[box type=”bio”] Learning Point of the Article: [/box]
In osteochondroma patients presenting with acute limb ischemia secondary to thrombus who fail to reperfuse following initial thrombectomy, the coexistence of concurrent vascular complications such as pseudoaneurysm should always be considered.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 59-62 | Paul Rodham, Lauren Shelmerdine, James McCaslin, Tom Beckingsale. DOI: 10.13107/jocr.2019.v09i05.1534
Authors: Paul Rodham[1], Lauren Shelmerdine[2], James McCaslin[2], Tom Beckingsale[3]
[1]Department of Plastic Surgery, University Hospital of North Durham, Durham, England,
[2]Department of Vascular Surgery, Freeman Hospital, Newcastle Upon Tyne, England,
[3]Department of Orthopaedics, Freeman Hospital, Newcastle Upon Tyne, England.
Address of Correspondence:
Dr. Paul Rodham,
Department of Plastic Surgery, University Hospital of North Durham, Durham. DH1 5TW, England.
E-mail: plrodham@doctors.org.uk
Abstract
Introduction: Vascular complications occurring secondary to osteochondroma are a rare phenomenona. They typically present insidiously with claudication, however, uncommonly may present with acute limb ischaemia. We present a case of a young boy who presented with acute limb ischaemia secondary to osteochondroma with an intraoperative diagnosis of popliteal pseudoaneurysm.
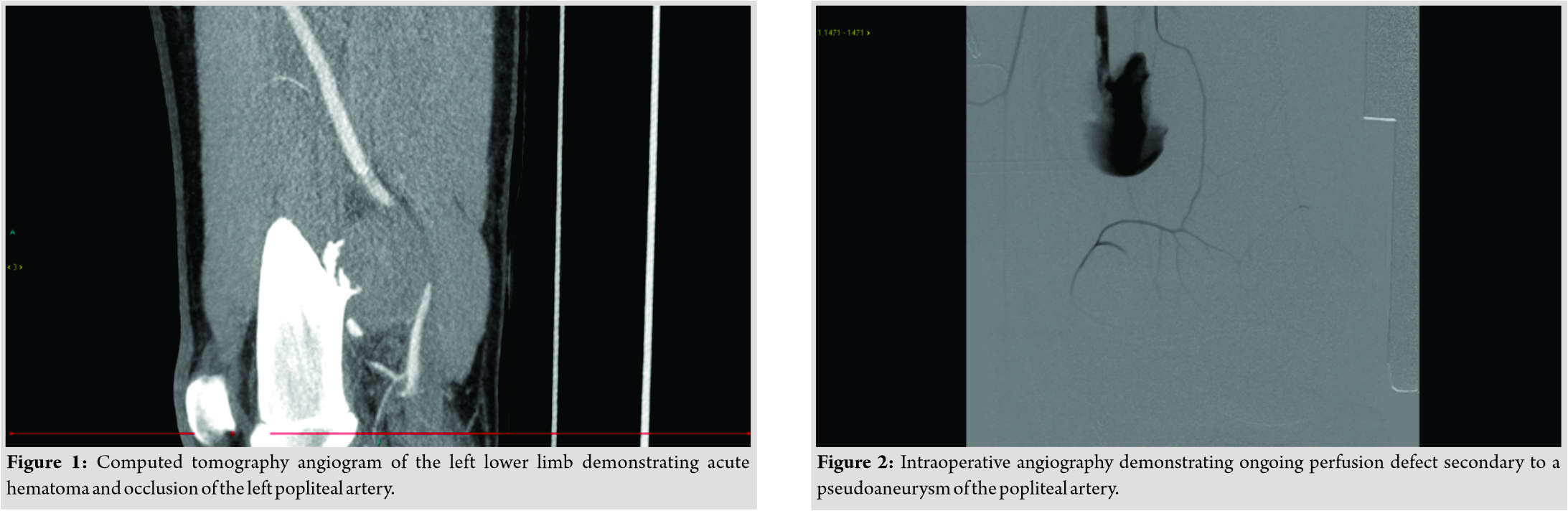
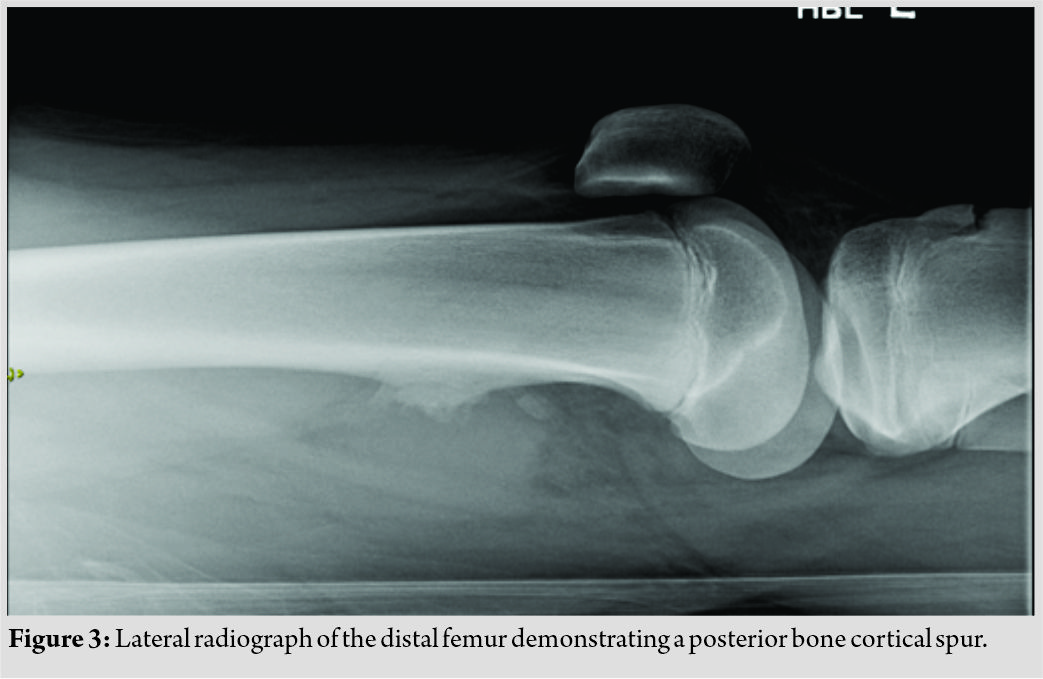
Case Report: A 15-year-old male presented with an acutely ischaemic limb. A computed tomography CT angiogram was performed which demonstrated complete occlusion of his popliteal artery secondary to a tumour of the distal femur. The patient underwent an open biopsy of the tumour followed by thrombectomy which failed to resolve the ischaemia. After further unsuccessful attempts at thrombectomy, angiography was performed which revealed a pseudoaneurysm. . The patient underwent a successful popliteal exclusion bypass using ipsilateral reversed long saphenous vein. The lesion was subsequently identified as an osteochondroma. The patient made a good recovery and at his latest follow-up is ambulant, free from claudication, and demonstrates good flow through the bypass on duplex ultrasonography.
Conclusion: Acute limb ischaemia is a rare occurrence within the adolescent population and will, therefore, frequently be secondary to an uncommon aetiology. Whilst While osteochondroma are is a common cause of vascular complications in this population, the onset of symptoms is usually more insidious. The acute onset, in this case, therefore, raised uncertainty as to the potential for malignancy. The management of these patients should involve a combination of both vascular and orthopaedic surgery in order to return perfusion whilest also ensuring the offending lesion is managed appropriately. In patients where initial measures do not restore perfusion, then the potential for further complications such as pseudoaneurysm should be considered and managed promptly.
Keywords: Osteochondroma, ischaemia, oncology, pseudoaneurysm.
Introduction
Vascular complications occurring secondary to osteochondroma are rare. Within literature, they most commonly occur due to pseudoaneurysm or direct compression by the tumor. We report a case of superficial femoral artery (SFA) thrombosis, popliteal artery occlusion, and a subsequent intraoperative diagnosis of popliteal pseudoaneurysm that was not visible on initial computed tomography (CT) angiography. This combination of complications has not been previously reported within literature; however, awareness of their potential is of utmost importance for clinicians treating young patients with acute limb ischemia who invariably have an unusual etiology.
Case Report
A 15-year-old boy was referred to our unit with severe leg pain on a background of 1 week of claudication-type symptoms. On arrival, he had a dusky left lower leg with reduced sensation, reduced movements, and a capillary refill time of 7 s. Examination of the foot demonstrated an absence of the dorsalis pedis and posterior tibial pulses. Medical history included meningococcal septicemia at 2 years old with no long-term sequelae. There was no family history of vascular disease. Blood tests revealed a normal prothrombin time of 14 s and a prolonged thrombin time of 194 s. A CT angiogram demonstrated complete occlusion of the left popliteal artery with additional thrombus within the profunda femoris artery (Fig. 1). The apparent cause for this was a mixed density lesion arising from the distal femur, compressing the femoral vessels. As thrombus was seen in the profunda without an obvious cause (the tumor was in the distal femur), a diagnosis of deep venous thrombosis (DVT) and paradoxical embolus was considered. An echocardiogram excluded a patent foramen ovale and subsequent imaging excluded a DVT. The exact cause of the post-traumatic femoral (PFA) thrombus was never ascertained, but the suspicion was the whole SFA thrombosed initially with thrombus spilling into the PFA, then later embolized distally away from the PFA origin.
Initial concern was that this lesion represented a malignant tumor with both osteosarcoma and chondrosarcoma within a previous osteochondroma considered. It was also considered that this could simply represent an osteochondroma with a vascular complication. Given the acute presentation, the patient was taken immediately to theater for attempted decompression of the tumor and popliteal vessels. Due to the concerns that this lesion may have represented a malignant tumor, an open biopsy was performed through a medial approach. Copious hematoma was evident which was compressing the popliteal vessels.
Following decompression, the wound was irrigated and closed and attention transitioned to the thrombectomy through the common femoral artery. Initial femoral thrombectomy was successful in retrieving a large volume of fresh thrombus. Despite this, an on-table angiogram demonstrated little flow distal to the tumor and so a repeat thrombectomy was performed. Further, angiography again demonstrated poor distal flow with the vessel, this time appearing to empty into a false aneurysm (Fig. 2). At this point, it was decided that further thrombectomy would be futile, so a popliteal exclusion bypass was performed using ipsilateral reversed long saphenous vein to good effect. Given the ischemic time, prophylactic four-compartment fasciotomies were performed and the patient was transferred to the pediatric intensive care unit on an unfractionated heparin infusion. Intraoperative frozen sections demonstrated a predominantly fibrinous tumor with no bony or cartilaginous matrix. This was later confirmed to be an osteochondroma. Post-operative radiographs and a magnetic resonance imaging demonstrated a posteromedial cortical spur without evidence of a clear chondral cap which was thought to have been removed intraoperatively (Fig. 3). Unfortunately, the patient returned to theater on the first post-operative night due to hemorrhage from a slipped ligature on the graft managed with a single suture. The patient was converted to warfarin on post-operative day 11 and subsequently transitioned to clopidogrel following 3 months of anticoagulant therapy. He was discharged on post-operative day 18 having made significant progress with the physiotherapists. At his 5 month follow-up, the patient remained free from claudication and demonstrates good flow on duplex ultrasonography follow-up at 1 year.
Discussion
Osteochondromas account for 10–15% of all bone tumors and are the most common benign tumor of bone [1]. They arise predominantly in metaphyseal bone undergoing endochondral ossification as a result of the aberrant proliferation of epiphyseal tissue at the periphery of the growth plate [2]. On histology, these lesions are characterized by a hyaline cartilage cap which also undergoes ossification once growth of the lesion arrests [3]. Osteochondroma most frequently occurs within the long bones with 40% of lesions affecting the knee. They most commonly occur in isolation, with multiple lesions raising the suspicion of hereditary multiple osteochondromas [1]. Vascular complications occurring secondary to an osteochondroma are rare, but most commonly present following ossification of the cartilage cap [4]. The repeated abrasion of a relatively fixed vessel against a bony exostosis can result in a number of complications including claudication, pseudoaneurysm, phlebitis, or acute ischemia. Rarely, patients may also suffer from venous disease in the form of DVT [5, 6]. Of these complications, acute limb ischemia is the least frequently reported, occurring due to direct compression, thrombosis, or distal embolization. Acute limb ischemia secondary to thrombosis most commonly occurs at a site of compression with management most commonly comprising thrombectomy and resection of the tumor [4, 7]. In contrast, distal embolization most commonly occurs in association with pseudoaneurysm formation due to the altered hemodynamics within the vessel [8]. These lesions also frequently require embolectomy combined with either closure of the arterial defect or exclusion bypass [4]. Within the presented case, and in contrast to literature, the arterial thrombosis occurred proximal to the level of obstruction. Perioperatively, it was thought that this may be due to a DVT that had embolized paradoxically through a patent foramen ovale; however, this was excluded by pre-operative echocardiography, and DVT was excluded with an ultrasound. There was also difficulty in establishing the cause of ongoing ischemia despite the adequate excavation of thrombus, and it was not until the patient had undergone two attempts at thrombectomy that the pseudoaneurysm became apparent on angiography. In retrospect, the significant tumor mass/hematoma initially present within the popliteal fossa is likely to have been a thrombosed pseudoaneurysm around the tumor. Concern in this case that the lesion may represent a malignant tumor led to a decision to perform a medial approach to decompressing the tumor along the posterior border of vastus medialis to ensure that should it be confirmed as malignant, only one compartment would have been contaminated. Within literature, there are few reported cases of acute limb ischemia occurring due to sarcoma with all of these cases arising from vascular tissue [9]. There are no reported cases of acute limb ischemia occurring secondary to a primary bone sarcoma. Given this information, the operating team may have been able to expedite their intervention; however, this did not ultimately affect the outcome attained.
Conclusion
Acute limb ischemia is a rare occurrence within the adolescent population and will, therefore, frequently be secondary to a rare etiology. Within literature, the presentation of vascular complications secondary to osteochondroma is classically more insidious, as opposed to a presentation with acute limb ischemia as in this case. In addition, the occurrence thrombus proximal to the site of the lesion was unusual and raised suspicion that this may potentially represent a malignant lesion or an alternate coexisting pathology. The presentation of acute limb ischemia and further intraoperative diagnosis of a pseudoaneurysm distal to the thrombus were unusual and have not previously been reported within literature. It is critical that these patients are managed through a multidisciplinary team involving both vascular and orthopedic surgery to ensure that such complications are recognized and managed promptly and effectively.
Clinical Message
In osteochondroma patients presenting with acute limb ischemia secondary to thrombus who fail to reperfuse following initial thrombectomy, the coexistence of concurrent vascular complications such as pseudoaneurysm should always be considered.
References
1. Mavrogenis AF, Papagelopoulos PJ, Soucacos PN. Skeletal osteochondromas revisited. Orthopedics 2008;31:orthosupersite.com/view.asp?rID=32071.
2. Milgram JW. The origins of osteochondromas and enchondromas. A histopathologic study. Clin Orthop Relat Res 1983;174:264-84.
3. Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the clinical, radiological and pathological features. In Vivo 2008;22:633-46.
4. Vasseur MA, Fabre O. Vascular complications of osteochondromas. J Vasc Surg 2000;31:532-8.
5. Dhillon M, Kumar V, Bachhal V, Bali K. Distal femoral osteochondroma masquerading as deep vein thrombosis in an adolescent male. J Knee Surg 2013;26 Suppl 1:S11-5.
6. Navadgi BC, Davies N, Beale AM, Arya R, Williamson DM. Deep venous thrombosis in a child: An unusual presentation of an osteochondroma. J Pediatr Orthop 2009;29:312-4.
7. Andrikopoulos V, Skourtis G, Papacharalambous G, Antoniou I, Tsolias K, Panoussis P, et al. Arterial compromise caused by lower limb osteochondroma. Vasc Endovascular Surg 2003;37:185-90.
8. Woolson ST, Maloney WJ, James DR. Superficial femoral pseudoaneurysm and arterial thromboembolism caused by an osteochondroma. J Pediatr Orthop 1989;9:335-7.
9. Navadgi BC, Davies N, Beale AM, Arya R, Williamson DM. Acute ischemoa of extremity as a first manifestation of peripheral artery leiomyosarcoma: Report of a case and review of the literature. J Pediatr Orthop 2009;29:312-4.
 |
 |
 |
 |
| Dr. Paul Rodham | Dr. Lauren Shelmerdine | Dr. James McCaslin | Dr. Tom Beckingsale |
| How to Cite This Article: Rodham P, Shelmerdine L, McCaslin J, Beckingsale T. Acute Limb Ischemia and a Disguised Pseudoaneurysm: A Rare Presentation of a Femoral Osteochondroma. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 59-62. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com