint Surg Am 2013;95:2119-25.
25. Sundaram RO, Ramakrishnan M, Harvey RA, Parkinson RW. Comparison of scars and resulting hypoaesthesia between the medial parapatellar and midline skin incisions in total knee arthroplasty. Knee 2007;14:375-8.
26. Borley NR, Edwards D, Villar RN. Lateral skin flap numbness after total knee arthroplasty. J Arthroplasty 1995;10:13-4.
27. Johnson RJ, Kettelkamp DB, Clark W, Leaverton P. Factors effecting late results after meniscectomy. J Bone Joint Surg Am 1974;56:719-29.
28. Tifford CD, Spero L, Luke T, Plancher KD. The relationship of the infrapatellar branches of the saphenous nerve to arthroscopy portals and incisions for anterior cruciate ligament surgery. An anatomic study. Am J Sports Med 2000;28:562-7.
29. Ogilvie-Harris DJ, Gilbart M. Endoscopic bursal resection: The olecranon bursa and prepatellar bursa. Arthroscopy 2000;16:249-53.
30. Lefaivre KA, Guy P, Chan H, Blachut PA. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma 2008;22:525-9.
31. Trescot AM, Brown MN, Karl HW. Infrapatellar saphenous neuralgia diagnosis and treatment. Pain Physician 2013;16:E315-24.
32. Harris JD, Fazalare JJ, Griesser MJ, Flanigan DC. Infrapatellar branch of saphenous neurectomy for painful neuroma: A case report. Am J Orthop (Belle Mead NJ) 2012;41:37-40.
33. Dellon AL, Mont MA, Mullick T, Hungerford DS. Partial denervation for persistent neuroma pain around the knee. Clin Orthop Relat Res 1996;329:216-22.
 |
 |
 |
 |
 |
 |
| Dr. Cedric Ngbilo | Dr. Eric Choudja Ouabo | Dr. Biljana Jovanovic | Dr. Adnan Saithna | Dr. Laurent Gillain | Dr. Bertrand Sonnery Cottet |
| How to Cite This Article: Ngbilo C, Choudja Ouabo E, Jovanovic B, Saithna A, Gillain L, Sonnery-Cottet B. Partial Denervation for Neuroma Pain after Knee Anterior Tibial Tuberosity Exostectomy: A Case Report. Journal of Orthopaedic Case Reports 2019 Jul-Aug; 9(4): 10-13. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com