[box type=”bio”] Learning Point of the Article: [/box]
Giant cell tumor of the tendon sheath should be considered in the differential diagnoses of children presenting with soft tissues welling in the hand.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 63-66 | Samuel Grant, Qaisar Choudry. DOI: 10.13107/jocr.2019.v09i05.1536
Authors: Samuel Grant[1], Qaisar Choudry[1]
[1]Department of Trauma and Orthopaedics, East Lancashire Hospitals NHS Trust, Haslingden Rd, Lancashire, BB2 3HH, UK.
Address of Correspondence:
Dr. Samuel Grant,
Department of Trauma and Orthopaedics, East Lancashire Hospitals NHS Trust, Haslingden Rd, Lancashire, BB2 3HH, UK.
E-mail: samuel.grant@nhs.net
Abstract
Introduction: Giant cell tumor of the tendon sheath (GCTTS) is a benign tumor, originating from proliferation of the synovial cells of a tendon sheath. It is very rare within the pediatric population.
Case Report: In this case presentation, we describe two cases of GCTTS in the hand, in a 7-year-old female and a 6-year-old male.
Conclusion: GCTTS occurs very uncommonly in children. It is difficult to accurately diagnose on clinical examination and radiological investigation alone, and thorough and complete excision is important to avoid recurrence of the lesion. The two cases presented in this report help further define this condition, in terms of diagnosis and management, in the pediatric population.
Keywords: Giant cell tumor tendon sheath, hand, pediatric.
Introduction
Giant cell tumor of the tendon sheath (GCTTS) is a benign tumor, originating from the proliferation of the synovial cells of a tendon sheath [1, 2]. It is the second most common soft tissue tumor of the hand, after ganglion cyst [3, 4]. It tends to affect individuals between the third and fifth decades and is more common in women than men [5, 6].
GCTTS is rare within the pediatric population [1]. Here, we describe two cases of GCTTS, in a 7 years old and 6 years old child, respectively.
Case Report
Case 1
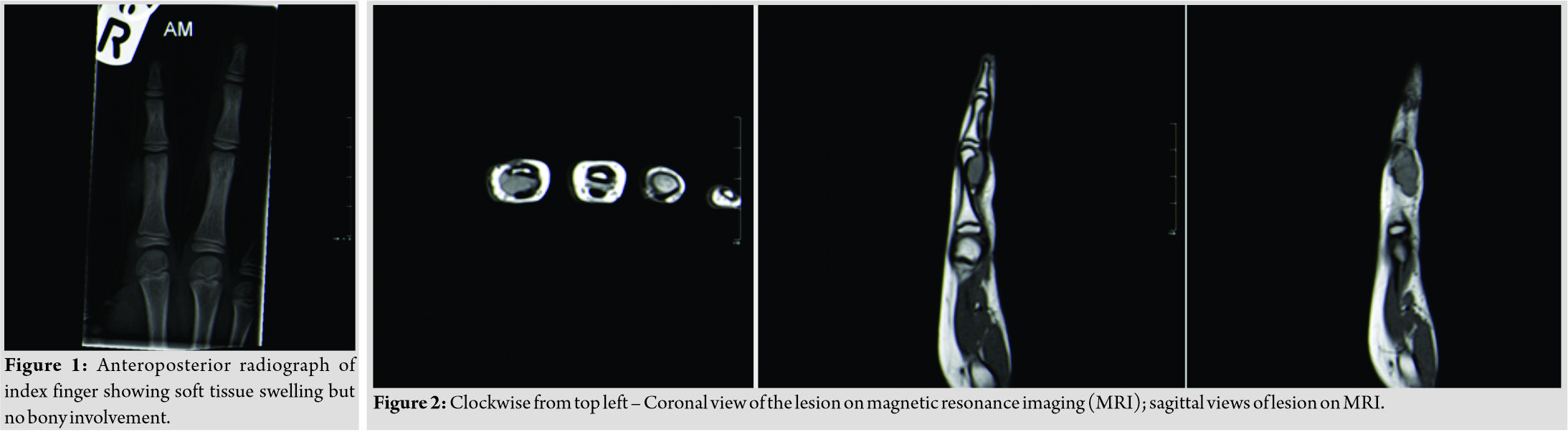
A 7-year-old female presented with 9-month histories of painless swelling of the right index finger proximal phalanx. She had no medical history of note. There was no skin tethering, and movement at the proximal interphalangeal joint was satisfactory and pain-free. Plain radiographs were obtained which showed soft tissue swelling but no bony involvement (Fig. 1). An ultrasound scan (USS) was arranged to assess the swelling. The USS was reported as showing a 16mm fluid-filled mass, diagnosed as a ganglion. The patient was subsequently seen a couple of months later with increased swelling, and magnetic resonance imaging (MRI) was undertaken (Fig. 2).
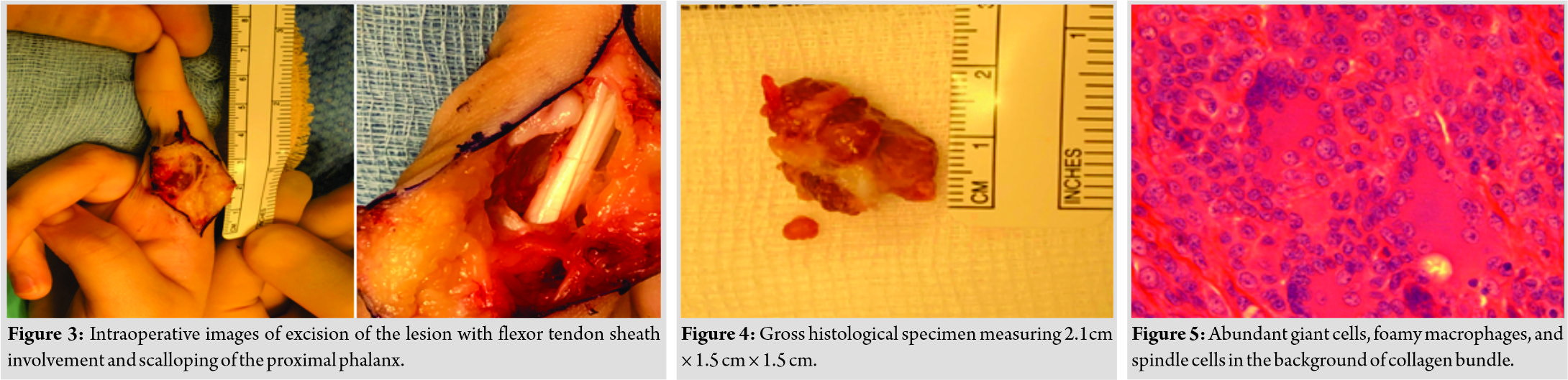
This was reported as showing a fluid-filled lesion at the radial aspect of the distal proximal phalanx, with dimensions of 2cm× 0.9cm× 0.9 cm. There was some interposition between the flexor tendon sheath and the proximal phalanx. It was again thought, that is, was most likely a ganglion. The lesion was initially managed conservatively; however, at 6-month follow-up, it was noted to have increased in size and was interfering with the patient’s ability to grip and hold pens/pencils. The patient was taken to theater for removal of the lesion. Intraoperatively, an extensive swelling was noted which enveloped the flexor tendon. Scalloping of the proximal phalanx was noted. A careful and thorough dissection was carried out with the use of magnification loupes, with subsequent flexor pulley reconstruction to allow easier flexor tendon excursion (Fig. 3).
Tissue samples were sent for histological analysis, measuring 0.4 × 0.3 × 0.3 cm and 2.1 × 1.5 × 1.5 cm (Fig. 4).
They were found to be composed of giant cells, foamy macrophages, and spindle cells in the background of collagen bundles in keeping with GCTTS. There was no evidence of mitoses or pleomorphism. Hemosiderin pigment was identified (Fig. 5). A wound check was carried out at 2 weeks postoperatively, with no issues noted. Further, 3 months and 1 year follow-up appointments were conducted, with no recurrence of the lesion and full return of function, with wounds having healed well.
Case 2
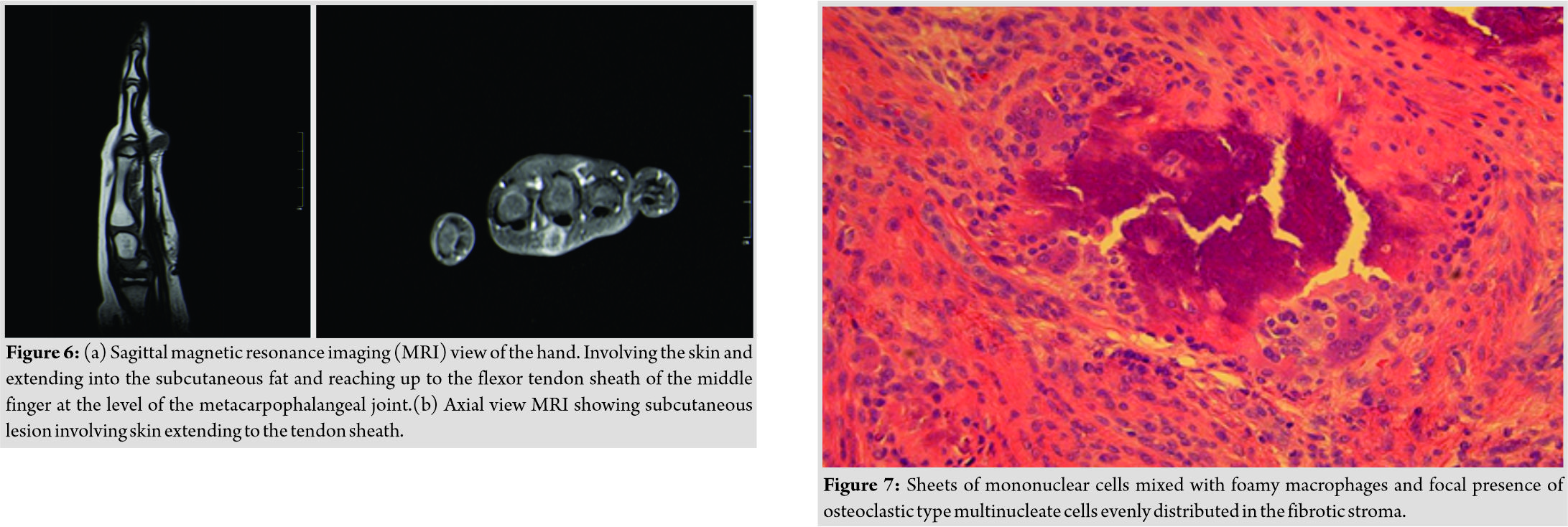
A 5-year-old male presented to the orthopedic clinic with a 1 year history of a gradually increasing swelling at the volar aspect of the right middle finger metacarpophalangeal (MCP) joint. The lesion was causing some discomfort and functional difficulties. Plain radiographs illustrated a soft tissue swelling adjacent to the heads of the index and middle finger metacarpals. MRI imaging was utilized to further define the lesion, which showed an enhancing lesion involving the skin, extending into the subcutaneous tissue and involving the flexor tendon sheath of the middle finger at the MCP joint (Fig. 6a and b). The reporting radiologist expressed doubt as to the proposed diagnosis of GCTTS, suggesting a differential diagnosis including granuloma annulare, hemangioma, and fibrocystic cytoma. The patient was taken for excision biopsy of the lesion, with the mass visualized and removed under magnification. Again macroscopic appearances suggested a diagnosis of GCTTS. Tissue samples obtained measured 1.4 × 1.4 × 1.3 mm. Histological examination showed a lobulated nodular lesion composed of sheets of mononuclear cells mixed with foamy macrophages and focal presence of osteoclastic type multinucleate cells evenly distributed in the fibrotic stroma. There was scattered hemosiderin pigment. The appearances were consistent with GCTTS (Fig. 7). As follow-up, wound checks were carried out at 2 weeks, with good healing noted. On further appointments at 3 months and 1 year postoperatively, the scar was healed, full function and range of movement were noted, and there was no sign of recurrence.
Discussion
GCTTS is known by a variety of alternate names including fibrous xanthoma, benign synovioma, and sclerosing hemangioma. Interestingly, there does appear to be some disagreement in existing literature regarding pigmented villonodular synovitis (PVNS) and its relation to GCTTS, beginning with if they are in fact distinct lesions, and how to distinguish them. Hulse and Watson case report includes PVNS as a terminological substitutefor GCTTS [7]. Occhipinti et al. suggest that PVNS is easily differentiated from GCTTS on histological examination [8] whereas Hwang et al. suggest that the lesions are histologically identical, distinguishable only by their location either in the joint or the tendon sheath, respectively [2]. GCTTS most often presents as a painless slow-growing mass of unknown etiology. It can occur in various locations, but is most frequently found in the hand or fingers. Although common in the adult population, the lesions are quite uncommon in children, especially those under 10 years old. In fact, the authors were able to find only one published report of an affected patient younger than the second case described in this report [9]. It is important to note that there was only 3-month history of swelling in the previously reported case; whereas the lesion in our case had been present much earlier. This illustrates GCTTS can occur from a very young age. The tumors usually appear radiologically as soft tissue shadowing with or without bone erosion, however, can exhibit degenerative or cystic changes [10]. In our first case, the mass was misdiagnosed as a ganglion cyst on both USS and MRI before surgical excision. In the second, it was thought unlikely to be GCTTS on MRI scan. This clearly illustrates the difficulty in accurately diagnosing GCTTS through radiological means alone. GCTTS can be classified macroscopically into tumors with, and without, a single pseudocapsule [4]. Although GCTTS is a benign mass, recurrence rates are high, with some studies reporting rates of between 25% and 45% [11]. This underlines the need for careful and thorough excision of lesions. A systematic review conducted by Fotiadis et al. identified a number of possible risk factors for recurrence [12], including location at the distal interphalangeal joint of the finger, poor surgical technique, osseous pressure erosion, cellularity/mitotic activity on histology, closeness to an arthritic joint, nm 23 negative tumors, and Type II tumors. During excision of both of the lesions presented in this case report, surgical loupes were used to ensure as complete excision of the lesions as possible. A pediatric case series conducted by Gholve et al. found the recurrence rate to be 0% which they suggested may be attributed to scrupulous excision with the aid of magnification equipment [13]. Neither of the patient cases reported here have encountered recurrence at the time of writing.
Conclusion
GCTTS is a benign lesion, which occurs very uncommonly in children. It is difficult to accurately diagnose on clinical examination and radiological investigation alone, and thorough and complete excision is important to avoid recurrence of the lesion. The two cases presented in this report help further define this condition in the pediatric population.
Clinical Message
Giant cell tumor of the tendon sheath is rare in children. These cases illustrate that it should be included in the differential diagnosis of children presenting with soft tissue swelling in the hand. They emphasize the importance of thorough investigation and careful excision of the lesion, to prevent recurrence.
References
1. Ueno T, Ansai S, Omi T, Kawana S. A child with giant cell tumor of tendon sheath. Dermatol Online J 2011;17:9.
2. Hwang JS, Fitzhugh VA, Gibson PD, Didesch J, Ahmed I. Multiple giant cell tumors of tendon sheath found within a single digit of a 9-year-old. Case Rep Orthop2016;2016:1834740.
3. Suresh SS, Zaki H. Giant cell tumor of tendon sheath: Case series and review of literature. J Hand Microsurg2010;2:67-71.
4. Al-Qattan MM. Giant cell tumours of tendon sheath: Classification and recurrence rate. J Hand Surg Br 2001;26:72-5.
5. Monaghan H, Salter DM, Al-Nafussi A. Giant cell tumour of tendon sheath (localised nodular tenosynovitis): Clinicopathological features of 71 cases. J Clin Pathol2001;54:404-7.
6. Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59:223-38.
7. Hulse N, Watson SJ. Giant cell tumour of tendon sheath in a child: A case report. Hand Surg 2005;10:97-100.
8. Occhipinti E, Heinrich SD, Craver R. Giant cell tumor of tendon sheath arising in the toe. Fetal PediatrPathol2004;23:171-9.
9. Stewart DA, Pedersen J, Coombs CJ. Giant cell tumour of tendon sheath in a 4-year-old boy. J Hand Surg Eur Vol 2014;39:889-91.
10. Karasick D, Karasick S. Giant cell tumor of tendon sheath: Spectrum of radiologic findings. Skeletal Radiol1992;21:219-24.
11. Kotwal PP, Gupta V, Malhotra R. Giant-cell tumour of the tendon sheath. Is radiotherapy indicated to prevent recurrence after surgery? J Bone Joint Surg Br 2000;82:571-3.
12. Fotiadis E, Papadopoulos A, Svarnas T, Akritopoulos P, Sachinis NP, Chalidis BE, et al. Giant cell tumour of tendon sheath of the digits. A systematic review. Hand (N Y) 2011;6:244-9.
13. Gholve PA, Hosalkar HS, Kreiger PA, Dormans JP. Giant cell tumor of tendon sheath: Largest single series in children. J PediatrOrthop2007;27:67-74.
 |
|
| Dr. Samuel Grant | Dr. Qaisar Choudry |
| How to Cite This Article: Grant S, Choudry Q. Giant Cell Tumor of Tendon Sheath in the Hand Affecting Children: Clinical and Radiological Findings, Histological Diagnoses and Treatment. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 63-66. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com