[box type=”bio”] Learning Point of the Article: [/box]
The multi-use applications of the Reamer Irrigator Aspirator (RIA) should be considered when addressing certain oncologic, traumatic, and infectious processes in light of its potential improved efficacy and reduced complication profile compared to conventional reamers.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 47-50 | Ryan T Voskuil, Brian Viscomi, Ginger E Holt, Jeremy Bruce. DOI: 10.13107/jocr.2019.v09.i05.1528
Authors: Ryan T Voskuil[1], Brian Viscomi[2], Ginger E Holt[3], Jeremy Bruce[1]
[1]Department of Orthopaedic Surgery, University of Tennessee College of Medicine, Tennessee 975 E. Third Street, Hospital Box 260,Chattanooga, TN 37403, United States,
[2]Department of Orthopaedic Surgery, East Tennessee State University Quillen School of Medicine, 1276 Gilbreath Dr, Johnson City, TN 37614, United States,
[3]Department of Orthopaedic Surgery, Vanderbilt University Medical Center, Nashville, Tennessee, 1211 Medical Center Drive, Nashville, TN 37232, United States.
Address of Correspondence:
Dr. Ryan T Voskuil,
Department of Orthopaedic Surgery, University of Tennessee College of Medicine, Chattanooga, Tennessee 975 E. Third Street, Hospital Box 260, Chattanooga, TN 37403, United States.
E-mail: rtvoskuil@gmail.com
Abstract
Introduction: Introduction: The treatment of chronic intramedullary infection of the long bones relies on microbe-specific antibiotics in conjunction with surgical removal of infected necrotic material. We discuss the use of reamer–irrigator–aspirator(RIA) for debridement of the intramedullary canal instead of conventional reaming techniques. This is the first case report to explore the use of RIA for osteomyelitis.
Case Report: We discuss the use of the RIA in treatment of a 26-year-old female presenting with chronic osteomyelitis of the left distal femoral shaft. She had normalization of infection laboratories at 6 weeks and complete resolution of symptoms at 3 months and was released at 6 months.
Conclusion: Recent exploration of the RIA system’s (Synthes®, Inc. West Chester, Philadelphia) multipurpose applications has indicated use in long bone debridement. While further exploration and high-quality studies are needed to make robust claims of efficacy, we believe that the use of RIA in the context of chronic osteomyelitis is a superior alternative to conventional reaming techniques.
Keywords: Reamer–irrigator–aspirator, chronic osteomyelitis, reamer, intramedullary infection, reamer, irrigation, aspiration.
Introduction
The current gold standard for debridement of infection in the intramedullary canal is conventional reaming of the cavity for removal of infected material [1]. Indeed, Sancineto and Barla report admirable results in treatment of 18 patients presenting with femoral and/or tibial osteomyelitis using traditional reaming techniques and concurrent antibiotic cement spacer: there was no report of subsequent infection during the follow-up interval (10–54 months) [2]. However, conventional reaming techniques in surgical debridement of chronic osteomyelitis present unique risk factors: increased intramedullary temperature resulting in thermal necrosis, inadequate removal of infected medullary cavity contents, and iatrogenic local and hematogenous spread of infection [3]. Further, increased intramedullary pressure can lead to extravasation of medullary contents into the venous pool resulting in impaired pulmonary gas exchange [4]. We believe that the use of a single-pass reamer–irrigator–aspirator (RIA) system more effectively accomplishes the goals of debridement while the constant irrigation and suction components of the system effectively limit the potential risks described. We are not aware of any other case report documenting the use of RIA in treatment of idiopathic chronic osteomyelitis.
Case Report
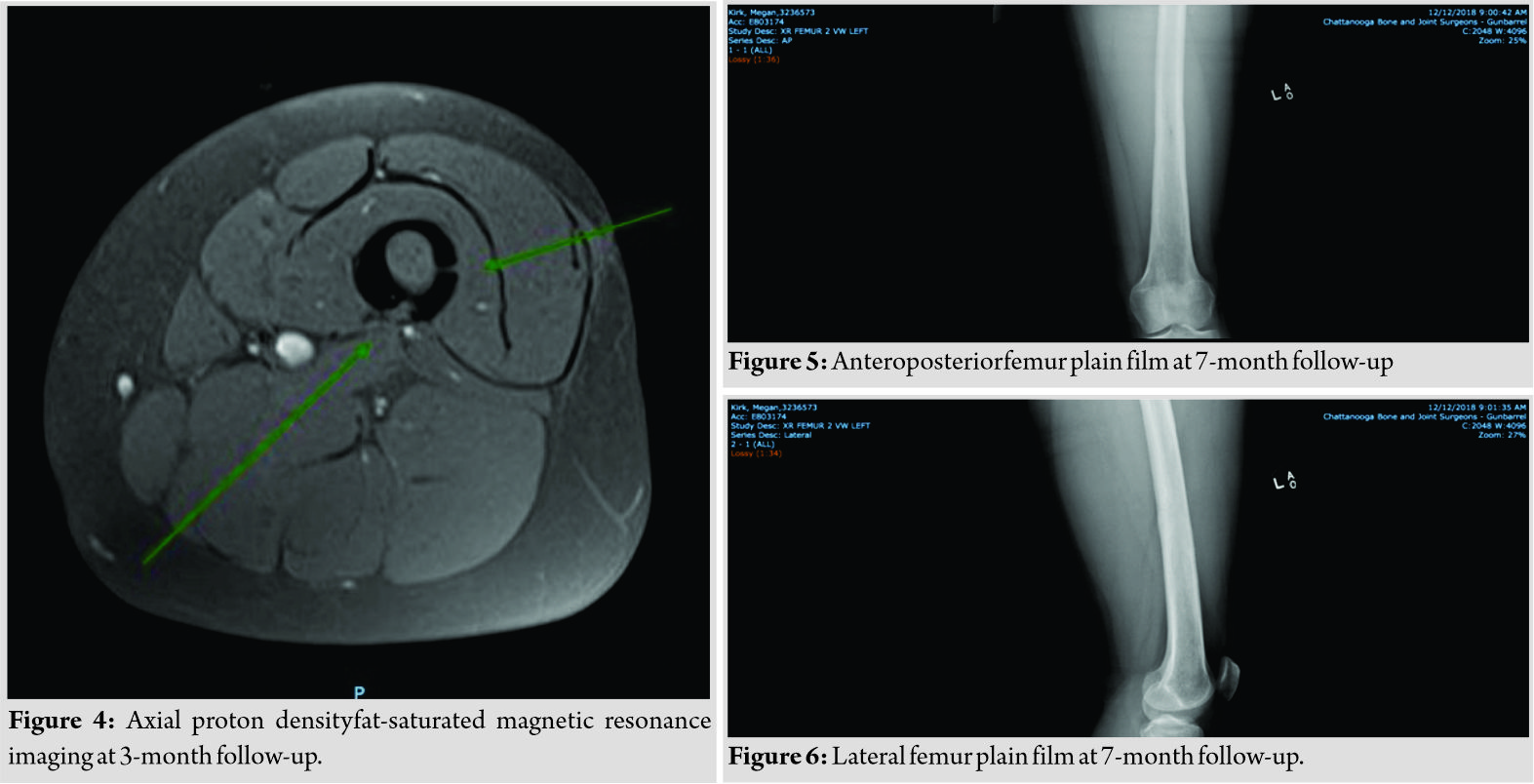
A 26-year-old female presented to office with an insidious onset of pain in her left distal femur that had been present for several months. The patient reports no history of trauma. Physical examination reveals that the patient was a febrile. There was no evidence of a rash or wound and weakness or numbness, but the patient did note swelling of the involved extremity. Normal pulse times were noted in all four extremities. Pushing/pulling provoked pain. Of note, the patient reported a recent molar extraction as her only past surgical history. The pain persisted and increased in severity over the course of several months before amagnetic resonance imaging (MRI) was obtained. MRI interpretation revealed a large marrow-replacing lesion in the distal femoral shaft with a posterior cortical breach and associated posteromedial soft tissue component (Fig. 1 and 2). 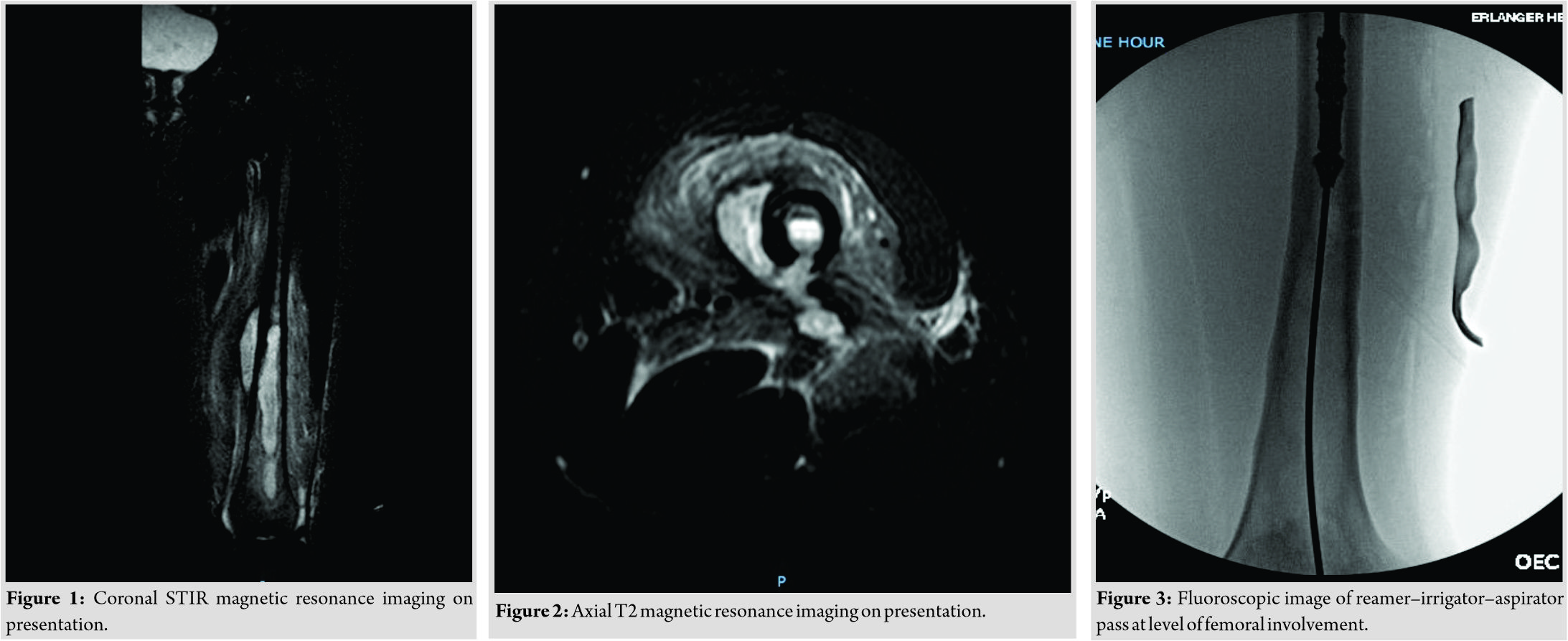
A thorough review of the MRI revealed that the main foci of infection of her distal femur and posteromedial fluid collection were roughly 12 cm proximal to the superior pole of the patella. On measuring 12 cm from the superior pole of the patella to the lateral thigh, a 6-cm longitudinal incision was made. Bovie electrocautery was used throughout the procedure to coagulate superficial vasculature. A longitudinal incision was made in the iliotibial band in line with that of the skin. The anterolateral compartment of musculature was identified, and Bovie was used to gently lift the compartment off the lateral intermuscular septum, revealing the femoral shaft. The periosteum of the femoral shaft was longitudinally incised, and a Cobb was used to circumferentially elevate the periosteum. Using blunt dissection, the posteromedial periosteum was separated resulting in a rush of fluid. Following decompression, samples were sent for biopsy and culture. After thorough decompression, a 3.5-mm drill was used to drill the lateral cortex. The lateral wound was irrigated and temporarily covered with a wet lap. We then addressed the RIA component of the procedure. X-ray was used to identify a start point roughly 8 cm proximal to the tip of the greater trochanter where a 4-cm incision was made in line with the femoral shaft. The guidewire was used to identify the tip of the greater trochanter on an anteroposterior view and to confirm alignment with the femoral shaft on the lateral view. The guidewire was advanced to the level of the lesser trochanter, and a 12-mm reamer was used to open the proximal femur. Based on measurements of the femoral isthmus, a 12-mm head was selected for the RIA system. On assembly of the RIA, a ball-tipped guidewire was passed into the femur and seated into the physeal scar of the distal femur. The RIA was then introduced over the ball-tipped guidewire and advanced distally with the cutting head moving in a forward direction. The RIA was slowly advanced through the medullary cavity with periodic retraction to allow proper suction of infected graft particulate. Progress was slowed upon reaching the level of the infection due to severe sclerosis of the distal isthmus (Fig. 3). One pass of the medullary cavity was made without complications or mechanic malfunction. The infected bone graft collected was stored in two containers. On obtaining cultures, anesthesia administered intravenous vancomycin. The proximal femoral wound was thoroughly irrigated and closed. Vancomycin powder was used locally over the lateral thigh incision. The patient remained in the hospital for 4days following surgery. She received empiric antibiotics and was discharged home when the surgical cultures and sensitivities resulted with final infectious disease antibiotic recommendations made.The patient was made 50-pound partial weight bearing on her left leg as precaution for 6 weeks. At 2 weeks following surgery, the patient had a decrease in pain and no signs of recurrent infection were noted. The patient was followed by infectious disease in the hospital and after surgery as well and completed 30 days of linezolid followed by Bactrim to finish the 6-week course. At 3month follow-up, the patient continued to show improvement clinically with complete resolution of the thigh pain she described preoperatively. Her white blood cell count, sedimentation rate, and c-reactive protein all returned to normal levels 6 weeks after surgery. An MRI was also obtained and revealed reactive changes evident of canal reaming but no osteomyelitis or abscesses (Fig. 4). At the 7-month follow-up, she continued to have resolution of all symptoms with normal laboratories and X-rays and was released from orthopedic and infectious disease follow-up (Fig. 5 and 6). The patient was made aware that her case would be written for publication, and informed consent was completed after she agreed.
Discussion
The treatment of chronic long bone osteomyelitis is complex. Most cases of chronic osteomyelitis result from previous open fracture. This was not the case for our patient; however, the principles of treatment remain the same. The alternative to our use of RIA would have been the use of a traditional reamer. We believe that RIA offers a better surgical approach for several reasons. First, compared to standard reamers, RIA utilizes a disposable head that is always sharp [5]. As Dehghan and Schemitsch note, this allows for simultaneous opening of the canal, removal of sclerotic and infected contents, and promotion of revascularization [5]. Second, we believe that RIA use effectively limits increased intramedullary pressure and temperature, thus limiting both necrosis and extravasation of medullary contents. A 2016 animal study performed by Miller et al. examined the number of microemboli in circulation following conventional sequentially reamed nailing and RIA reamed nailing. Their results demonstrate a statistically significant reduction in circulating microemboli in the RIA reamed group [6]. Further, a 2017 prospective randomized clinical trial in humans demonstrates a modest reduction in total embolism score in patients treated with RIA compared to those treated with a conventional reamer [7]. We note that, although fewer emboli were present in the RIA group, this did not result in measured physiologic differences. Finally, studies have documented the ability of the RIA system to successfully remove large quantities of intramedullary material [5,8].Dawson et al. directly compared the amount of intramedullary contents gathered by femoral RIA, anterior, and posterior iliac crest. The RIA system obtained the most graft at an average of 38 cm3, and it was significantly more than anterior iliac crest bone graft, solidifying the ability of RIA to remove a large amount of intramedullary contents [9]. It is apparent that simultaneous irrigation and aspiration as achieved by RIA provides a more effective mechanism for removal of intramedullary contents than traditional techniques. Therefore, we believe that RIA offers a promising alternative to conventional surgical practice and should be considered in the care of patients with chronic long bone osteomyelitis. We should note that RIA use in treatment of chronic osteomyelitis is limited to the long bones as the smallest reamer head is 12 mm. Further, RIA is a costly system and may not be realistic in many health-care settings.
Conclusion
RIA offers a promising alternative to conventional reaming techniques in a variety of situations including long bone debridement for osteomyelitis. We believe that this case report is the first of its kind to discuss the treatment of chronic osteomyelitis using RIA for intramedullary debridement. The favorable outcome in this case is encouraging and lends to the recent body of evidence surrounding the multiple uses of RIA in orthopedic surgery. In addition, this case highlights the importance of understanding the variety of options for treating difficult problems and provides support for adding RIA to the toolbox when dealing with long bone infection.
Clinical Message
The multiuse applications of the RIA should be considered when addressing certain oncologic, traumatic, and infectious processes in light of its potential improved efficacy and reduced complication profile compared to conventional reamers.
References
1. Kanakaris NK, Morell D, Gudipati S, Britten S, Giannoudis PV. Reaming irrigator aspirator system: Early experience of its multipurpose use. Injury 2011;42 Suppl 4:S28-34.
2. Sancineto CF, Barla JD. Treatment of long bone osteomyelitis with a mechanically stable intramedullar antibiotic dispenser: Nineteen consecutive cases with a minimum of 12 months follow-up. J Trauma 2008;65:1416-20.
3. Tosounidis TH, Calori GM, Giannoudis PV. The use of reamer-irrigator-aspirator in the management of long bone osteomyelitis: An update. Eur J Trauma Emerg Surg 2016;42:417-23.
4. Bellapianta J, Gerdeman A, Sharan A, Lozman J. Use of the reamer irrigator aspirator for the treatment of a 20-year recurrent osteomyelitis of a healed femur fracture. J Orthop Trauma 2007;21:343-6.
5. Dehghan N, Schemitsch EH. Extended applications of the reamer-irrigator-aspirator (RIA) system. Injury 2017;48 Suppl 1:S47-51.
6. Miller AN, Deal D, Green J, Houle T, Brown W, Thore C, et al. Use of the reamer/Irrigator/Aspirator decreases carotid and cranial embolic events in a canine model. J Bone Joint Surg Am 2016;98:658-64.
7. Hall JA, McKee MD, Vicente MR, Morison ZA, Dehghan N, Schemitsch CE, et al. Prospective randomized clinical trial investigating the effect of the reamer-irrigator-aspirator on the volume of embolic load and respiratory function during intramedullary nailing of femoral shaft fractures. J Orthop Trauma 2017;31:200-4.
8. Belthur MV, Conway JD, Jindal G, Ranade A, Herzenberg JE. Bone graft harvest using a new intramedullary system. Clin OrthopRelat Res 2008;466:2973-80.
9. Dawson J, Kiner D, Gardner W 2nd, Swafford R, Nowotarski PJ. The reamer-irrigator-aspirator as a device for harvesting bone graft compared with iliac crest bone graft: Union rates and complications. J Orthop Trauma 2014;28:584-90.
 |
 |
 |
 |
| Dr. Ryan T Voskuil | Dr. Brian Viscomi | Dr. Ginger E Holt | Dr. Jeremy Bruce |
| How to Cite This Article: Voskuil R T, Viscomi B, HoltGE, Bruce J. Reamer–Irrigator–Aspirator Multiuse Application in the Treatment of Chronic Osteomyelitis. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 47-50. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com