[box type=”bio”] Learning Point of the Article: [/box]
Bilateral ulnar nerve instability and ECU dislocation should be addressed as possible manifestations of systemic disorders such as Marfan´s syndrome.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 3-6 | RN Brandariz, MO Abrego, JG Boretto, GL Gallucci, P De Carli. DOI: 10.13107/jocr.2019.v09i05.1506
Authors: RN Brandariz[1], MO Abrego[1], JG Boretto[1], GL Gallucci[1], P De Carli[1]
[1]Department of Trauma and Orthopaedics “Carlos E. Ottolenghi,” Italian Hospital of Buenos Aires, Buenos Aires, Argentina.
Address of Correspondence:
Dr. Mariano Oscar Abrego,
Hospital Italiano de Buenos Aires, Juan D. Perón 4190 (C1181ACH) Buenos Aires, Argentina.
E-mail: mariano.abrego@hospitalitaliano.org.ar
Abstract
Introduction: Marfan’s syndrome is a hereditary, autosomal dominant multisystemic disorder involving connective tissue. Bilateral extensor carpi ulnaris and ulnar nerve (UN) instability is rare, usually caused by the alteration of structures mainly formed by connective tissue. The association between Marfan’s syndrome and bilateral instability of UN and extensor carpi ulnaris has never been reported.
Case Report: We present the case of a 38-year-old female with no history of trauma, diagnosed with Marfan’s syndrome, who developed bilateralinstability of the UN and extensor carpi ulnaris. Bilateral UN transposition and extensor carpi ulnaris tenoplasty were performed.
Conclusion: Atraumatic bilateral instability of UN and extensor carpi ulnaris is a new rare clinical profile caused by Marfan’s syndrome whether standard treatment is successful in a long-term basis in these particular cases of collagen intrinsic pathology remains unclear.
Keywords: Marfan’s syndrome, ulnar nerve instability, extensor carpi ulnaris dislocation.
Introduction
Extensor carpi ulnaris (ECU) dislocation may be associated with instability of the distal radioulnar joint as the result of post-traumatic sequelae. It is also frequently seen in rheumatoid disease [1]. On the other hand, recurrent dislocation of the ulnar nerve (UN) at the elbow is uncommon. Hyperlaxity is usually present, with no differences in age, gender, or physical activity [2]. These two conditions can be caused by the alteration of structures that provide stability to both the ECU and the UN. These structures are known as the ECU tendon subsheath and the cubital tunnel retinaculum. They are mainly formed by connective tissue; therefore, in the presence of tissue anomalies, the chances of instability may increase. Marfan’s syndrome (MS) was first described by Antoine-Bernard Marfan [3] in 1896. It is a hereditary, autosomal dominant connective tissue multisystemic disorder [4, 5]. Classic clinical profile includes ocular, cardiovascular, and musculoskeletal abnormalities [6]. Skeletal findings include pectus excavatum, pectus carinatum, scoliosis, spondylolisthesis, calcaneal displacement, “protrusio acetabuli,” arachnodactyly, and pes planus [7]. MS diagnosis requires multidisciplinary assessment. To the best of our knowledge, there are no medical reports describing MS as the cause of bilateral UN and ECU instability.
Case Report
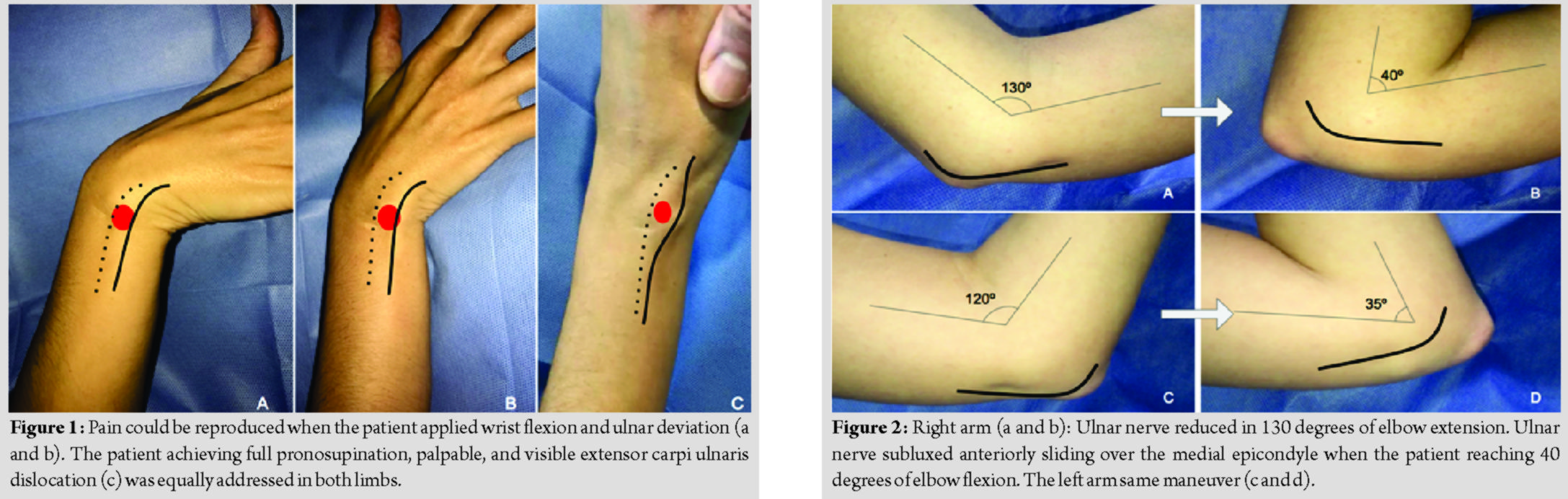
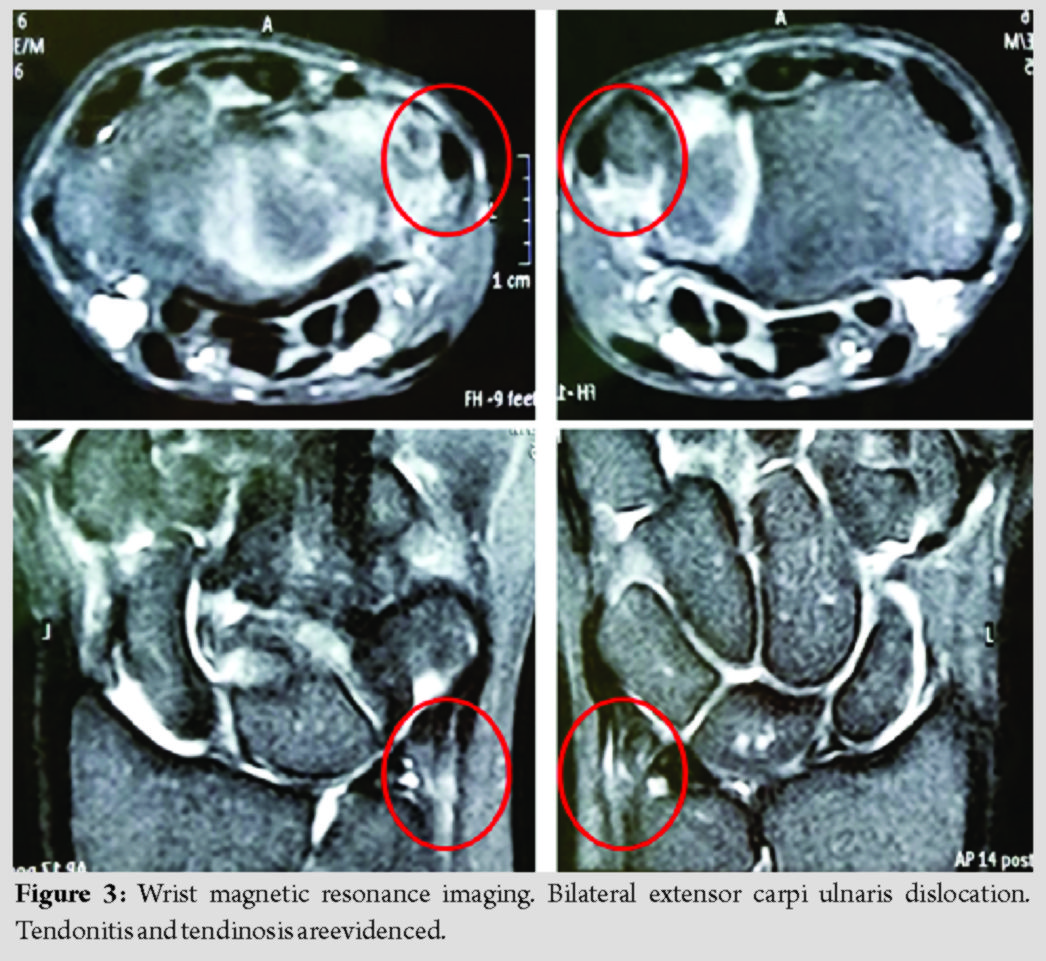
A 38-year-old right-hand dominant female patient with MS was admitted to our institution addressing bilateral elbow and wrist pain for the past 2 years. The patient had no history of upper limb trauma. Her symptoms increased during manual activities. Clinically, exquisite and snapping pain could be reproduced when the patient pronates her forearms applying wrist flexion and ulnar deviation. When achieving full pronosupination, palpable and visible ECU dislocation was equally addressed in both limbs (Fig. 1). When reaching 30 degrees of elbow flexion, UN subluxed anteriorly sliding over the medial epicondyle; this phenomenon was found to be bilateral (Fig. 2). Paresthesia along UN territory was constant. There was no motor deficit along with UN distribution.
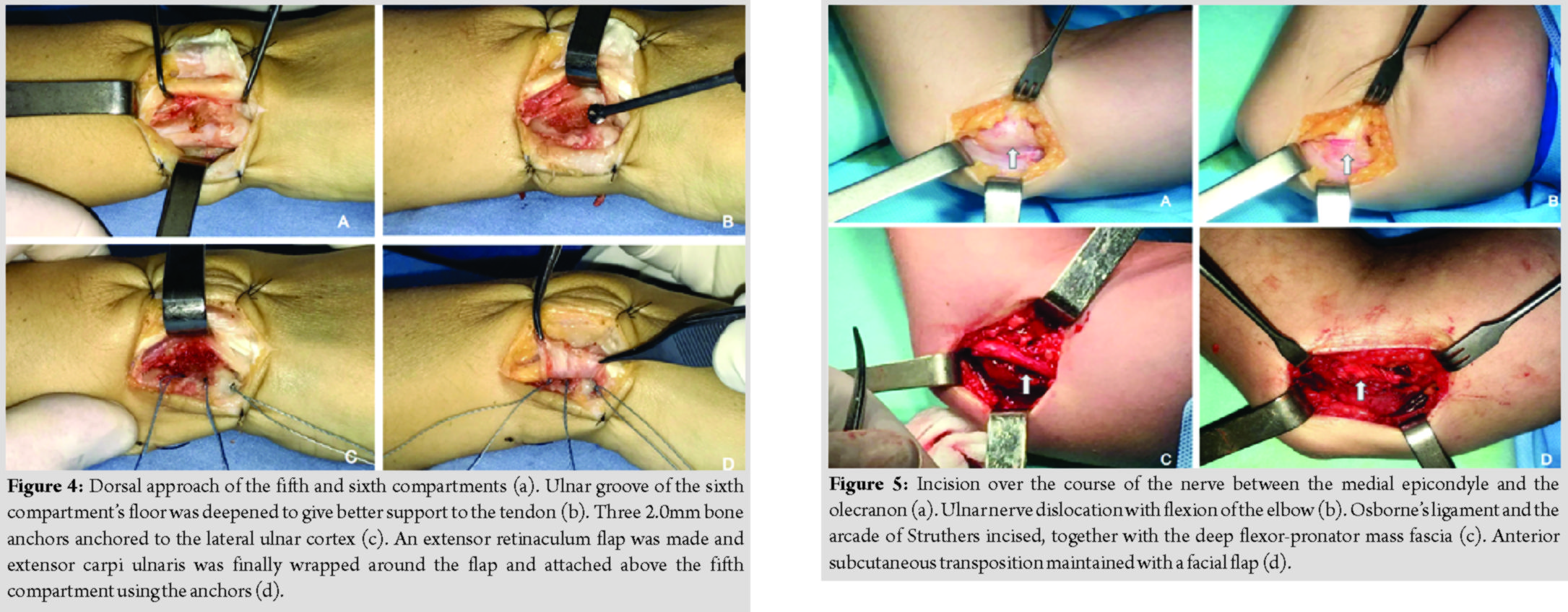
The patient’s initial assessment included visual analog scale (VAS), Quick-Disability of the Arm, Shoulder, and Hand (Q-DASH), and the modified American Shoulder and Elbow Surgeons (m-ASES)scores. VAS for wrists and elbows happened to be 7 and 5, respectively. Pre-operative Q-DASH and m-ASES scores were 33 and 45, respectively. Plain radiographs were performed with no pathological findings. A magnetic resonance imaging disclosed bilateral ECU dislocation together with tendonitis and tendinosis (Fig. 3).
Due to the insufficient mechanical containment of both ECU and UN, bilateral surgical treatment was offered. Limbs were planned to be treated separately; first, the dominant side. Surgical procedure consists of two acts: First, ECU tenoplasty and 3 months later UN transposition. Then, the same surgical procedure was performed on the contralateral limb.
Surgical technique
Ultrasound-guided bilateral infraclavicular block combined with general anesthesia is performed. The patient is operated in supine position.
ECU tenoplasty
Dorsal approach of the fifth and sixth compartments is performed. ECU tendon subsheath was weaker and thinner than normal. When flexing about 30 degrees the wrist in slight ulnar deviation and simultaneous rotating the forearm from neutral to full supination, the ECU tendon dislocated ulnarly leaving the ulnar groove and translated anteriorly. The abnormally thin and elastic tendon sheath stretched in this maneuver letting the tendon dislocate when tensed. An extensor retinaculum flap was made. ECU tendon was then lifted and the ulnar groove of the sixth compartment’s floor was deepened to give better support to the tendon. ECU was finally wrapped around the flap and attached above the fifth compartment using absorbable 2.0 bone anchors (Fig. 4). Adequate tendon stability was assessed through stress maneuvers. A wrist immobilization splint was used for protection during 6 weeks.
UN nerve transposition
Incision was done over the course of the nerve between the medial epicondyle and the olecranon. Special care was taken to identify and protect the medial brachial cutaneous nerve. UN dislocation was then addressed with flexion/extension of the elbow. Osborne’s ligament and the arcade of Struthers were incised, together with the deep flexor-pronator mass fascia. As ECU tendon in the wrist, the nerve dislocated anteriorly with a snap when the elbow flexion was more than 30 degrees. The Osborne ligament and retaining structures of the UN were thin and stretched. Once the nerve was released, anterior subcutaneous transposition was performed and maintained in its new position with a facial flap (Fig. 5). UN stability and proper gliding were assessed. The arm was immobilized in a sling during a 2-week period. The patient continued with paresthesia along with the UN territory for 3 weeks after UN transposition (dominant side); then, all neurological symptoms disappeared both at rest and during elbow motion. Two weeks after the procedure, the sling was removed, starting a rehabilitation protocol. At a 16-week follow-up, the patient had no clinical symptoms, with 0pain according to the VAS. Final Q-DASH score was 11 and m-ASES was 90 (excellent).
Discussion
Glycoprotein fibrillin-1 mutation (chromosome 15q21) is responsible for MS. This glycoprotein is an important component of the extracellular microfibrils. Despite the exact role of microfibrils remains unclear, these structures are found in a wide range of connective tissues and are vital for normal elastogenesis, elasticity, and homeostasis of the elastic fibers [8]. This finding explains patients’ joint laxity: Hyperextensible fingers, wrists, elbows, and knees [9]. Under stress conditions, ECU is involved in activities known as “loaded pronosupination tasks” such as turning a screwdriver, swimming, or draining cloth; particularly, when the wrist is loaded in full supination, extension, and ulnar deviation. In this situation, the only structure able to prevent ECU dislocation is the “ECU tendon subsheath.” This subsheath is a thin layer of collagen fibers in relation with the sixth extensor compartment; a fibroosseous tunnel that maintains the ECU moored in the dorsal sulcus of the distal ulna [10, 11]. Under normal circumstances, the ECU subsheath is a very strong structure able to neutralize ECUs dislocating force. Marfan’s syndrome weakens this collagen structure making it less effective for its supporting function. Although it was repaired and short-term results are acceptable, long-term follow-up is essential because the tissue might stretch again due to the basal syndrome. O’Driscoll [12] described the cubital tunnel retinaculum as a 4 mm wide band extending from the medial epicondyle to the olecranon, suggesting that this retinaculum was responsible for holding the UN in position. He classified this retinaculum according to anatomic variations and clinical implications: In type 0, the retinaculum is absent and the UN tends to dislocate, while in type 1, the retinaculum is “normal.” Whether the patient had a type 0 or a type 1 retinaculum, it seems that UN dislocation may happen more likely due to her MS condition and ligament weakness and stretching. The same thoughts regarding long-term results of tendon sheath reconstruction are to be considered when performing UN transposition and neurological symptoms improvement. Longer follow-up is needed to verify if standard techniques success in the presence of tissue collagen pathology.
Conclusion
Bilateral ECU and UN instability as a direct consequence of MS has not been reported in medical literature before. We strongly believe that connective tissue disorders present in MS could be responsible for this infrequent clinical presentation: The lack of ECU tendon subsheath efficiency and a deficient retinaculum at the cubital tunnel act as predisposing factors for ECU and UN instability.
Clinical Message
Bilateral ECU and UN instability should become suspicious of systemic connective tissue disorders. We ignore if standard treatment is successful in a long-term basis in these particular cases of collagen intrinsic pathology.
References
1. Allende C, Le Viet D. Extensor carpi ulnaris problems at the wristclassification, surgical treatment and results. J Hand Surg Br 2005;30:265-72.
2. Xarchas KC, Psillakis I, Koukou O, Kazakos KJ, Ververidis A, Verettas DA, et al. Ulnar nerve dislocation at the elbow: Review of the literature and report of three cases. Open Orthop J 2007;1:1-3.
3. Marfan A. Un cas de déformation congénitale des quatre membres, plus prononcée aux extrémités, caractérisée par l ́allongement des os avec un certain degré d ́amincissement. Bull Mem Soc Med Hop Paris 1896;13:220-6.
4. Yang RQ, Jabbari J, Cheng XS, Jabbari R, Nielsen JB, Risgaard B, et al. New population-based exome data question the pathogenicity of some genetic variants previously associated with marfan syndrome. BMC Genet 2014;15:74.
5. Tsang AK, Taverne A, Holcombe T. Marfan syndrome: A review of the literature and case report. Spec Care Dentist 2013;33:248-54.
6. Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, et al. The revised ghent nosology for the marfan syndrome. J Med Genet 2010;47:476-85.
7. Nelson AM, Walega DR, McCarthy RJ. The incidence and severity of physical pain symptoms in marfan syndrome: A survey of 993 patients. Clin J Pain 2015;31:1080-6.
8. McBride AR, Gargan M. Marfan syndrome. Curr Orthop 2006;20:418-23.
9. Grahame R, Pyeritz RE. The marfan syndrome: Joint and skin manifestations are prevalent and correlated. Br J Rheumatol 1995;34:126-31.
10. Taleisnik J, Gelberman RH, Miller BW, Szabo RM. The extensor retinaculum of the wrist. J Hand Surg Am 1984;9:495-501.
11. Salva-Coll G, Garcia-Elias M, Leon-Lopez MM, Llusa-Perez M, Rodríguez-Baeza A. Role of the extensor carpi ulnaris and its sheath on dynamic carpal stability. J Hand Surg Eur Vol 2012;37:544-8.
12. O’Driscoll SW, Horii E, Carmichael SW, Morrey BF. The cubital tunnel and ulnar neuropathy. J Bone Joint Surg Br 1991;73:613-7.
 |
 |
 |
 |
 |
| Dr. R N Brandariz | Dr. M O Abrego | Dr. J G Boretto | Dr. G L Gallucci | Dr. P De Carli |
| How to Cite This Article: Brandariz R N, Abrego M O, Boretto J G, Gallucci G L, P De Carli P. Atraumatic Bilateral Instability of Ulnar Nerve and Extensor Carpi Ulnaris in a Patient with Marfan’s Syndrome. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 3-6. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com