[box type=”bio”] Learning Point of the Article: [/box]
The presence of huge swelling around shoulder usually raises the suspicion of neoplastic lesion especially in elderly. However, even in the presence of massive swelling, a benign lesion like infection, cyst or bursitis should be considered in the differential diagnosis.
Case Report | Volume 9 | Issue 6 | JOCR November – December 2019 | Page 23-26 | Manoj Kashid, S K Rai, Barun Chakrabarty. DOI: 10.13107/jocr.2019.v09.i06.1572
Authors: Manoj Kashid[1], S K Rai[1], Barun Chakrabarty[2]
[1]Department of Orthopaedics, 151 Base Hospital, Guwahati, Assam, India,
[2]Department of Pathology, 151 Base Hospital, Guwahati, Assam, India.
Address of Correspondence:
Dr. Sanjay Kumar Rai,
Department of Orthopaedics, 151 Base Hospital, Guwahati, Assam, India.
E-mail: skrai47@yahoo.com
Abstract
Introduction: We report a rare case of massive subacromial bursitis in Rheumatoid Arthritis (RA) patient. A solid tumor was initially suspected because it was very large with no apparent local sign of inflammation or infection in a 69-year-old patient. Isolated subacromial bursa is an uncommon and it is usually small in size. This bursa usually does not enlarge enough to mimic a neoplastic lesion. The presence of huge swelling around shoulder usually raises the suspicion of neoplastic lesion. However, even in the presence of huge swelling, a benign lesion such as infection, cyst, or bursitis should be considered. This case report presents that even if swelling is huge, the benign lesion must be considered as a differential diagnosis of swelling around shoulder joint.
Case Report: We describe the clinical presentation, radiological investigations, and strategies for the management of a 69-year-old patient who was a known case of RA, and he was non-diabetic. Patient presented with massive swelling around shoulder for the past 6 years. We performed radiograms, a plain computed tomography, magnetic resonance imaging, a 99m Tc-MDP bone scintigram, and a 67Ga-citrate scintigram, which all indicated no evidence of tumor. It was treated by excision and no recurrence observed after 5 years.
Conclusion: Massive subacromial bursitis is rarely reported in medical literature. Even if swelling is massive, the benign lesion must be considered as a differential diagnosis of swelling around shoulder joint.
Keywords: Subacromial bursitis, rheumatoid arthritis, massive swelling.
Introduction
Synovial inflammation of the glenohumeral joint is common in Rheumatoid Arthritis (RA), and synovitis frequently extends to affect the rotator cuff and bursae of the shoulder joint give rise to swelling around shoulder joint [1, 2]. However, the massive involvement of a subacromial bursa without inflammation in the glenohumeral joints is rare [1, 3]. We encountered a RA patient with a massive subacromial bursitis that was initially suspected to be a solid neoplasm because of its clinical appearance. The final diagnosis was bursitis associated with RA.
Case Report
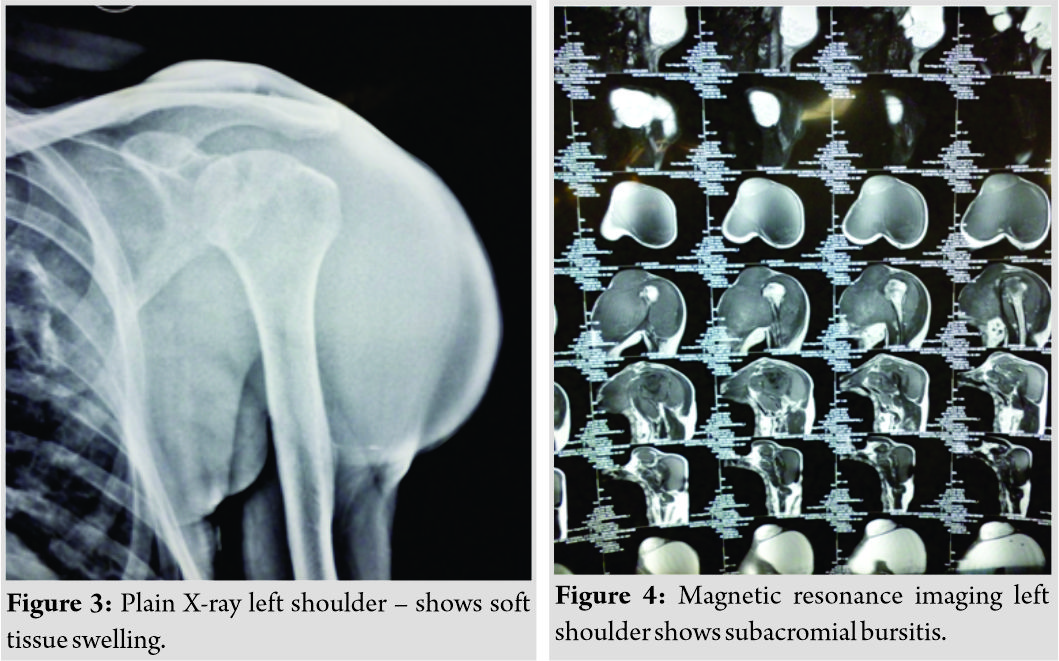
A 69-year-old patient reported to orthopedic outpatient department in February 2012 with huge swelling of the left shoulder. The swelling had first manifested in late 2005 spontaneous onset, but the patient had not sought treatment because there was no pain or restriction of shoulder function. This patient had been diagnosed with classical RA according to the revised diagnostic criteria of RA about 19 years ago and was Steinbrocker’s Stage I, Class 2 [4]. Physical examination on palpation revealed a marked soft to firm non-tender soft tissue swelling on the anterolateral aspect of the shoulder joint (Fig. 1 and 2).
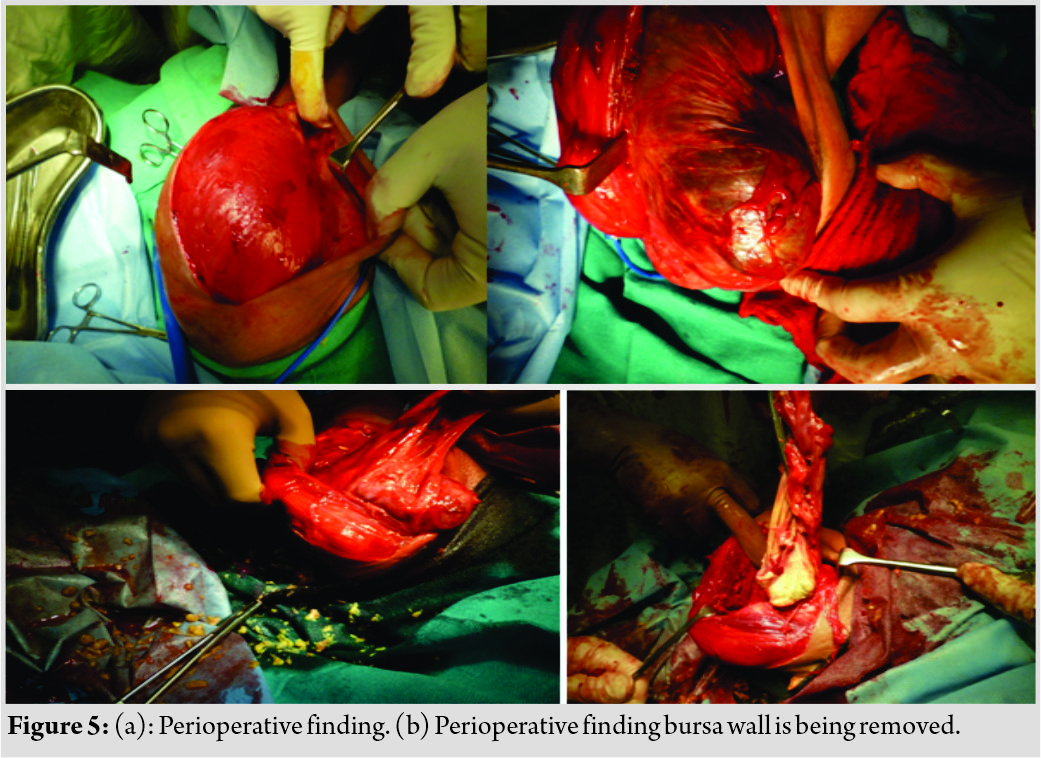
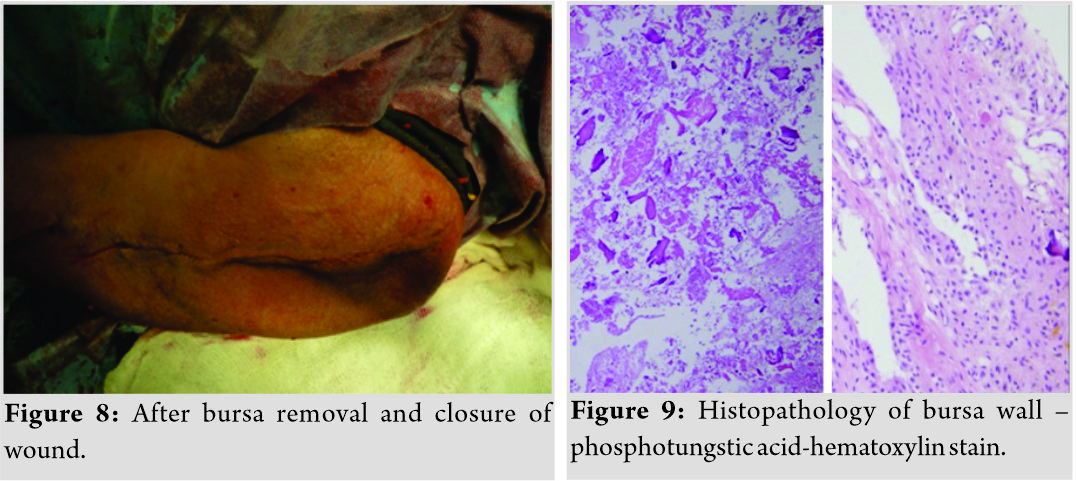
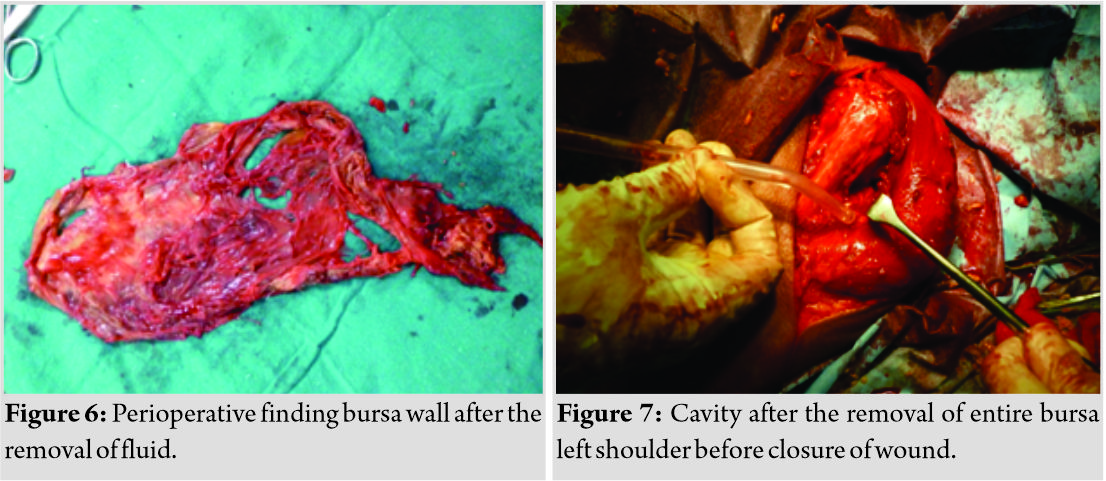
The patient was treated by surgical exploration on February 20, 2012, based on a clinical diagnosis of subacromial bursitis in RA. After pre-anesthesia checkup, the patient was operated under general anesthesia in supine position. After the tight and expanded bursal roof was incised, rice body like material and straw-colored fluid came out (Fig. 5a and b). All of these substances were removed and the bursectomy was completed. The excised bursa measured approximately 25 cm × 9 cm (Fig. 6). Macroscopically, no villous formation was seen in the bursal membrane. In addition, inspection of the glenohumeral joint through the rotator interval appeared normal. Wound was lavaged and finally closed (Fig. 7 and 8).
Results
The patient has full range of motion and followed up for 4 years. At the end of 5 years, he does not show any recurrence.
Discussion
Subacromial or deltoid bursitis is usual complication of RA generally occurs in association with scapulohumeral arthritis. The other common etiologies include Subacromial impingement, Subacromial hemorrhage, Repetitive overhead activities, direct trauma, crystal deposition, gouty bursitis and Infection are also common. There is communication between the two cavities due to perforation of the rotator cuff. There have been few reports of isolated involvement of the subdeltoid bursa [5, 6]. However, subdeltoid bursitis as a presenting manifestation of Rheumatoid disease is rare. The formation of intra-articular rice bodies was first described in tuberculous arthritis; however, it appears to be a common finding in RA and bursitis as well [7, 8]. The presence of rice bodies in bursal in RA was described by Doury et al. [9] and Watanabe et al. [6]. Subacromial Rheumatoid bursitis may presents with a painful arc syndrome, but marked swelling of the shoulder is the most unusual and rare presenting symptom. The condition is of course, treated surgically. This allows the removal of the loose bodies, resection of the lining of the bursa, and pathologic examination of the synovial membrane. The size of subacromial bursa is usually small but sometimes it presents as huge swelling mimic neoplasm as reported by Minoru Yoneda et al., in 2001 [10]. It may also present as a swelling filled with multiple rice body, a rare presentation of chronic subacromial bursitis secondary to extensive underlying RA, seronegative inflammatory arthritis or tuberculous joints as noted by Joshi [11], and similar presentation was also noted by Bacha et al. [12]. In a separate study by Krishnamoorthy, he was found to have giant-cell tumor of the supraspinatus tendon sheath, which was the cause of swelling and pain along with impingement of shoulder. Takayama et al., in 2000, reported a swelling around shoulder join that mimics soft tissue tumor [13].
Conclusion
The subacromial bursa usually does not enlarged enough in RA to mimic a neoplastic lesion. The presence of huge swelling around shoulder usually raises the suspicion of neoplastic lesion, especially in the elderly. However, even in the presence of huge swelling, a benign lesion such as infection, cyst, or bursitis should be considered. This case report presents that even if swelling is massive, the benign lesion must be considered as a differential diagnosis of swelling around shoulder joint.
Clinical Message
The presence of massive swelling around shoulder usually raises the suspicion of neoplastic lesion, especially in the elderly. However, even in the presence of massive swelling, a benign lesion such as infection, cyst, or bursitis should be considered in the differential diagnosis.
References
1. Sbarbaro JL. The rheumatoid shoulder. Orthop Clin North Am 1975;6:593-6.
2. Booth RE Jr., Marvel JP Jr. Differential diagnosis of shoulder pain. Orthop Clin North Am 1975;6:353-79.
3. Steinbrocker O. In: Hollander JL, McCarty DJ, editors. The Painful Shoulder, Arthritis and Allied Conditions. 8th ed. Philadelphia, PA: Lea and Febiger; 1972. p. 1467.
4. Steinbrocker O, Traeger CH, Batterman RC. Therapeutic criteria in rheumatoid arthritis. J Am Med Assoc 1949;140:659-62.
5. Huston KA, Nelson AM, Hunder GG. Shoulder swelling in rheumatoid arthritis secondary to subacromial bursitis. Arthritis Rheum 1978;21:145-7.
6. Watanabe S, Kawakita Y, Tatsuzawa Y, Yoshioka K, Kubo T. Case of rheumatoid arthritis with the inflamed subdeltoid bursa containing 923 rice bodies With special reference to the development of rice bodies. Ryumachi 1983;23:206-11.
7. Wynne-Roberts CR, Cassidy JT. Juvenile rheumatoid arthritis with rice bodies: Light and electron microscopic studies. Ann Rheum Dis 1979;38:8-13.
8. Albrecht M, Marinetti GV, Jacox RF, Vaughan JH. A biochemical and electron microscopy study of rice bodies from rheumatoid patients. Arthritis Rheum 1965;8:1053-63.
9. Doury P, Delahaye RP, Rochat G, Thabaut A, Pattin S, Durosoir JL, et al. Les bursites de 1’Cpaule au cours de la polyarthrite rhumatoide: A propos d’une observation. Ann Med Interne (Paris) 1977;128:745-9.
10. Yoneda M, Wakitani S, Yamamoto T. Huge tumor-like subacromial bursitis associated with rheumatoid arthritis. Mod Rheumatol 2001;11:255-8.
11. Joshi PS. Severe sub-acromial bursitis with rice bodies in a patient with rheumatoid arthritis: A case report and review of literature. Malays Orthop J 2018;12:52-5.
12. Bacha R, Manzoor I, Gilani SA. Sonographic presentation of rice bodies in subacromial-subdeltoid chronic bursitis. Ultrasound J 2019;11:16.
13. Krishnamoorthy VP, Jacob KM, Poonnoose PM. Giant cell tumor of the supraspinatus tendon sheath causing shoulder impingement. Int J Shoulder Surg 2012;6:23-4. 13. Takayama A, Ito H, Shirai Y. Subacromial bursitis mimicking a soft tissue tumor. J Shoulder Elbow Surg 2000;9:72-5.
 |
 |
 |
| Dr. Manoj Kashid | Dr. S K Rai | Dr. Barun Chakrabarty |
| How to Cite This Article: Kashid M, Rai S K, Chakrabarty B. Rare Presentation of Subacromial Bursitis Mimics Neoplasm in a Case of Rheumatoid Arthritis. Journal of Orthopaedic Case Reports 2019 Nov-Dec;9(6): 23-26. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com