[box type=”bio”] Learning Point of the Article: [/box]
The atypical proximal-medial, distal-lateral PT rupture pattern seen after bone-patella tendon-bone graft harvest for ACL reconstruction is technically challenging, which we’ve effectively addressed with our novel technique that allows for aggressive postoperative rehabilitation.
Case Report | Volume 9 | Issue 4 | JOCR July-August 2019 | Page 34-40 | Micah Lissy, Urvi J Patel. DOI: 10.13107/jocr.2019.v09i04.1468
Authors: Micah Lissy[1],[2], Urvi J Patel[2]
[1]Department of Orthopaedics, United Health Services Sports Medicine, Vestal, New York, USA,
[2]Department of Orthopedic Surgery, State University of New York Upstate Medical University, Syracuse, New York, USA.
Address of Correspondence:
Dr. Micah Lissy,
4433 Vestal Parkway, Vestal, New York 13850, USA.
E-mail: Micah_Lissy@uhs.org
Abstract
Introduction: A rare cause of patellar tendon (PT) ruptures is complications after bone-PT-bone (BPTB) graft harvest for anterior cruciate ligament (ACL) reconstruction. The atypical tear pattern in these patients can be technically challenging to address.
Description of Technique: A Krackow suture fixation of the medial, tibial based PT was fixed with a knotless suture anchor to the patella. A Krackow suture fixation of the lateral, patella based PT was fixed with a knotless suture anchor to the tibia. Fiber Tape was used for an Internal Brace.
Patient and Methods: We retrospectively reviewed a single patient with a proximal-medial and distal-lateral PT rupture following BPTB graft harvest for an ACL reconstruction. The described repair technique was used to repair the PT rupture. Follow-up was 6-months. Range of motion (ROM), functional outcome scores, and patient-reported outcomes were assessed and recorded.
Results: Six-months postoperatively, the patient has regained full knee extension and flexion to 130 degrees. The patient has good quadriceps strength, and manual muscle testing shows no deficits in the operative leg. The patient is able to perform all of her activities of daily living and is discharged from physical therapy.
Conclusion: We describe a novel technique that effectively repairs the atypical PT rupture pattern seen after ACL reconstruction using BPTB autograft. This technique allows for aggressive post-operative rehabilitation in ROM and strengthening.
Level of Evidence: Level V.
Keywords: Patellar tendon rupture, anterior cruciate ligament harvest, repair technique.
Introduction
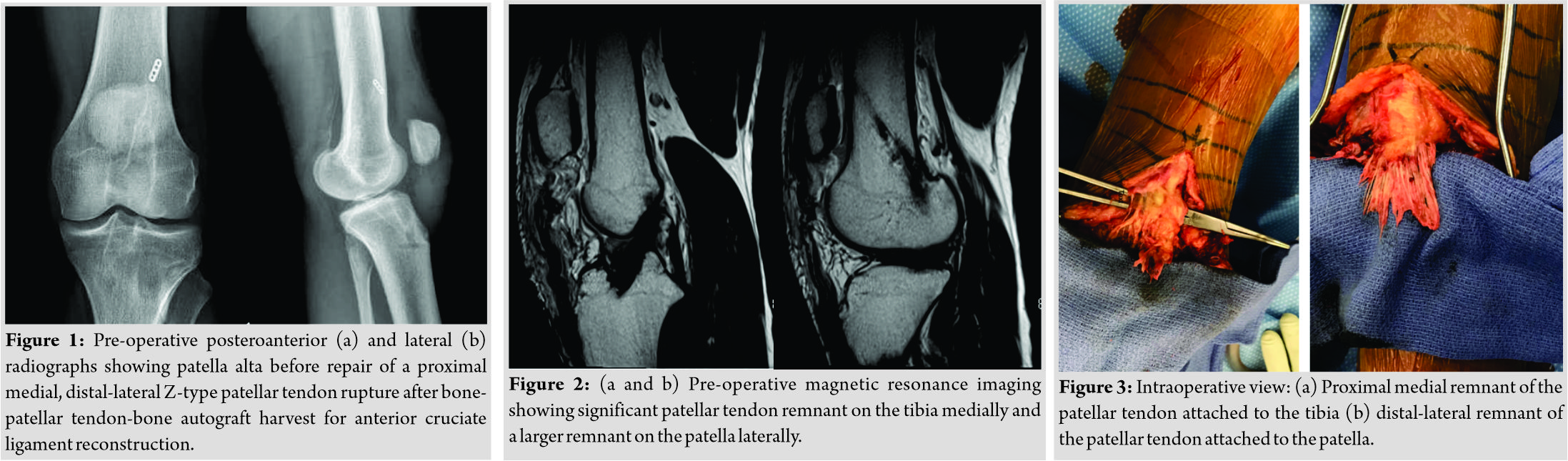
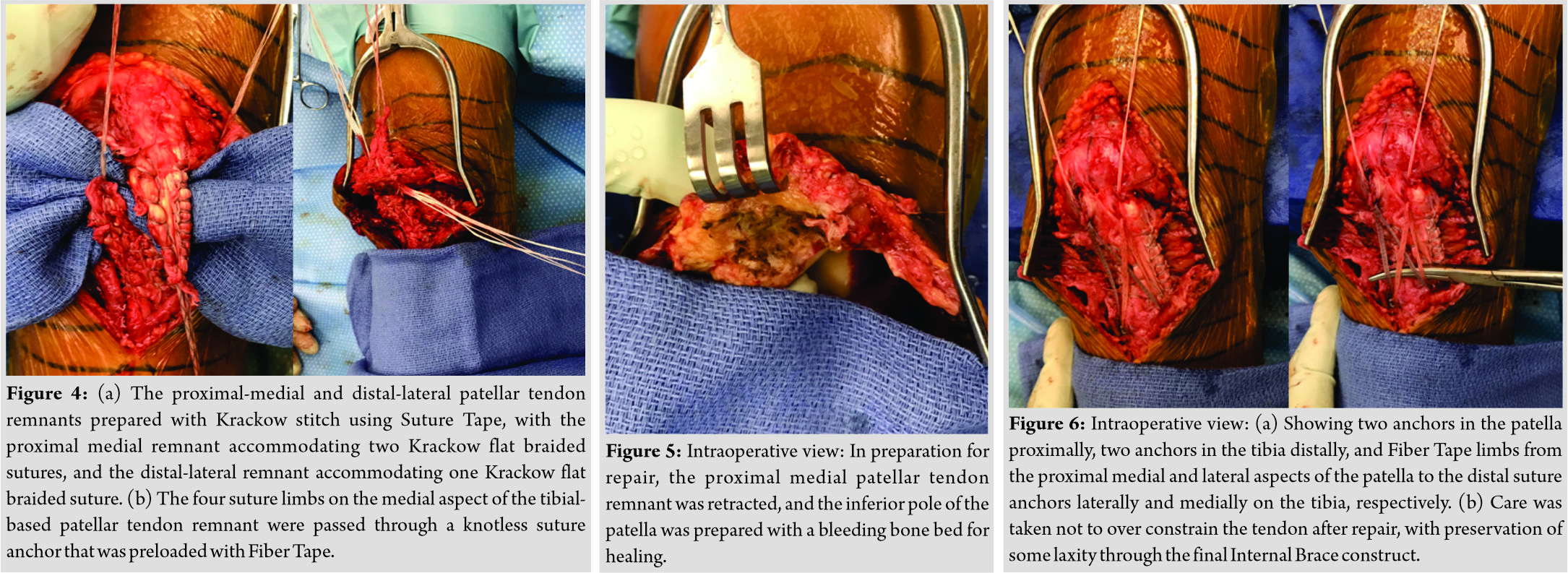
A rare cause of patellar tendon (PT) ruptures is post-operative complications after bone-PT-bone (BPTB) graft harvest for anterior cruciate ligament (ACL) reconstructions. A PT rupture is an injury to the extensor mechanism of the knee; it most often presents in middle-aged adults. Acute rupture is often secondary to a rapid eccentric force of the quadriceps against a partially flexed knee [1, 2, 3, 4, 5]. Tendon ruptures have been long associated with several underlying risk factors and medical comorbidities [1, 2, 3, 4]. These may include, but are not limited to, diabetes mellitus, systemic lupus erythematosus, chronic kidney disease, repetitive microtrauma, previous knee surgery, and chronic corticosteroid injections [3, 4, 6]. The treatment of choice for complete PT ruptures is surgical repair [1, 3]. Poor blood supply and high mechanical loads compromise the operative success of even native PT repairs, making the optimal surgical technique unclear [2, 5, 6]. PT ruptures after BPTB graft harvest for ACL reconstructions are a rare, and technically demanding surgical challenge. Following BPTB harvest for ACL reconstruction, there exists a defect in the central one-third of the native PT [7, 8]. Before consideration for harvest, an adequate PT width of approximately 30 mm for a desired 10 mm tendon harvest should be substantiated [8]. These considerations are vital to ensure adequate tendon remains both medially and laterally post-harvest. It stands to reason that if the harvest was angled and deviated from the central third of the tendon, the risk of rupture would increase. Ruptures may be secondary to focal necrosis of the proximal tendon due to excessive tension if defect closure occurred, loss in tensile strength of the remaining tendon due to reduced tendon mass, interrupted vascular supply, or purely mechanical reasons [7, 9, 10]. Common tears that have been described in the literature include a proximal, intra-substance, or distal pattern for native PT ruptures. However, PT ruptures that occur after a BPTB harvest for ACL reconstruction commonly occur in a proximal medial, distal-lateral tear pattern [8]. While there exists a multitude of techniques for the acute repair of native PT ruptures, none adequately address the complicated nature of a PT rupture secondary to post-operative complications from BPTB graft harvest for ACL reconstructions. The most common repair techniques for the native PT rupture include the standard transosseous approach and the suture anchor approach. However, these approaches come with complications including gap formation and anchor stripping. To address these complications, novel techniques, such as the knotless suture anchor, internal brace construct, and combination suture techniques, have recently been published [1, 2, 4, 5, 6, 11, 12]. There is a paucity of literature regarding PT ruptures after BPTB graft harvest for ACL reconstructions. The methods that have been described in the literature come with drawbacks. For example, the Dall-Miles cable technique for augmentation of PT rupture repair necessitates an additional surgical procedure for removal and is often complicated by cable breakage. We report the case of a 23-year-old female, former Division III basketball athlete, with a PT rupture 2 years after a BPTB ACL reconstruction due to a fall from her bicycle. Physical exam showed a large effusion, palpable defect inferior to the patella, patella Alta on clinical exam and lateral X-ray, and no active extension of the leg (Fig. 1). Magnetic resonance imaging was obtained and revealed disruption of the PT (Fig. 2). The purpose of this study is to describe a novel repair technique for the proximal medial and distal-lateral pattern PT rupture.
Surgical technique
The patient was positioned appropriately and draped. The tourniquet was inflated and an 18 cm midline incision was made which incorporated and excised the previous incision. The correct fascial plane overlying the tendon and paratenon was identified, and flaps were elevated both medially and laterally. The remnants of the tendon were cleared of all scar tissue to adequately achieve exposure. The tendon remnants were then thoroughly interrogated to identify the appropriate reduction, similar to fracture care.
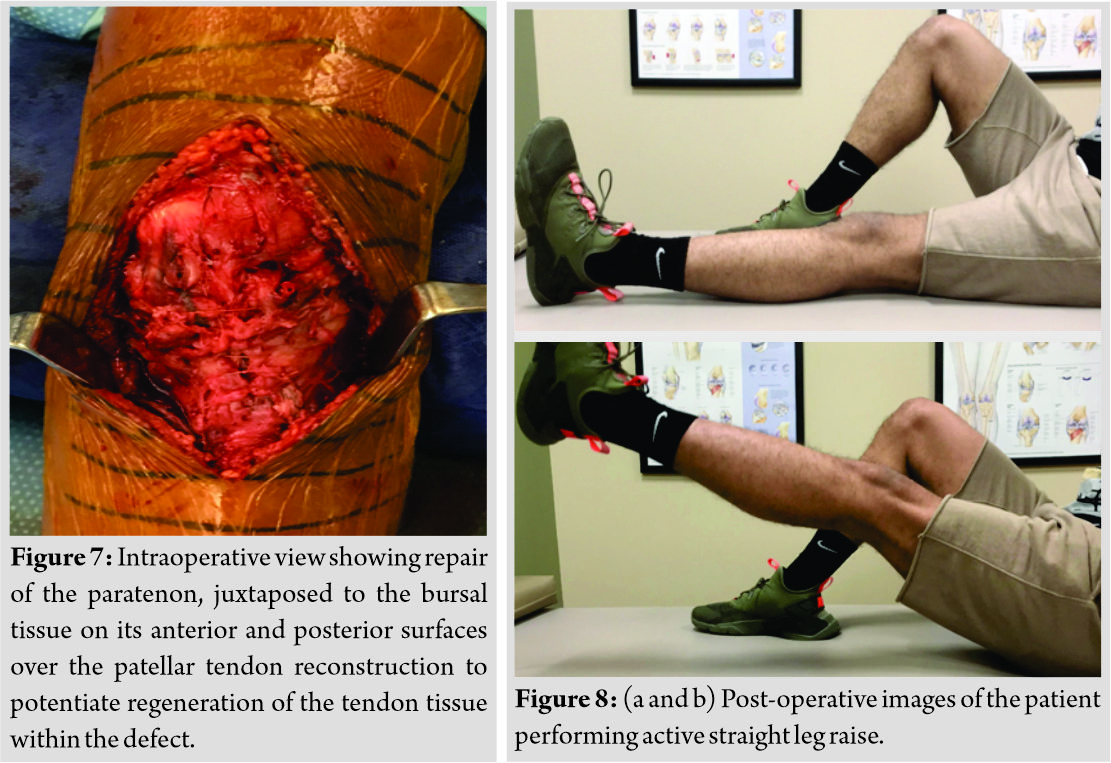
On examination, the PT was found to have ruptured medially off of the patella and laterally off of the tibial tubercle in an angulated fashion, as previously described (Fig. 3) [13]. Using SutureTape (Arthrex, Naples, F1), Krackow whipstitch of the medial tibial based PT was performed. Of note, the angulated nature of the rupture presented with a larger medial segment as compared to the lateral-patella based segment and was able to accommodate two Suture Tape limbs along its width while laterally only one Krackow suture was possible (Fig. 4). A bleeding bone bed was then created on the medial aspect of the patella to improve healing and reattachment of the tendon to the patella (Fig. 5). The same process was repeated on the bone at the lateral aspect of the tibial tubercle.
The first anchor, preloaded with Tiger Tape for internal brace fixation, was drilled and tapped deep to the lateral tendon remnant on the patella. Before anchor insertion, a lateral X-ray was performed at 30 degrees of knee flexion to confirm the appropriate length of the tendon.
One limb from each Suture Tape from the medial, tibial-based tendon remnant was passed through the suture anchor and secured with insertion for a knotless fixation lateral to the patella. Care was taken to ensure appropriate length was maintained during fixation. A small rent through the tendon just off the patella was then created, and the two strands of the Tiger Tape were pulled through.
The second anchor, again preloaded with Fiber Tape for internal brace fixation, was drilled and tapped at the medial patella. The remaining medial, tibial-based Suture Tapes were then passed through the anchor and secured through the lateral drill hole for knotless fixation of the PT to the medial patella. This effectively spread the fixation among two anchors proximally. Two holes were then drilled and tapped at the most proximal insertion of the tibial tubercle on the medial and lateral edges. Care was taken to avoid over constraining the internal brace while maintaining the appropriate length of the PT. One limb from the Fiber Tape and Tiger Tape and both limbs of the Suture Tape from the lateral patella-based tendon were then passed through the third anchor and secured at the lateral insertion of the tendon on the tibial tubercle. The remaining limbs of the Fiber Tape and Tiger Tape from the medial patella were passed through the final anchor and secured at the medial aspect of the tibial tubercle (Fig. 6). We then used the Fiber Wire from our proximal anchor to incorporate both the medial and lateral PT segments together. The integrity of the repair and possibility of over tensioning was evaluated and ruled out. There was no evidence of pull-off of the tendon, and excellent fixation was noted. The paratenon was then repaired in a running fashion with absorbable suture (Fig. 7). The wound was closed in layers, and the patient was placed in a sterile compressive dressing, and a hinged knee immobilizer locked in extension.
Results
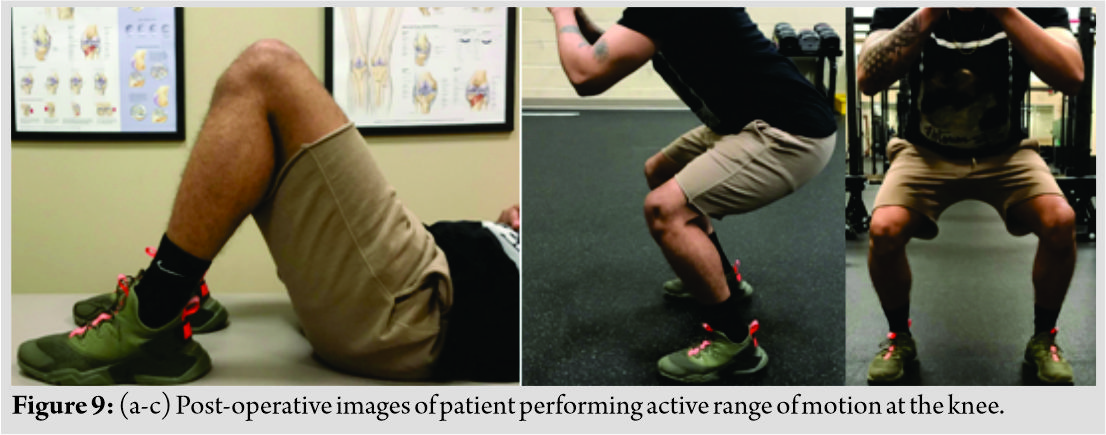
After surgery, the patient was placed in a knee immobilizer and was maintained as weight-bearing as tolerated for 2 weeks. Following the initial 2-week period postoperatively, the patient was allowed for a limited range of motion (ROM) with slow progression until week 6, after which all restrictions and the brace were removed. Formal rehabilitation for the patient began immediately postoperatively and focused on the restoration of patellofemoral ROM and quadriceps activation. Six months after the operation, the patient had full extension and 130 degrees of flexion in the operated knee. Manual muscle testing of the knee in flexion and extension showed strength to return to 5/5 as compared to the non-operative leg. One-rep maximum with leg press returned to 84% in the operated knee. The anterior reach direction of the Y-balance test was within four of the non-operative leg. Lachman test performed on the operated knee showed a firm endpoint with no laxity. A functional assessment was performed 6 months postoperatively. The patient’s focus on therapeutic outcomes score on intake was at Stage 4, and by discharge from physical therapy (PT) was at Stage 6. Her fear avoidance beliefs questionnaire score improved significantly from an intake score of 45–26 on discharge from physical therapy. Her Knee Injury and Osteoarthritis Outcome Score (KOOS, JR.) went from 100 to 92 from the point of intake to discharge from physical therapy with complaints of mild stiffness on waking in the morning. Her Lower Extremity Functional Scale crosswalk knee score improved significantly from a 39.7 on intake to a 70 on discharge from physical therapy. On discharge from physical therapy, the patient was able to perform all of her activities of daily living without pain or difficulty (Fig. 8 & 9).
Discussion
There are a variety of different techniques that can be utilized for repair of PT ruptures. The surgical technique is generally based on the location of the PT tear, either proximal, midsubstance, or distal [8]. While a majority of native PT ruptures are proximal or midsubstance, ruptures secondary to post-operative complications from BPTB graft harvest for ACL reconstruction are more likely to occur in a proximal-medial, distal-lateral tear pattern as seen in our patient.
Native PT ruptures
The standard repair for native PT ruptures, a transosseous approach, shows high failure rates due to gap formation at the repair site from repetitive loading that result in attenuation of the repair [2, 5]. Recent studies have described a suture anchor repair that demonstrates an almost 40% reduced gap formation within cadaveric models and higher ultimate load failures when compared to the standard transosseous repair [1, 5, 6, 11]. Ettinger et al. attributed these findings to longer distance bridging through suture material in the transosseous approach as compared to the suture anchor technique [6]. Bushnell et al. discussed suture anchor advantages such as reduced need for tissue dissection and damage, and a potentially reduced risk of patellar fractures, and intra-articular damage compared to the intraosseous tunnel approach [11]. Additional reported advantages of the suture anchor technique include reduced operation time, higher strength of repair, easily accessible implantation sites, and earlier functional rehabilitation leading to quicker recoveries [4, 6, 11]. However, these studies also describe the risk for suture anchor failure through anchor stripping and anchor cut out that may complicate hardware removal and adjustment after failure [6, 11]. Lanzi et al. compared a knotless anchor technique to the standard transosseous technique in porcine specimens [1]. The study found all transosseous repair specimens to have a failure at the level of the knot that was secured at the proximal patellar pole. The knotless suture anchor group, however, had two modes of failure: Pullout from interference around the anchor in the bone or suture breakage at the level of the first locking throw in the tendon. The authors suggested a potential advantage to their method over the traditional suture anchors as it allows for traction to be placed on both suture limbs sequentially, leading to a reduction of the tendon to bone in an optimal fashion with the threaded anchor. When secured, the anchor functions by holding both sutures between the threaded implant and the bony socket. However, this study failed to compare the knotless suture anchor to the previously described standard suture anchor repair. When compared to recent biomechanical studies that used the standard suture anchor, the maximum load to failure rates was comparable, suggesting that a knotless construct is an equivalent. The most recent literature has described various PT repair techniques such as cortical button suspensory fixation devices, internal brace constructs, and combined suture techniques. Ode et al. demonstrated mechanical advantages over suture and anchor repairs through a cortical button fixation approach in cadaveric studies [5]. The study showed less cyclic gap formation and resistance of twice the load to failure of the construct. However, the study was limited secondary to the utilization of older cadaveric specimens with poor clinical comparison to the more common presentation among younger athletic populations. Rothfeld et al. described the use of a novel knotless suture anchor internal brace with suture tape (SAIB) technique for mid substance PT repairs [12]. The study established that PT repair with augmentation with SAIB is biomechanically superior to a non-augmented repair and equivalent to augmentation with 18-gauge steel wires. However, this study specifically evaluated augmentation of midsubstance PT ruptures in human cadaveric knee specimens that were artificially created and failed to discuss technique application to the more common proximal tendon ruptures seen in the native tendon. Sanchez et al. described a PT repair through an internal brace construct with unicortical buttons and suture tape [2]. The study ascertains that their technique disperses tension and distributes it along the posterior aspect of the anterior tibial cortex allowing for complementary strength and maintenance of the reduced PT. However, limitations of this technique include the inability to use the approach for distal ruptures of the PT and an increased risk of patellar fracture secondary to the compromised bone integrity from the transosseous tunneling. Gaines et al. described a combined suture technique with suture anchors and a Krackow-Bunnell Weave that requires minimal dissection [4]. The authors of this study highlighted minimal exposure of only the tendon, retinaculum, and inferior pole of the patella. The study surmised that the Krackow suture loops in conjunction with the Bunnell suture loops allow for multi-planar tension distribution with decreased pull-through stresses throughout the tendon. While the technique bypasses drilling of tunnels, it is not recommended for PT tears that are associated with avulsion fractures due to the use of suture anchors being dependent on an intact cortex.
PT ruptures after BPTB ACL reconstruction
While there exists a multitude of techniques for the repair of native PT disruptions, none adequately address the complicated nature of a PT rupture secondary to post-operative complications from a BPTB graft harvest for ACL reconstructions. Most of the reported cases are described in the early post-operative period of 0–6 weeks; however, there are rare occurrences of injury years after ACL reconstruction [10]. For PT ruptures in the early post-operative period, there lies a significant risk of interrupting and delaying a patient’s rehabilitation which can compromise the overall outcome of the initial ACL reconstruction. This constitutes the necessity for a PT rupture reconstruction method that allows for aggressive rehabilitation in the post-operative period. Most of the PT ruptures after BPTB graft harvest for ACL reconstructions are seen to have occurred in the first 10 months after surgery [7, 10]. Of note, a majority of the ruptures described in literature occurred after a Marshall/MacIntosh procedure in which a wide portion of the prepatellar retinaculum is excised along with the central-third portion of the PT [7, 9]. This method may lead to decreased vascularization or direct damage to the remaining PT attachments [7, 9]. While there have been reported cases of atraumatic PT ruptures after an ACL reconstruction with central-third PT graft harvest, a majority of cases are related to some form of minor trauma such as direct impact, hyperflexion injury, or forceful quadriceps contraction. The quality and quantity of the remaining PT tissue with which the donor site defect heals are important in determining the remaining strength of the tendon [7]. Repair methods in regard to the soft tissue defect include repairing both the PT and the paratenon defects; repairing only the PT defect; repairing only the paratenon defect; or leaving both the PT and paratenon unrepaired [8]. The paratenon is juxtaposed to the bursal tissue on its anterior and posterior surfaces, and thus exhibits the potential to regenerate the tendon tissue within the defect [7]. The surgical technique that we describe for a proximal medial, distal-lateral repair includes surgical repair of the paratenon. There have been many studies in the recent literature regarding the closure of the PT defect after BPTB graft harvest for ACL reconstruction. Histologically, the tissue growth in the non-reconstructed defect does not resemble normal tendon, but rather scar tissue made of poorly oriented collagen fibers [7, 8]. Aggressive scar tissue reaction with disorganized collagen networks may be secondary to exposure of the original tendon substance to stresses leading to overproduction of repair tissue and remodeling of the cross-sectional area [7]. While defect closure may reduce the size of the gap, and therefore scar reaction, the closure has also been noted to be adversely affective to the remaining tendon. The tension in the defect closure may result in avascular degeneration, focal necrosis, and calcification of the proximal remaining tendon, which leads to an increased risk of PT rupture [9]. The techniques reported for the reconstruction of a PT rupture after its central-third has been used for ACL reconstruction, include simple suture of the avulsed PT, suture with augmentation with a semitendinosus and gracilis tendon, and a fascia lata autograft [13, 14]. In a recent retrospective study by Benner et al., patients with PT rupture secondary to ACL graft harvest were surgically repaired by employing a novel suture anchor technique with Dall-Miles Cable augmentation through the patella and tibia [13]. The authors propose that their technique prevents shortening of the PT, with cable augmentation allowing for early mobilization, immediate ROM, and avoidance of complications from patella baja and subsequent loss of knee flexion. However, augmentation with Dall-Miles Cable may not be the ideal approach to repair, as these cables may break and must be removed through an additional surgical procedure 6–8 weeks postoperatively [10, 13]. Repairs of the tendon to the bone may also be augmented with dacron sutures, neutralization wires, cerclage wires, autogenous semitendinosus grafts, and fascia lata strips [10]. In a report by Miroslav et al., BPTB frozen allograft with multiple-wire loop reinforcement was used for reconstruction [14]. The authors secured the donator allograft into the central aspect of the defect where the previous graft was harvested and secured it with two screws. They then ran wire loops from the upper edge of the patella to the tibial tubercle to reinforce the repair, and the remnants of the patellar ligament were sutured. However, as a reported complication with the Benner et al. study, wires and screws had to be removed 6 months post-operation due to breakage. Another disadvantage to use of allografts is the possible risk of disease transmission, infection, and delayed allograft incorporation [14]. Hardin and Bachaugmented PT repair post-BPTB graft harvest for ACL reconstruction with semitendinosus and gracilis tendon autografts [15]. Disadvantages of autograft utilization for PT reconstruction include donor site morbidity, delayed mobilization, and delayed achievement of full ROM [14]. Hardin and Bach also utilized wire augmentation for their autograft reconstructions, which again runs the risk of complications from wire breakage [15].
Conclusion
Our goal for developing a repair technique was one that allows for aggressive post-operative ROM and strengthening while limiting the post-operative immobilization period. In addition, we sought to demonstrate an ideal surgical repair technique for the proximal medial, distal-lateral tear pattern that is most commonly seen in PT ruptures post-BPTB graft harvest for ACL reconstruction, as was seen in our patient. Our preferred method for PT repair after BPTB graft harvest for ACL reconstruction is a Krackow suture fixation of the medial, tibial based PT with a knotless suture anchor to the patella, and a Krackow suture fixation of the lateral, patella based PT with a knotless suture anchor to the tibia. We also utilized Tiger Tape and Fiber Tape for Internal Brace augmentation. Our preferred surgical technique bypasses the common complications that are reported in literature regarding the tear pattern, use of transosseous tunnels, wire or autograft augmentation, and knotted anchor pull out.
Clinical Message
The most commonly seen PT rupture post-BPTB graft harvest for ACL reconstruction is the proximal-medial, distal-lateral tear pattern. These types of PT ruptures are rare and technically demanding surgical challenges. We describe a novel technique that effectively repairs the atypical PT rupture pattern seen after ACL reconstruction using BPTB autograft. This technique bypasses the drawbacks of other previously described repair approaches and allows for aggressive post-operative rehabilitation in ROM and strengthening.
References
1. Lanzi JT Jr., Felix J, Tucker CJ, Cameron KL, Rogers J, Owens BD, et al. Comparison of the suture anchor and transosseous techniques for patellar tendon repair: A biomechanical study. Am J Sports Med 2016;44:2076-80.
2. Sanchez G, Ferrari MB, Sanchez A, Moatshe G, Chahla J, DePhillipo N, et al. Proximal patellar tendon repair: Internal brace technique with unicortical buttons and suture tape. Arthrosc Tech 2017;6:e491-7.
3. Capiola D, Re L. Repair of patellar tendon rupture with suture anchors. Arthroscopy 2007;23:906.e1-4.
4. Gaines RJ, Grabill SE, DeMaio M, Carr D. Patellar tendon repair with suture anchors using a combined suture technique of a krackow-bunnell weave. J Orthop Trauma 2009;23:68-71.
5. Ode GE, Piasecki DP, Habet NA, Peindl RD. Cortical button fixation: A better patellar tendon repair? Am J Sports Med 2016;44:2622-8.
6. Ettinger M, Dratzidis A, Hurschler C, Brand S, Calliess T, Krettek C, et al. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: A cadaveric study. Am J Sports Med 2013;41:2540-4.
7. Marumoto JM, Mitsunaga MM, Richardson AB, Medoff RJ, Mayfield GW. Late patellar tendon ruptures after removal of the central third for anterior cruciate ligament reconstruction. A report of two cases. Am J Sports Med 1996;24:698-701.
8. Frank RM, Tilton AK, Campbell KA, Bach BR. Managing perioperative extensor mechanism injuries and the patellar defect after anterior cruciate ligament reconstruction. Oper Tech Sports Med 2016;24:29-34.
9. Bonamo JJ, Krinick RM, Sporn AA. Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction. A report of two cases. J Bone Joint Surg Am 1984;66:1294-7.
10. Shelbourne KD, Lawrance SE, Kerr B. Patellar tendon rupture after anterior cruciate ligament surgery. Oper Tech Sports Med 2006;14:8-14.
11. Bushnell BD, Byram IR, Weinhold PS, Creighton RA. The use of suture anchors in repair of the ruptured patellar tendon: A biomechanical study. Am J Sports Med 2006;34:1492-9.
12. Rothfeld A, Pawlak A, Liebler SA, Morris M, Paci JM. Patellar tendon repair augmentation with a knotless suture anchor internal brace: A biomechanical cadaveric study. Am J Sports Med 2018;46:1199-204.
13. Benner RW, Shelbourne KD, Urch SE, Lazarus D. Tear patterns, surgical repair, and clinical outcomes of patellar tendon ruptures after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med 2012;40:1834-41.
14. Milankov Ziva M, Semnic R, Miljković N, Harhaji V. Reconstruction of patellar tendon rupture after anterior cruciate ligament reconstruction: A case report. Knee 2008;15:419-22.
15. Hardin G, Bach BR. Distal rupture of the infrapatellar tendon after use of its central third for anterior cruciate ligament reconstruction. Am J Knee Surg 1992;5:140-3.
 |
 |
| Dr. Micah Lissy | Ms. Urvi J Patel |
| How to Cite This Article: Lissy M, Patel U J. Surgical Technique: Repair of Patella Tendon Rupture in a Previously Harvested Tendon for an Anterior Cruciate Ligament Reconstruction. Journal of Orthopaedic Case Reports 2019 Jul-Aug; 9(4): 34-40. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com