[box type=”bio”] Learning Point of the Article: [/box]
Neglected atlantoaxial dislocation is a rare injury, can be frequently missed, and can be managed by C1-C2 posterior instrumentation with joint remodeling and manipulation.
Case Report | Volume 9 | Issue 4 | JOCR July-August 2019 | Page 80-83 | Kaustubh Ahuja, Pankaj Kandwal, Sanny Singh, Rohit Jain. DOI: 10.13107/jocr.2019.v09i04.1490
Authors: Kaustubh Ahuja[1], Pankaj Kandwal[1], Sanny Singh[1], Rohit Jain[1]
[1]Department of Orthopaedic Surgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Address of Correspondence:
Dr. Pankaj Kandwal,
Department of Orthopaedic Surgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand – 249 203, India.
E-mail: pankajkandwal27@gmail.com
Abstract
Introduction: In atlantoaxial context, spondyloptosis has been defined as a situation when both the inferior facets of atlas are fixed anterior to the superior facets of axis. Such an injury scenario is a rare presentation with a few reported cases in available literature.
Case Report: We present a case of post-traumatic anterior atlantoaxial dislocation or spondyloptosis associated with a Type 2 odontoid fracture in an adult patient who presented to us 3 months after injury. After failed attempts of closed reduction with traction, open reduction and posterior instrumentation with fusion were done using joint remodeling technique. 6-month follow-up showed completely reduced facet joints with near complete fusion.
Conclusion: Long-standing complete C1-C2 dislocations pose a challenge for a surgeon because of the associated difficulty in joint reduction. Joint remodeling and manipulation have antiquated transoral odontoidectomy as excellent results have been achieved by direct posterior approach.
Keywords: Atlantoaxial dislocation, odontoid fracture, spondyloptosis
Introduction
Spondyloptosis is defined as complete slippage of a vertebral body over the vertebra below it. In atlantoaxial context, spondyloptosis has been defined as a situation when both the inferior facets of atlas are fixed anterior to the superior facets of axis [1]. Such an injury scenario is a rare presentation with a few reported cases in available literature. Moreover, most cases of atlantoaxial dislocation have a rotational component primarily caused in young patients with Down’s syndrome, rheumatoid arthritis, or cervical vertebral anomalies [2, 3]. We present a case of post-traumatic anterior atlantoaxial dislocation or spondyloptosis associated with a Type 2 odontoid fracture in an adult patient who presented to us 3 months after injury.
Case Report
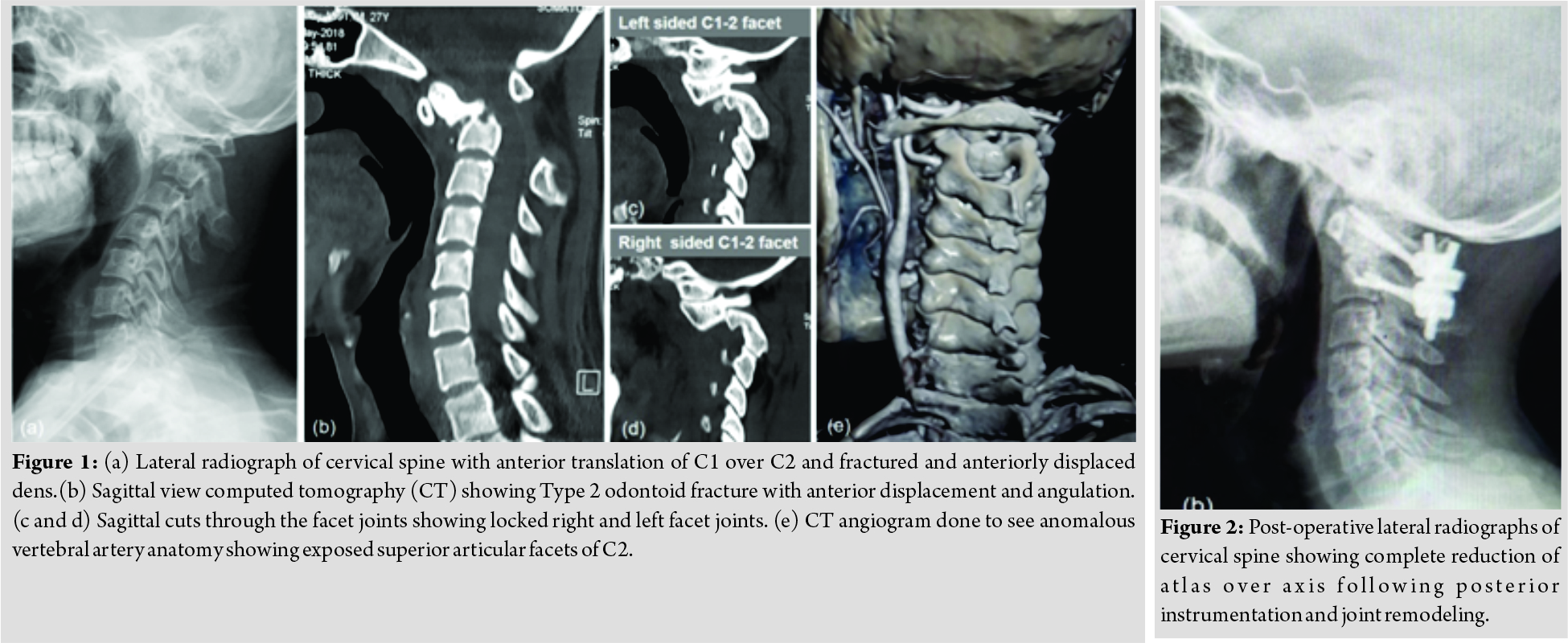
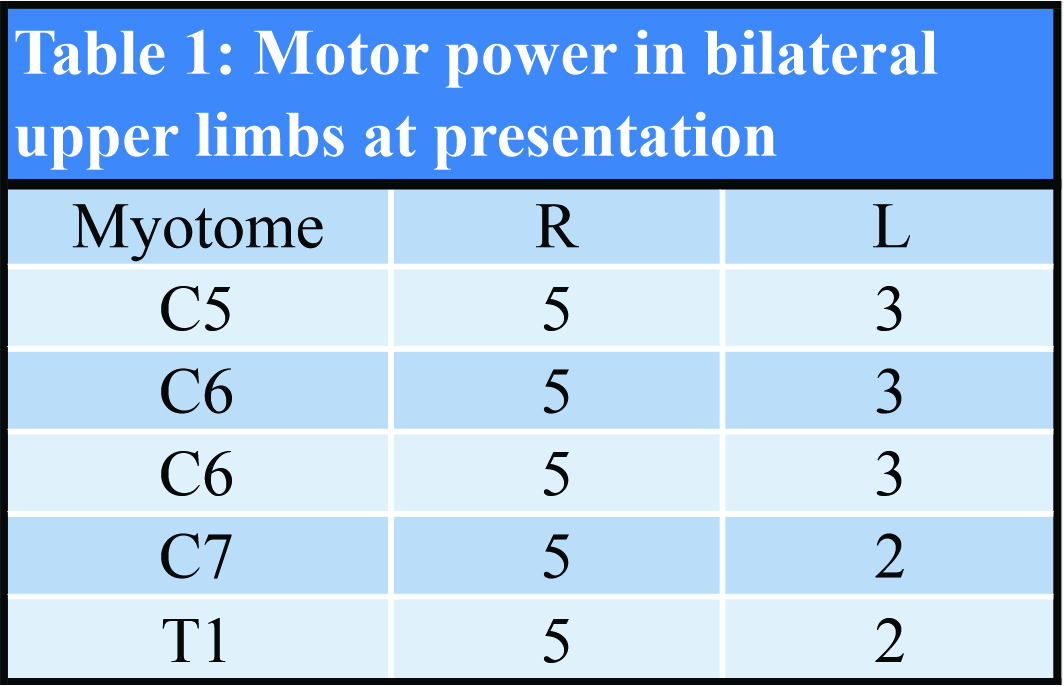
A 25-year-old male suffered from a fall over 100 feet in a bus from a cliff. He was managed in a local hospital with humerus plating for fracture of humerus shaft. The patient presented to us 3 months later following inability to extend his neck and new-onset weakness in left upper limb. On examination, the patient was found to have monoparesis of left upper limb along with upper motor neuron lesion signs including bilateral ankle clonus and exaggerated deep tendon reflexes. Motor power in bilateral upper limbs is depicted in Table 1. Onradiological evaluation, the patient was diagnosed to have anteriorly displaced Type 2 odontoid fracture with complete dislocation of atlas over axis such that bilateral atlas inferior facets were locked anterior of axis superior facets (Fig. 1). Skull traction was applied in the pre-operative period with sequential weight incrementation upto 10 kgs but the facet joint reduction was not achieved. Subsequently, open reduction and posterior fixation was were planned.
Operative procedure
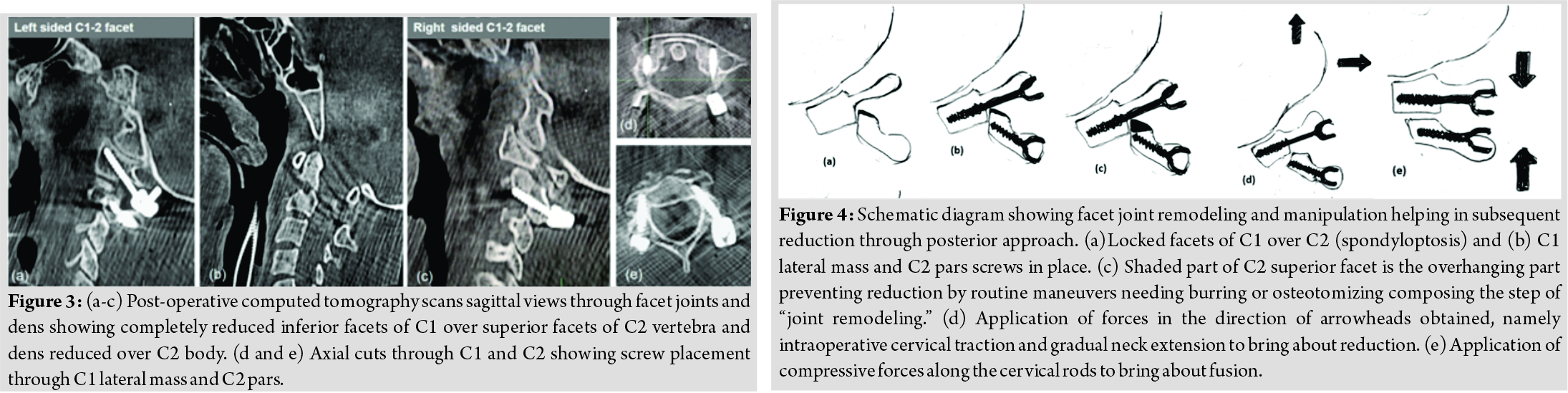
The patient was placed prone in OT table on Mayfield traction under intraoperative neuromonitoring (IONM) support. Posterior midline incision was used to expose inferior aspect of C1 and C2. Bilateral C2 nerve roots were preserved. C1 inferior facets were not visible. Bilateral superior facets of C2 were encountered first. Partially threaded polyaxial C1 lateral mass screws were placed bilaterally by carefully retracting C2 ganglion and nerve root caudally (Fig. 2 and 3). C2 pars screw were placed, and high-speed burr was used to burr out overriding superior facets of axis after retracting the nerve root cephalad. Intraoperatively axial traction and careful neck extension manoeuvre was done to achieve reduction, and rods were connected (Fig. 4). This was followed by decortication of inferior aspect of C1 posterior arch and C2 lamina and pars. Iliac crest graft was used to bridge the decorticated C1-C2 gap to achieve fusion. The patient was extubated and discharged in 4 days. The patient was allowed full mobilization and all activities of daily living in a hard cervical collar for 12 weeks following which the collar was gradually weaned off. At 6-month follow-up patient showed full neurological recovery in left upper limb (5/5 in all myotomes bilaterally) with early bone formation between C1 and C2 posteriorly.
Discussion
Purely traumatic atlantoaxial dislocation is an extremely rare injury. Atlanto-axial joint is peculiar and different than subaxial cervical spine in being horizontal in orientation. Thus, anterior translation of atlas over axis is prevented only by ligamentous restraints. Primary stabilizer is the transverse ligament while secondary stabilizers are the apical and alar ligaments. Hyperflexion at this level may either lead to rupture of transverse ligament or Type II odontoid fracture like in this case leading to the loss of restraint and anterior translation of atlas over axis. Atlanto-axial dislocation can occur at any age and signifies high high-velocity trauma. The clinical presentation is highly varied and may range from neck pain (50%), limb weakness (70%), and pyramidal signs(90%) [4, 5]. It can also present with serious complications like such as respiratory depression, vertebral artery dissection, and quadriplegia [6, 7]. Other differentials with similar presentations include torticollis, atlanto-axial rotatory subluxation, and anteriorly displaced odontoid fractures [8]. Our patient presented with late onset of neurological symptoms and subsequently late presentation to the hospital. An associated complication with late late-presenting cases is irreducibility of atlantoaxial joint due to peri-facetal fibrosis. Salunkhe et al. have described gradual progression of atlantoaxial subluxation to irreducible dislocation leading to worsening of symptoms of pain and myelopathy [9].
Various methods to reduce a dislocated atlanto-axial joint includecervical halter traction with increasing weight [10], anterior odontoidectomy followed by posterior fusion [11], transoral anterior release and atlantoaxial reduction plate [12], and posterior only fixation with facet joint manipulation and facet joint remodelling alone or in combination with each other [13, 14]. Kirankumar et al. reported a series of nineteen patients with remote isolated Type 2 odontoid fracture with atlantoaxial dislocation. All patients with irreducible atlantoaxial joints were managed with transoral odontoidectomy followed by posterior fusion [11]. At present, irreducible atlantoaxial joints are managed with direct posterior reduction and fusion by facet manipulation and remodelling. Joint manipulation involves distraction of C1-C2 joints while remodelling involves drilling or osteotomizing parts of C1 or C2 facets, thus facilitating reduction [9, 13]. Salunke et al. in their article reported 6 cases of irreducible atlantoaxial joints. They tried to delineate factors which predict feasibility of direct posterior reduction of atlantoaxial joint which include movement on dynamic X-rays, a malunion ruled out on computed tomography CT scan, and locked facets [9]. Another article reported a series of 14 patients with 12 patients having rotatory dislocation and 2 patients having translation. All were managed using direct posterior reduction and fusion after drilling and removal of articular cartilage [14]. A number of new instruments like such as T type and L type reducers have been used by various authors to facilitate joint reduction in cases of subluxed atlanto-axial joints, but these instruments are less beneficial in long-standing complete dislocations [15]. We attempted closed reduction with gradually increasing weights on cervical traction but were unable to attain joint reduction. This was because old injury and the locked facet anatomy, also because of the fact that cervical traction forces work best in reduction of subaxial cervical spine. We managed to reduce the facets by burring out the anterosuperior part of superior facets of axis. This manoeuvre facilitates joint reduction by increasing the space for insinuation of osteotome and subsequently unlocking and reduction of the facets by controlled extension of neck. The results were satisfactory with respect to radiological joint reduction and neurological recovery.
Conclusion
Long-standing complete C1-C2 dislocations pose a challenge for a surgeon because of the associated difficulty in joint reduction. Joint remodeling and manipulation have antiquated transoral odontoidectomy as excellent results have been achieved by direct posterior approach.
Clinical Message
Traumatic atlantoaxial dislocations are extremely rare injuries. A high index of suspicion is warranted to make an early diagnosis and prompt management to obtain optimum clinical results. Irreducible atlantoaxial dislocations should be subjected to surgical reduction and fixation.
References
1. Goel A, Muzumdar D, Dange N. One stage reduction and fixation for atlantoaxial spondyloptosis: Report of four cases. Br J Neurosurg 2006;20:209-13.
2. Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am 1977;59:37-44.
3. de Roeck BN. A case of rotary dislocation of atlas on axis. Radiography 1977;43:127-30.
4. Passias PG, Wang S, Kozanek M, Wang S, Wang C. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech 2013;26:15-21.
5. Yin YH, Qiao GY, Yu XG, Tong HY, Zhang YZ. Posterior realignment of irreducible atlantoaxial dislocation with C1-C2 screw and rod system: A technique of direct reduction and fixation. Spine J 2013;13:1864-71.
6. Wadia NH. Myelopathy complicating congenital atlanto-axial dislocation. (A study of 28 cases). Brain 1967;90:449-72.
7. Panda S, Ravishankar S, Nagaraja D. Bilateral vertebral artery dissection caused by atlantoaxial dislocation. J Assoc Physicians India 2010;58:187-9.
8. Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Globl Spine J 2014;4:197-210.
9. Salunke P, Sahoo SK, Savardekar A, Ghuman M, Khandelwal NK. Factors influencing feasibility of direct posterior reduction in irreducible traumatic atlantoaxial dislocation secondary to isolated odontoid fracture. Br J Neurosurg 2015;29:513-9.
10. Chechik O, Wientroub S, Danino B, Lebel DE, Ovadia D. Successful conservative treatment for neglected rotatory atlantoaxial dislocation. J Pediatr Orthop 2013;33:389-92.
11. Kirankumar MV, Behari S, Salunke P, Banerji D, Chhabra DK, Jain VK. Surgical management of remote, isolated type II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery 2005;56:1004-12; discussion 1004-12.
12. Yin Q, Ai F, Zhang K, Chang Y, Xia H, Wu Z, et al. Irreducible anterior atlantoaxial dislocation: One-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine 2005;30:E375-81.
13. Goel A, Kulkarni AG, Sharma P. Reduction of fixed atlantoaxial dislocation in 24 cases: Technical note. J Neurosurg Spine 2005;2:505-9.
14. Goel A, Shah A. Atlantoaxial facet locking: Treatment by facet manipulation and fixation. Experience in 14 cases. J Neurosurg Spine 2011;14:3-9.
15. Suh BG, Padua MR, Riew KD, Kim HJ, Chang BS, Lee CK, et al. A new technique for reduction of atlantoaxial subluxation using a simple tool during posterior segmental screw fixation: Clinical article. J Neurosurg Spine 2013;19:160-66.
 |
 |
 |
 |
| Dr. Kaustubh Ahuja | Dr. Pankaj Kandwal | Dr. Sanny Singh | Dr. Rohit Jain |
| How to Cite This Article: Ahuja K, Kandwal P, Singh S, Jain R. Neglected Posttraumatic Atlantoaxial Spondyloptosis with Type 2 Odontoid Fracture: A Case Report. Journal of Orthopaedic Case Reports 2019 Jul-Aug; 9(4): 80-83. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com