[box type=”bio”] Learning Point of the Article: [/box]
A high index of suspicion must exist when evaluating adult patients with clinical presentation of chronic neck pain, torticollis, or ‘cock robin’ head positioning, especially in the post-traumatic setting, to avoid overlooking the possible serious diagnosis of atlantoaxial rotatory subluxation.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 23-25 | Joseph Elsissy, Wayne Cheng, Andrew Kutzner, Olumide Danisa. DOI: 10.13107/jocr.2019.v09i05.1516
Authors: Joseph Elsissy[1], Wayne Cheng[1], Andrew Kutzner[2], Olumide Danisa[1]
[1]Department of Orthopedic Surgery, Loma Linda University, School of Medicine, Loma Linda, California, U.S.A,
[2]Department of Orthopedic Surgery, Grand Rapids Orthopedic Surgery Residency Grand Rapids, Michigan, U.S.A.
Address of Correspondence:
Dr. Joseph Elsissy,
Department of Orthopedic Surgery, Loma Linda University, 11234 Anderson St Westerly C, Loma Linda, California 92354 U.S.A.
E-mail: Jelsissy@llu.edu
Abstract
Introduction: Atlantoaxial rotatory subluxation (AARS) is an uncommonly encountered diagnosis within the adult population. The rare nature of this dislocation within the adult population often results in delayed diagnosis and treatment.
Case Report: A 30-year-old male presented following a low-speed motor vehicle accident. The patient had been involved in a work-related accident 1-year prior and had experienced fixed leftward gaze and tenderness of the cervical spine following this incident, but exhibited no focal neurologic deficits. Imaging demonstrated a Fielding Type 1 AARS of approximately 45°. The subluxation was reduced; and posterior C1–C2 instrumentation and fusion were performed, with no complications. Post-operative imaging revealed maintained reduction and alignment. The patient regained acceptable alignment and relief from his pre-operative symptoms.
Conclusions: Our case is an illustration of a chronic post-traumatic AARS in an adult patient with delayed diagnosis and definitive management. This diagnosis is rare within the adult population and is frequently overlooked. A high index of suspicion must exist when evaluating adult patients with clinical presentations of chronic neck pain, torticollis, or “cock robin” head positioning as delayed diagnosis.
Keywords: Atlantoaxial, subluxation, rotary, delayed.
Introduction
Atlantoaxial rotatory subluxation (AARS) is a rare diagnosis in the adult patient that is characterized by incomplete dislocation of the inferior atlantal and superior axial articular facets [1, 2, 3, 4]. Patients typically present in the characteristic “cock robin” position with associated painful torticollis. Due to its rarity, AARS is typically overlooked, often resulting in delayed diagnosis and treatment [3, 4, 5]. The current case is an illustration of delayed diagnosis and treatment of post-traumatic AARS in a 30-year-old male.
Case Report
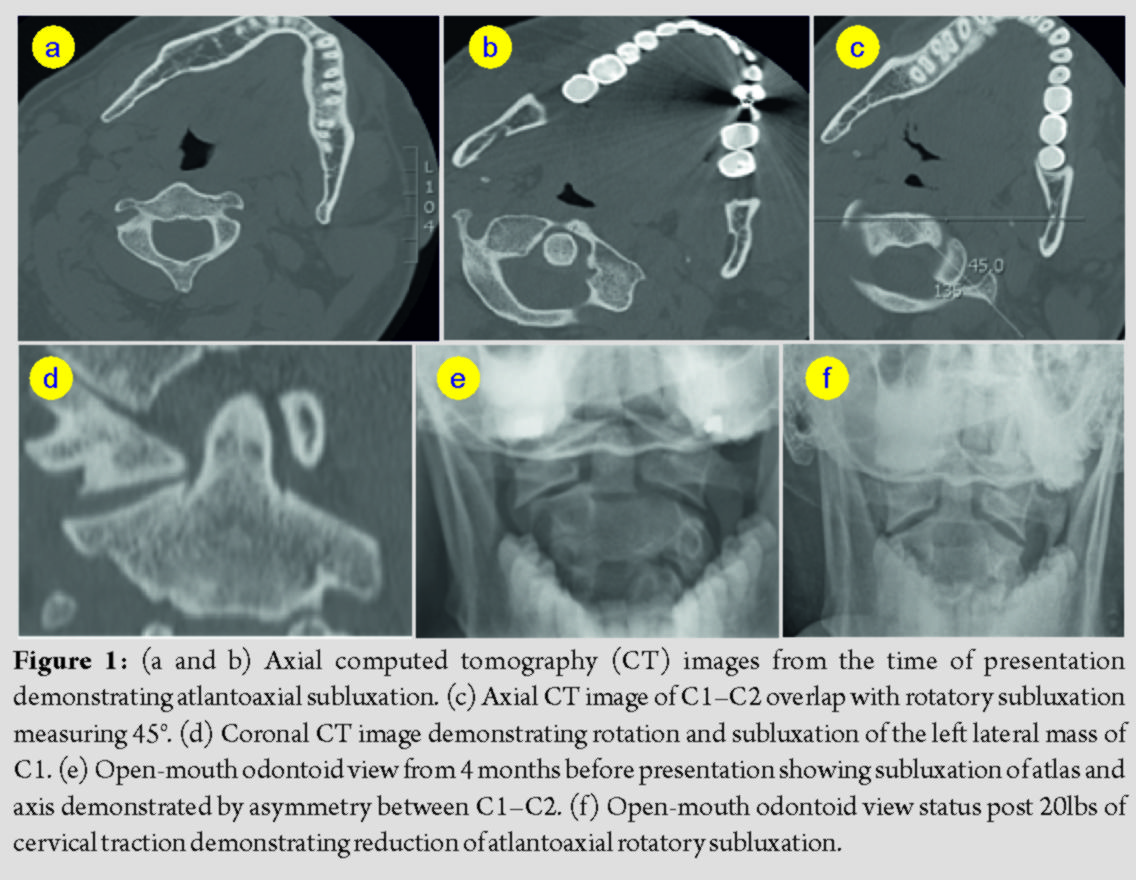
An otherwise healthy 30-year-old male self-presented to the emergency department after being involved in a low-speed traffic collision. He was seeking evaluation of acutely worsening neck pain that had been present for approximately 1 year. Physical examination demonstrated a fixed leftward gaze with midline tenderness about the cervical spine. There were no neurological deficits. He noted to our team that his gaze had been fixed and his neck had been painful for 1 year following a work-related accident. Computed tomography (CT) scan demonstrated a Fielding Type 1 AARS of approximately 45° (Fig. 1). A cervical spine X-ray from 4 months prior was obtained that also demonstrated subluxation of the atlantoaxial joint (Fig. 1). He was subsequently admitted and placed into 20 pounds of cervical traction with Gardner-Wells tongs. He was also started on oral benzodiazepines for muscle relaxation. Post-traction X-rays demonstrated reduction of the chronic subluxation (Fig. 1). The patient was maintained in cervical traction for 48 h and was then taken to the operating room where posterior C1–C2 instrumentation and fusion were performed undermaintained traction.
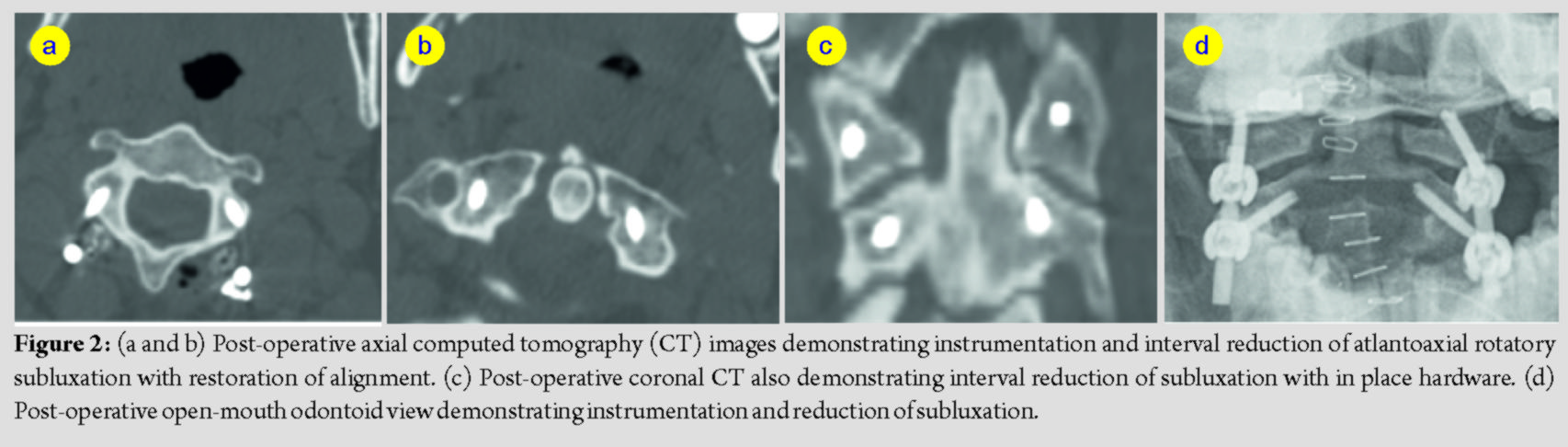
There were no complications related to the procedure. Post-operative CT and X-rays demonstrated maintained reduction and alignment of the atlantoaxial joint (Fig. 2). The patient regained normal head alignment and had relief from his pre-operative symptoms. He was discharged home from the hospital on post-operative day #6.
Discussion
Unlike children who are predisposed to AARSdue to large heads, underdeveloped musculature of the neck, and increased laxity of the joint capsule, adults will typically develop rotatory subluxation secondary to higher energy trauma [2, 3, 6]. Adult patients can also present after remote history of cervical trauma. Symptoms may include painful neck, torticollis, occipital neuralgia, and even vertebrobasilar insufficiency [6]. In addition, initial plain radiographs are exceedingly challenging to interpret for a variety of reasons and are often read as normal studies [7]. Therefore, a high index of suspicion must exist when evaluating adult patients with clinical presentations of chronic neck pain, torticollis, or “cock robin” head positioning as delayed diagnosis can result in catastrophic complications. Our case is an illustration of a chronic post-traumatic AARS in an adult patient with delayed diagnosis and definitive management.
Conclusion
AARS is a relatively uncommon diagnosis in the adult population. It can present acutely after significant trauma, and rarely, patients can present in delayed fashion after remote cervical injury as described in this case. It is critical to keep AARS in mind when assessing patients with neck pain and loss of motion. Proper history, examination, and imaging studies will often allow for diagnosis. Treatment can be done with either closed or operative measures and is decided on a case-to-case basis based on patient factors and severity of injury.
Clinical Message
It is a key to pay close attention to history and examination findings of patients presenting with symptoms of neck pain and stiffness, especially those with fixed posturing or loss of neck motion. Careful attention to imaging studies including plain radiographs and CT scan is critical to identification of AARS. Diagnosis allows the clinician to institute proper treatment with closed or operative measures, thus avoiding potentially serious complications related to AARS.
References
1. Missori P, Miscusi M, Paolini S, DiBiasi C, Finocchi V, Peschillo S, et al. A C1-2 locked facet in a child with atlantoaxial rotatory fixation. Case report. J Neurosurg 2005;103:563-6.
2. Neal KM, Mohamed AS. Atlantoaxial rotatory subluxation in children. J Am Acad Orthop Surg 2015;23:382-92.
3. Singh VK, Singh PK, Balakrishnan SK, Leitao J. Traumatic bilateral atlantoaxial rotatory subluxation mimicking as torticollis in an adult female. J Clin Neurosci 2009;16:721-2.
4. Jones RN. Rotatory dislocation of both atlanto-axial joints. J Bone Joint Surg Br 1984;66:6-7.
5. Maile S, Slongo T. Atlantoaxial rotatory subluxation: Realignment and discharge within 48 h. Eur J Emerg Med 2007;14:167-9.
6. Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am 1977;59:37-44.
7. Scapinelli R. Three-dimensional computed tomography in infantile atlantoaxial rotatory fixation. J Bone Joint Surg Br 1994;76:367-70.
 |
 |
 |
 |
| Dr. Joseph Elsissy | Dr. Wayne Cheng | Dr. Andrew Kutzner | Dr. Olumide Danisa |
| How to Cite This Article: Elsissy J, Cheng W, Kutzner A, Danisa O. A 30-year-old Male with Delayed Diagnosis and Management of Chronic Post-traumatic Atlantoaxial Rotatory Subluxation. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 23-25. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com