[box type=”bio”] Learning Point of the Article: [/box]
Patients presenting with bilateral tendon ruptures should be investigated for hyperlipidaemia and treated accordingly.
Case Report | Volume 9 | Issue 4 | JOCR July-August 2019 | Page 88-91 | Sam K Yasen, Aaron J Foster, Raj R Thakrar. DOI: 10.13107/jocr.2019.v09i04.1494
Authors: Sam K Yasen[1], Aaron J Foster[1], Raj R Thakrar[1]
[1]Department of Trauma and Orthopaedics, Basingstoke and North Hampshire Hospital, Aldermaston Road, Basingstoke, RG24 9NA, Hampshire.
Address of Correspondence:
Dr. Sam K Yasen,
Department of Trauma and Orthopaedics, Basingstoke and North Hampshire Hospital, Aldermaston Road, Basingstoke, RG24 9NA, Hampshire.
E-mail: samyasen@doctors.org.uk
Abstract
Introduction: Rupture of the extensor mechanism is a relatively common injury, most frequently occurring as a result of patella fracture, while ruptures of the quadriceps tendon and patellar ligament are less common. Extensor mechanisms of healthy knees are able to tolerate large forces before rupturing; therefore, complete ruptures without significant trauma are due to minor injury to an already degenerate or attenuated tendon. Hyperlipidemia has been linked as a cause of tendon degeneration due to the systemic biological effect that it has on tenocytes. Non-identical bilateral ruptures are rare. To the best of our knowledge, this is the only case report of bilateral ruptures involving the quadriceps tendon of one knee and patellar ligament of the contralateral knee simultaneously.
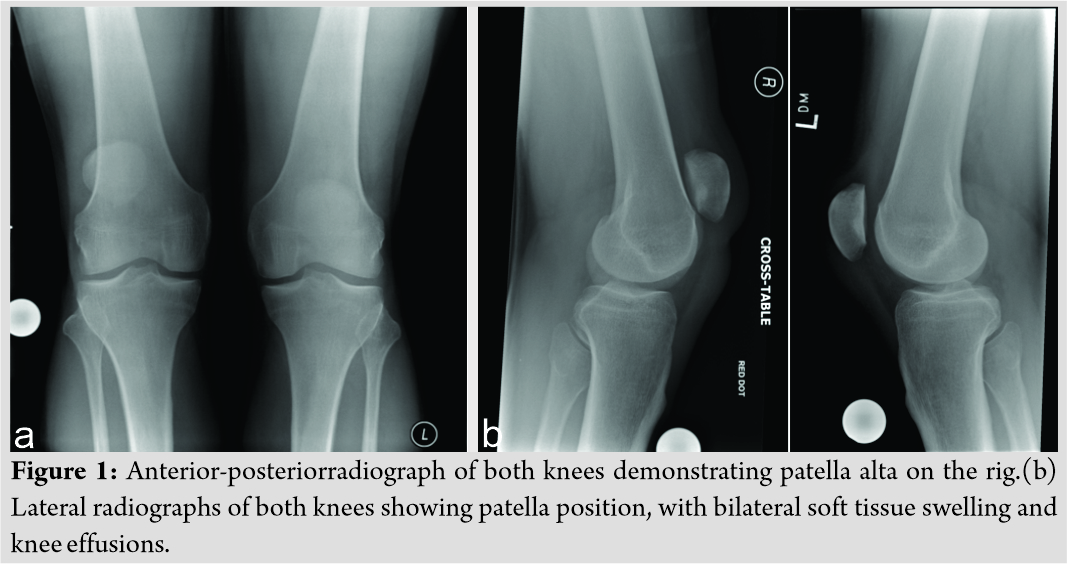
Case Report: A 42-year-old man presented to our department with bilateral traumatic rupture of the extensor mechanism of the knee. He had no medical history, was not taking any regular medications, and had no significant family history but a 15-year history of anterior knee pain. Both of his legs gave way on landing from a jump. Radiographs demonstrated a knee effusion with normal patella height on the left and a knee effusion with an elevated patella on the right. A diagnosis of quadriceps tendon rupture on the left and patellar ligament rupture on the right was made.
Conclusion: Hyperlipidemia has been associated with ruptures of the Achilles tendon but has not been reported in association with failure of the extensor mechanism of the knee. We suggest that all patients presenting with bilateral tendon ruptures, especially in the absence of systemic disease or corticosteroid therapy, are investigated for hyperlipidemia and treated accordingly.
Keywords: hyperlipidemia, hypertriglyceridemia, quadriceps tendon, patella ligament rupture
Introduction
The extensor mechanism of the knee is comprised of the quadriceps muscle and tendon, the patella and patellar ligament, and the tibial tubercle. Rupture of the extensor mechanism is a relatively common injury, most frequently occurring as a result of patella fracture. Quadriceps tendon and patellar ligament ruptures are seen less frequently [1]. The usual mechanism is one of the eccentric contractions of the quadriceps with the foot planted and the knee flexed as a person falls. Considerable force is required to rupture the extensor mechanism in the healthy knee, with estimates as high as 17.5 times body weight being required [2]. Quadriceps tendon and patellar ligament rupture are, therefore, either the result of highly significant trauma or a minor traumatic insult to an already degenerate or attenuated tendon. In the absence of significant trauma, histologically ruptured tendons typically demonstrate appearances consistent with chronic inflammation and degeneration. Hyperlipidemia is a group of disorders characterized by an increased level of lipids in the bloodstream and can involve an imbalance between low-density and high-density lipoprotein (HDL) cholesterol[3]. It is thought that this can cause a systemic biological effect on the tenocytes, thus weakening the tendon [4]. Specifically, increased blood cholesterol levels have been linked with a greater risk of tendon tears [5, 6, 7] though rupture of the extensor mechanism of the knee, in association with hyperlipidemia, as an independent variable has not been previously described. Rose and Frassica [8] previously reviewed bilateral patellar ligament ruptures and identified 48 cases in the English literature. Most patients had a prior history of systemic disease or knee surgery. There were 16 cases of atraumatic rupture, with 10occurring at the osseotendinous junction (nine at the inferior pole of the patella) and five in the mid-substance of the tendon. Case reports of non-identical ruptures are far rarer, however. To the best of our knowledge, this is the only case report of bilateral ruptures involving the quadriceps tendon of one knee and patellar ligament of the contralateral knee simultaneously.
Case Report
A 42-year-old man presented to our department with bilateral traumatic rupture of the extensor mechanism of the knee. He worked as a sports course designer, was a non-smoker, and drank alcohol only in moderation. He had no medical history, was not taking any regular medications, and had no significant family history. The incident occurred while under the influence of alcohol he jumped over a sleeping policeman as he was running along a road. Both of his legs gave way on landing and he was subsequently unable to weight bear or actively extend either knee. On direct questioning, he recounted a 15-year history of anterior knee pain, which was worse on kneeling and typically flared after approximately 2 min of running or jogging. He had, therefore, not participated in any regular sporting activity for several years.
On examination, he had a palpable defect in his extensor mechanism proximal to the patella on the left and distal to the patella on the right. He was unable to straight leg raise bilaterally and had no power in knee extension. His plain radiographs (Fig. 1) demonstrated a knee effusion with normal patella height on the left and a knee effusion with an elevated patella on the right. A diagnosis of quadriceps tendon rupture on the left and patellar ligament rupture on the right was made.
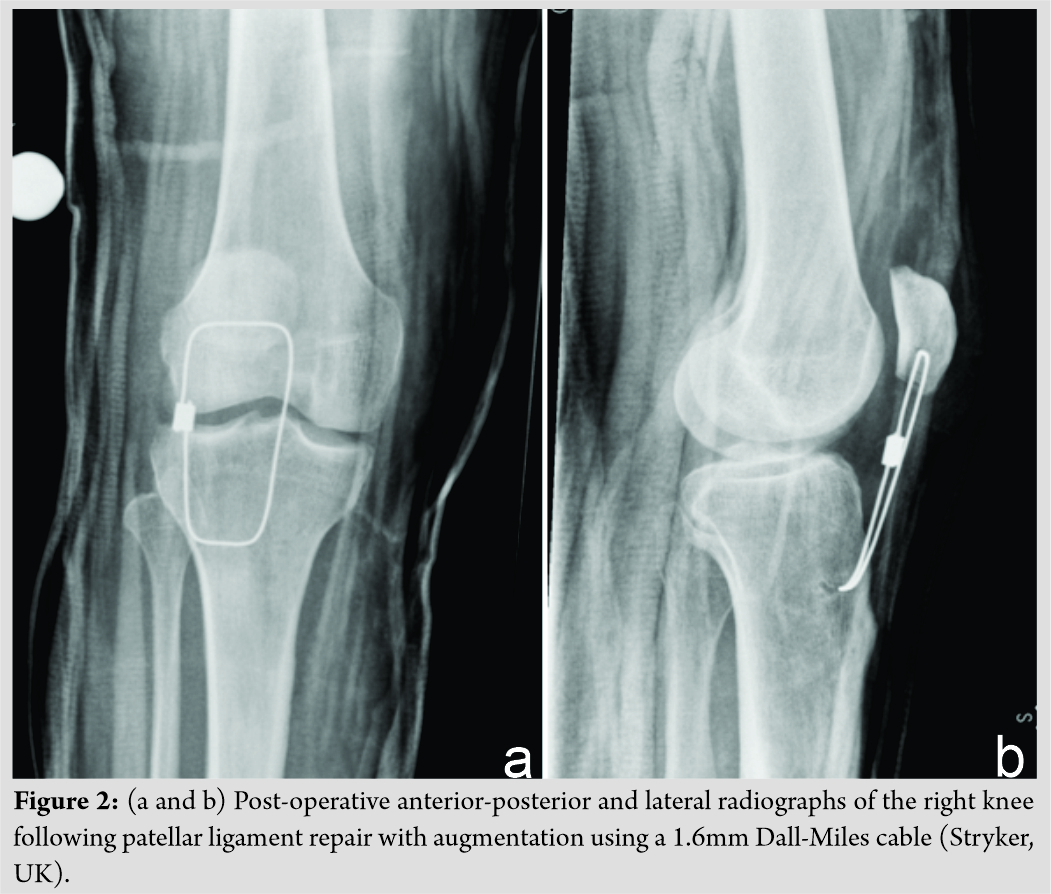
The patient was managed operatively with bilateral extensor mechanism repairs using an intraosseous suture technique. Vertically orientated tunnels using a 2.0 millimeters (mm) drill were made through the patella, and number-5 FiberWire® sutures (Arthrex Inc., Naples, FL) were used to reattach the quadriceps tendon on the left and the patellar ligament on the right. The patellar ligament repair was augmented with a 1.6mm Dall-Miles cable (Stryker, UK) passed transversely through the patella and proximal tibia. The post-operative radiographs of the right knee are shown in [Fig. 2]. At operation, the quadriceps tendon on the left had ruptured leaving approximately a 1 cm stump on the patella with near complete disruption of the retinaculum. On the right, the patellar ligament had failed at the osseotendinous junction at the inferior pole of the patella, with complete disruption of the retinaculum. Bilaterally, the extensor apparatus appeared attenuated throughout, lacking the typical healthy sheen that may be expected in a 42-year-old individual with no prior medical history. Hematological and biochemical parameters revealed a normal full blood count and differential and normal urea, creatinine, and electrolytes. His fasted lipid profile showed a serum cholesterol level of 4.9mmol/L with elevated cholesterol-HDL ratio of 5.5. Serum triglyceride levels were also raised at 2.33mmol/L.Operative biopsy of the extensor mechanism was sent for histological examination. This demonstrated tendinosis. Postoperatively, he was allowed to weight bear immediately using crutches with both knees locked in extension braces and commenced a graded rehabilitation programme. Full passive range of motion, ranging from 0 to 135°, was achieved at the 1 year post-operative time point, with no extensor lag. The patient was counseled on dietary modification with a view to starting pharmacological treatment for his hyperlipidemia should his biochemical lipid parameters not improve. To date, there have been no post-operative complications.
Discussion
Bilateral ruptures are rare, although the true incidence is unknown. They have been described as occurring in three broad groups of patients; first, in patients after local injection of corticosteroid or prolonged oral steroid therapy, this is thought to cause a breakdown of collagen organization and strength, weakening the tendon [9]; second, in patients with systemic inflammatory or autoimmune disease, such as systemic lupus erythematosus, rheumatoid arthritis, diabetes mellitus, chronic renal failure, and hyperparathyroidism, histology may show amyloid deposition in these cases [8,10]; and third, low energy and spontaneous bilateral ruptures have been reported in patients with no apparent medical comorbidity. This has been attributed to chronic, repetitive microtrauma, as described by Davidson’s theory in theliterature [11]. Taylor et al. [10] reported on a 36-year-old healthy man with bilateral patellar ligament rupture with an intrasubstance failure on one side and contralateral avulsion at the inferior patella pole. The mechanism of injury was similar to that presented in this case with the patient landing from a jump while playing football and subsequently unable to weight bear. They identified only two other case reports of non-identical ruptures [12]. There is a known association between hyperlipidemia and rupture of the tendoachilles [7]. In one series of patients undergoing surgical repair, 83% had elevated serum cholesterol levels [5]. Bilateral spontaneous rupture is rare, and most cases have been reported in relation to corticosteroid therapy [13]. Rao et al. [6], however, presented a case of bilateral rupture in a patient with recently diagnosed hypothyroidism and markedly elevated serum cholesterol levels. They surmise that the combination of lipomatous infiltration of the tendon causing fibrillation of collagen and the production of cleavage planes, coupled with decreased vascularity in part due to hypothyroidism, and led to reduced tendon strength and failure. Histopathologically, the tendon showed degenerative changes. Radiographic changes in relation to hyperlipidemia have also been described in the Achilles tendon on both ultrasonography [14] and magnetic resonance imaging [15]. In our case, the patient had a long history of anterior knee pain, which was worse on kneeling and any attempted running, and he had, therefore, not participated in sports for many years but had not previously sought medical attention. His employment involved a reasonable amount of walking and occasional kneeling, but no heavy work. In the absence of any significant perpetuating trauma, we speculate whether he had bilateral tendinopathy of his extensor mechanism as a consequence of hyperlipidemia. Macroscopically, his extensor mechanism was degenerate bilaterally at the time of operative intervention. The case is also unusual in the non-identical pattern of rupture, suggesting that the entire extensor mechanism was diseased and vulnerable to injury. We suggest that all patients presenting with bilateral tendon ruptures, especially in the absence of systemic disease or corticosteroid therapy, are investigated for hyperlipidemia and treated accordingly.
Conclusion
A 42-year-old, previously healthy, man presented with bilateral non-identical ruptures of the extensor mechanism of the knee. He was diagnosed with quadriceps tendon rupture on the left and patellar ligament rupture on the right, which, to the best of our knowledge, is the first such case report. Laboratory work-up revealed an elevated cholesterol-HDL ratio and serum triglyceride level. Hyperlipidemia has been associated with ruptures of the Achilles tendon but has not been reported in association with failure of the extensor mechanism of the knee. We, therefore, recommend that patients presenting with bilateral tendon ruptures are investigated for hyperlipidemia and treated accordingly.
Clinical Message
Patients presenting with bilateral tendon ruptures should be investigated for hyperlipidaemia and treated accordingly.
References
1. Ramseier LE, Werner CM, Heinzelmann M. Quadriceps and patellar tendon rupture. Injury2006;37:516-9.
2. Zernicke RF, Garhammer J, Jobe FW. Human patellar-tendon rupture. J Bone Joint Surg Am 1977;59:179-83.
3. Karr S. Epidemiology and management of hyperlipidemia. Am J Manage Care 2017;23:S139-48.
4. Scott A, Zwerver J, Grewal N, de Sa A, Alktebi T, Granville DJ, et al. Lipids, adiposity and tendinopathy: Is there a mechanistic link? Critical review. Br J Sport Med 2014;49:984-8.
5. Mathiak G, Wening JV, Mathiak M, Neville LF, Jungbluth K. Serum cholesterol is elevated in patients with Achilles tendon ruptures. Arch Orthop Trauma Surg 1999;119:280-4.
6. Rao SK, Navadgi BC, Vasdev A. Bilateral spontaneous rupture of Achilles tendons: A case report. J Orthop Surg (Hong Kong) 2005;13:178-80.
7. Raunest J, Bürrig KF, Derra E. Pathogenesis of Achilles tendon rupture. Chirurg1990;61:815-9.
8. Rose PS, Frassica FJ. Atraumatic bilateral patellar tendon rupture, A case report and review of the literature. J Bone Joint Surg Am 2001;83:1382-6.
9. Ismail AM, Balakrishnan R, Rajakumar MK, Lumpur K. Rupture of patellar ligament after steroid infiltration. Report of a case. J Bone Joint Surg Br 1969;51:503-5.
10. Taylor BC, Tancev A, Fowler T. Bilateral patellar tendon rupture at different sites without predisposing systemic disease or steroid use. Iowa Orthop J 2009;29:100-4.
11. Splain SH, Ferenz C. Bilateral simultaneous infrapatellar tendon rupture: Support for davidsson’s theory. Orthop Rev 1988;17:802-5.
12. Peters KM, Bucheler D, Westerdorf G. Bilateraleruptur des lig. patellae bei diabetes mellitus. Unfallchirurg2000;103:164-7.
13. Habusta SF. Bilateral simultaneous rupture of the Achilles tendon. A rare traumatic injury. Clin OrthopRelat Res 1995;(320):231-4.
14. Kainberger F, Seidl G, Traindl O, Trattnig S, Breitenseher M, Schneider B, et al. Ultrasonography of the Achilles tendon in hypercholesterolemia. Acta Radiol1993;34:408-12.
15. Dussault RG, Kaplan PA, Roederer G. MR imaging of Achilles tendon in patients with familial hyperlipidemia: Comparison with plain films, physical examination, and patients with traumatic tendon lesions. AJR Am J Roentgenol1995;164:403-7.
 |
 |
 |
| Dr. Sam K Yasen | Dr. Aaron J Foster | Dr. Raj R Thakrar |
| How to Cite This Article: Yasen S K, Foster A J, Thakrar R R. Non-identical Bilateral Rupture of the Extensor Mechanism of the Knee in a Patient with Hyperlipidemia: A Case Study. Journal of Orthopaedic Case Reports 2019 Jul-Aug; 9(4): 88-91. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com