[box type=”bio”] Learning Point of the Article: [/box]
Every orthopaedic practitioner should keep tuberculosis as differential in dealing with posterior element of spine pathology.
Case Report | Volume 9 | Issue 4 | JOCR July-August 2019 | Page 41-43 | S V Sonone, A A Dahapute, S A Keny, N A Marathe, K P Dhole. DOI: 10.13107/jocr.2019.v09i04.1470
Authors: S V Sonone[1], A A Dahapute[1], S A Keny[1], N A Marathe[1], K P Dhole[2]
[1]Department of Orthopedics, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, Maharashtra, India,
[2]Department of Orthopedics, Topiwala National Medical College, Mumbai. Maharashtra, India.
Address of Correspondence:
Dr. S A Keny,
Department of Orthopedics, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital.
E-mail: swapnilakeny@gmail.com
Abstract
Introduction: Spinal Koch involving posterior elements of the neural arch is one of the atypical presentations which are often missed.
Case presentation: A 40-year-old female presented with radiculopathy and bilateral lower limb claudication for 5 months. Radiological investigations showed compressive lesion resembling flavum hypertrophy and a degenerative etiology was thus suspected. However, histopathology report pointed toward tuberculosis (TB) of the posterior elements (atypical form). Management with surgical decompression and anti-Koch treatment gave a successful outcome.
Conclusion: TB affecting posterior elements of spine is a rare entity and needs a high degree of suspicion for accurate diagnosis. Newer radiological interventions such as computed tomography and magnetic resonance imaging along with histopathological evidence will help to clinch the diagnosis of Koch’s spine early before neurological problems or deformity sets in. Keeping a high index of suspicion will help to avoid missing the atypical forms of the disease.
Keywords: Koch’s spine, posterior elements, ligamentum flavum hypertrophy.
Introduction
Spinal tuberculosis (TB) is the most common form of osteoarticular TB and accounts for 50% of all cases of skeletal TB [1]. The thoracolumbar junction is the most common site of involvement [2]. TB spine can present in one of the two patterns: (a) Caseous exudative type; with severe constitutional symptoms and bony destructive changes on radiological examination and (b) granular dry type; without abscess formation or classic bony changes [3]. The above case fits into the second category with insidious onset and no active inflammatory signs of TB. Spinal involvement is usually a result of hematogenous spread of Mycobacterium tuberculosis from primary foci such as lungs, lymph nodes, and gastrointestinal tract [4]. The venous plexus surrounding the spinous, transverse, and articular processes and on the posterior aspect of lamina anastomose freely with the neighboring venous plexuses help infection to reach and lodge in the neural arch[5]. The classical spinal TB is a disease of the vertebral body with the involvement of the intervertebral disc (spondylodiscitis) [6]. Destruction of two or more adjacent vertebral bodies, destruction of the intervening intervertebral disc and opposing end plates with progressive collapse and kyphosis, and formation of paravertebral or psoas abscess dominate the clinical picture [7]. Due to insufficient emphasis and descriptions in literature, diagnosing atypical spinal TB continues to be difficult, which could lead difficulty in establishing proper diagnosis and to start timely treatment, especially regarding the choice of surgical options. The atypical features of spinal TB may present as the involvement of posterior elements of neural arch(intervertebral disc and vertebral body intact), formation of skip lesions, extradural spinal cord compression without any bony involvement, or lesions involving the sacrum. When posterior spinal TB exists in association with anterior spinal TB at the same level, it is called composite lesion or panvertebral involvement.
Case Presentation
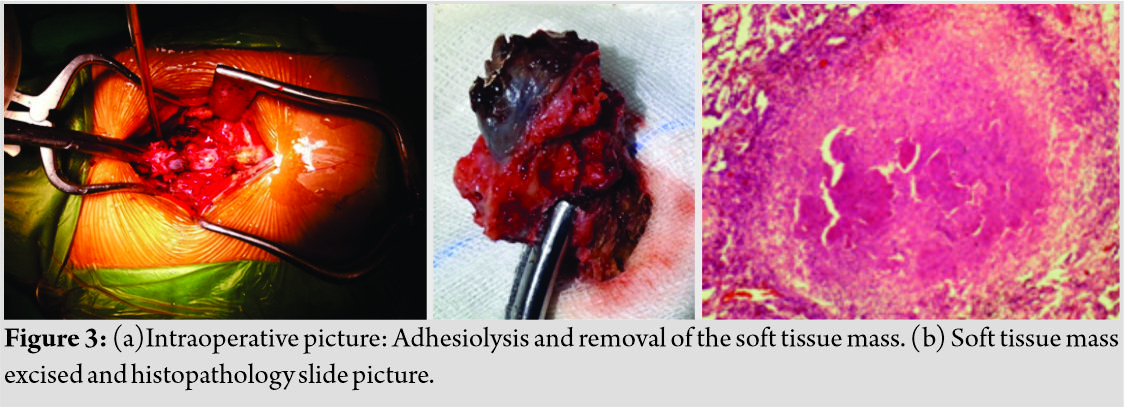
A 40-year-old female presented with a history of radiculopathy and claudication in bilateral lower limbs with a claudication distance of 300 mfor 5 months. She gave a history of intermittent back pain, however, that was not her primary complaint. The patient did not have a history of any constitutional symptoms (fever, weight loss, and evening rise of temperature).There is no history of TB. On clinical examination, there was no local rise of temperature, paraspinal muscle spasm, or local tenderness. Lumbar spine X-ray was normal. Magnetic resonance imaging (MRI)(Fig. 1) revealed ligamentum flavum hypertrophy and a degenerative cause for the low back pain was suspected. 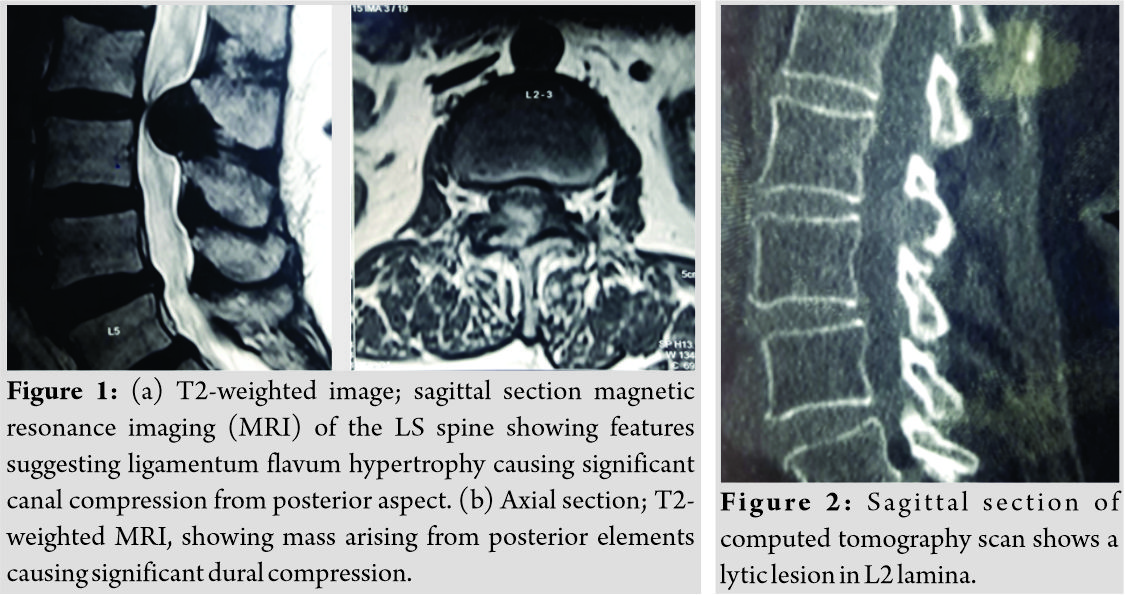
Discussion
Typical clinical features related to posterior spinal TB include a localized bony pain with tenderness in the midline, swelling in the midline or paraspinal area, formation of cold abscess, or sinuses adhered to the underlying bone. Pathology when present closer to the neural structures can give rise to radicular pain and in severe stages progress to paraplegia. Kyphosis or kyphoscoliosis can occur in cases of panvertebral involvement [5]. Our patient presented with midline back pain with radiculopathy and severe claudication. Posterior spine TB is usually associated with high incidence of neurological deficit. Even though the compression is from the posterior aspect of the cord, ironically, we still find that the motor fibers (located anteriorly in the spinal cord) are affected first before the sensory tracks. In general, motor tracks are more susceptible to pressure effects. Furthermore, as the cord is pushed from behind, the anteriorly based motor fibers are compressed against the bony wall of the spinal canal causing neurological injury. Posterior spine TB is infrequently reported in literature. Arora et al. [8] reviewed 24 patients with patients with posterior elements TB without vertebral body involvement. Decompression and laminectomy were performed for patients with neurological involvement and epidural abscess. Narlawar et al.[9]in their study involving 33 patients of posterior elements TB reiterated the usefulness of MRI in diagnosis and assessment of response to treatment. Conventional X-rays have limited role as lesion smaller than 1.5cm is mostly overlooked. The radiographic differentiation from neoplasia may be difficult. MRI features can be positive much before X-ray changes and are especially useful for demonstrating extent of cord compromise and the presence of an extradural granuloma. CT scan is helpful to identify bony destruction, granulation tissue (high signal), and caseous tissue (low signal) [9]. In this case, MRI features were consistent with pathology involving posterior elements mimicking hypertrophy of ligamentum flavum causing obliteration of spinal canal. Although CT scan done preoperatively was helpful to rule out the above condition as it showed no ossification or calcification of the ligament [12]. Due to high incidences of neurological injury, surgical intervention is indicated for debridement, debulking of the lesion, and also for the establishment of the final diagnosis [10]. Histopathological confirmation of TB, as in our patient, helps to establish proper diagnosis and initiate timely and appropriate treatment.
Conclusion
TB is known for being one of the great mimickers in medicine. It is now hoped that with increased knowledge of the atypical forms in literature, there will be an increased suspicion to rule out atypical TB in such situations. Newer radiological interventions (CT scan and MRI) along with histopathological evidence will help to clinch the diagnosis early before neurological problems or deformity sets in.
Clinical Message
TB of posterior elements of the vertebral body should be kept as differential diagnosis in case of low back pain with radiculopathy in lower limb keeping in mind the prevalence of TB in our country. Radiological (MRI) helps to reach diagnosis. Surgery should be kept as management if needed.
References
1. Moon MS. Tuberculosis of spine: Current views in diagnosis and management. Asian Spine J 2014;8:97-111.
2. Jain AK, Kumar J. Tuberculosis of spine: Neurological deficit. Eur Spine J 2013;22 Suppl 4:624-33.
3. Jain AK, Dhammi IK. Tuberculosis of the spine: A review. Clin Orthop Relat Res 2007;460:39-49.
4. Tuli SM. Tuberculosis of te shoulder. In: Tuberculosis of the Skeletal System. 1st ed. New Delhi: JayPee Brothers Medical Publisher (P) Ltd; 1993.
5. Kumar K. Posterior spinal tuberculosis: A review. Mycobact Dis 2017;7:1-4.
6. Yeol LK. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J 2014;8:216-23.
7. Momjian R, George M. Atypical imaging features of tuberculous spondylitis: Case report with literature review. J Radiol Case Rep 2014;8:1-14.
8. Kumar K. Posterior spinal tuberculosis: A review. Mycobact Dis 2017;7:1-4.
9. Arora S, Sabat D, Maini L, Sural S, Kumar V, Gautam VK, et al. Isolated involvement of the posterior elements in spinal tuberculosis: A review of twenty-four cases. J Bone Joint Surg Am 2012;94:e151.
10. Narlawar RS, Shah JR, Pimple MK, Patkar DP, Patankar T, Castillo M. Isolated tuberculosis of posterior elements of spine: Magnetic resonance imaging findings in 33 patients. Spine (Phila Pa 1976) 2002;27:275-81.
11. Al-Khudairi N, Meir A. Isolated tuberculosis of the posterior spinal elements: Case report and discussion of management.J R Soc Med Open 2014;5:2054270414543396.
12. Patnaik S, Jyotsnarani Y, Uppin SG, Susarla R. Imaging features of primary tumors of the spine: A pictorial essay. The Indian journal of radiology & imaging. 2016 Apr;26(2):279.
 |
 |
 |
 |
 |
| Dr. Sandeep V Sonone | Dr. Aditya A Dahapute | Dr. Swapnil A Keny | Dr. Nandan A Marathe | Dr. Kiran P Dhole |
| How to Cite This Article: Sonone S V, Dahapute A A, Keny S A, Marathe N A, Dhole K P. Unusual Presentation of Koch’s Spine Involving Posterior Elements of Vertebra– A Case Report. Journal of Orthopaedic Case Reports 2019 Jul-Aug; 9(4): 41-43. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com